The purpose of this article is to outline key technical considerations in the performance of total hip arthroplasty after common osteotomies of both the proximal femur and acetabulum. Attention is called to anatomic variation, both innate and incurred. After a femoral osteotomy, specific focus should be placed on incision selection, residual hardware management, abductor handling, and proper version establishment. After a periacetabular osteotomy, similar concern should be granted to cup position and fixation. Results of total hip arthroplasty after common osteotomies are also reviewed and importance of these issues highlighted.
- •
Be prepared for broken hardware.
- •
Removal of extensive hardware can be avoided with proper implant selection.
- •
A staged approach for hardware removal before total hip arthroplasty (THA) is sometimes prudent.
- •
Critically assess the position of the greater trochanter preoperatively, so that a required osteotomy can be appropriately planned.
- •
Assess the femoral version preoperatively so that modular stems may be used if required.
- •
Recognize and prepare for femoral deformity that often accompanies acetabuli that have previously undergone an osteotomy.
- •
Be mindful of a retroverted socket after a previous acetabular osteotomy and plan accordingly.
- •
Overmedialization of the acetabulum may warrant additional fixation at the time of arthroplasty.
Introduction
Hip preservation surgery is often used to relieve pain and correct osseous deformity that would otherwise predispose patients to early-onset arthritis. Osteotomies of the proximal femur and acetabulum are performed in this setting to negate or, more commonly, prolong a patient’s need to undergo a THA. Osteotomies are usually performed to address deformities of a congenital or developmental etiology; however, they are also used to address traumatic deformities, either during an initial presentation or in the treatment of nonunions/malunions. Osteotomies are also occasionally performed in the setting of avascular necrosis (AVN) and some other less common indications.
Despite a well-performed osteotomy and regardless of the impetus for its performance, a subsequent THA is sometimes required for progression of coxarthrosis. Previously performed osteotomies warrant deliberation in preoperative planning and patient counseling before conversion to an arthroplasty. The purpose of this article is to outline key technical considerations in the performance of THA after common osteotomies of both the proximal femur and acetabulum. Attention is called to retained hardware and anatomic variation, both innate and incurred.
THA after femoral osteotomy
Technical Pearls
Overview
Femoral osteotomies have been performed for a variety of indications, including but not limited to, congenital/developmental dysplasia, AVN, treatment of femoral neck fractures, treatment of proximal femoral nonunions/malunions, and osteoarthritis. In most instances, these osteotomies are performed through the intertrochanteric region of the proximal femur to produce a more varus or valgus hip alignment, although purely rotational osteotomies may also be performed to alter the weight-bearing portion of the femoral head. Irrespective of the indication for femoral osteotomy, key technical considerations for subsequent THA include incision selection, hardware removal, abductor condition, femoral version, and femoral offset.
Incision selection
Most incisions for a varus-producing or valgus-producing osteotomy are longitudinal and centered over the greater trochanter. In these cases, the incision for an anterolateral, direct lateral, or posterior approach to the hip usually incorporates and uses the previous incision. In a series of 215 THAs after failed trochanteric osteotomies, the ideal arthroplasty incision was compromised in fewer than 5% of cases. A direct anterior approach may be performed based on surgeon preference; however, this generally requires a separate incision for hardware removal. These incisions should be appropriately spread to allow for a skin bridge of at least 6 cm. If a horizontal incision is encountered over a favored approach site, this should be crossed at an angle greater than 40° to prevent ischemic necrosis of skin edges.
Hardware removal
The majority of femoral osteotomies are secured with internal fixation. In the previously cited series of 215 hips, 211 were fixed with internal hardware, and 72% of patients underwent hardware removal at the time of their arthroplasty. The need for hardware removal at the time of arthroplasty may alter the choice of surgical approach, particularly if a surgeon’s preference is normally directly anterior. It can also add to the length of the arthroplasty procedure, thereby incurring added risk for infection. This can be compounded if a surgeon is not prepared to deal with broken hardware or screws that have been stripped. It is wise to have a broken screw set available, as well as burs and potentially trephines, in addition to the appropriate hardware extraction set as identified in previous operative notes. Ferguson and colleagues noted difficulty during hardware removal in 24% and breakage of implants at the time of removal in 21% in his series of 215 hips.
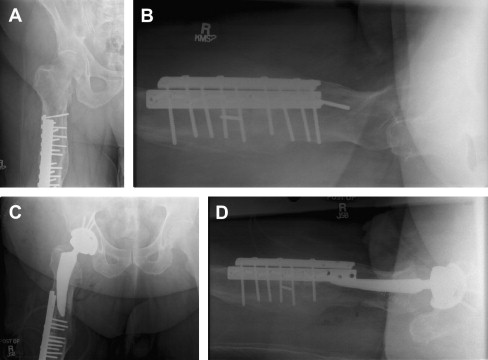
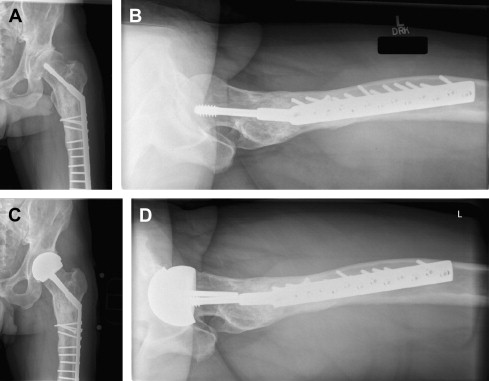
The length of fixation along the femoral shaft may also play a role in implant selection. If all the hardware is to be removed, an implant should be selected that bypasses any residual stress risers created by screw removal. Conversely, a carbide bur may be used to cut a plate short so that only the proximal portion is removed with subsequent implantation of a shorter femoral stem and retention of a portion of distal hardware ( Fig. 1 ). The latter technique may allow for a less-extensive soft tissue insult. On rare occasions, removal of the existing hardware incurs such a grievous insult to a patient’s soft tissues or bone stock that a hip resurfacing prosthesis proves the most beneficial option, because all the femoral hardware may be retained ( Fig. 2 ).
Empty screw holes also may increase the rate of intraoperative fracture by serving as a stress riser during femoral preparation. Great care should be taken during rasping, broaching, and reaming under these circumstances. In cases of cemented femoral fixation, empty screw holes may also compromise a surgeon’s ability to adequately pressurize the canal. This may lead to a poorer cement mantle and a subsequently increased rate of mechanical failure over time.
A staged approach to hardware removal and THA is another option in the treatment of these patients. Tissue cultures at the time of hardware removal should be obtained routinely. Ferguson and colleagues reported that 28 of 290 patients had positive intraoperative cultures despite absence of any other data to suggest an active infection. If an ongoing infection is detected, it can be treated before THA. Conversely, if tissue cultures are negative, then surgeons are afforded a greater degree of aseptic certainty during subsequent THA.
Abductor mechanism considerations
The position of the greater trochanter is often altered significantly after a proximal femoral osteotomy. If the resultant position of the trochanter overhangs the entry point to the femoral canal, it can complicate stem insertion. Boos and colleagues noted a significant increase in the need for trochanteric osteotomy during THA after a proximal femoral osteotomy compared with a primary THA control group. The position of the trochanter also needs to be critically gauged with respect to the final tension of the abductors during trialing and after component insertion. The abductors may be long compared with the offset afforded by the femoral implant, especially in circumstances where a calcar-replacing implant is required. A trochanteric advancement should be considered in these instances to improve hip stability.
Femoral version
Rotational alterations performed during an osteotomy vary the normal version of the proximal femur and may obscure the normal bony landmarks often used by surgeons during stem placement. Evaluating the combined version during component trialing can be used as a surrogate assessment of the femoral version when the cup position and acetabular landmarks are more reliable. Often the femoral component needs to be placed in a position of relative retroversion compared with the modified anatomy observed in the previously osteotomized femur. This can be attempted with standard uncemented implants; however, if stable interference fit cannot be achieved, then a smaller stem can be cemented in relative retroversion to “cheat” the patient’s anatomy. Modular uncemented stems, which pair a proximal metaphyseal fitting sleeve and a distal fluted stem, allow for any degree of selected version and are a powerful tool for addressing this deformity. The use of intraoperative radiographs to assess component position is another means of providing feedback to surgeons and helps ensure operative success.
Results
THA after a proximal femoral osteotomy is usually performed in a younger more active population than standard primary THA. In the studies reviewed, the average time from a varus/valgus-producing osteotomy until conversion to a total hip varied from 7.3 to 12.4 years in patients with mean ages between 50 and 61 years. Rotational osteotomies had a shorter survivorship and were converted between 1.7 and 4 years in patients with mean ages between 40 and 43 years. The higher demand this patient population imposes on their components has affected reported results with early stem designs and implantation techniques. Historical results with cemented stems, using first-generation and second-generation cementation techniques, demonstrated a higher complication rate and a greater degree of procedure difficulty compared with standard primary THA. Ferguson and colleagues noted a 19.5% mechanical failure rate of cemented stems, with a 12% stem revision rate at 10-year average follow-up. This series also highlighted a 25% complication rate, technical difficulty in 23% of patients, and an overall aseptic revision rate of 15%. Another study, performed by Boos and colleagues, noted a trend of decreased survivorship (82% vs 90%) in a group of 74 cemented THAs after a proximal femoral osteotomy compared with a control group of 74 cemented standard primary THAs at follow-up between 5 years and 10 years. This series also noted a significant increase in technical demand and longer procedure times in the postosteotomy group. Both of these studies, however, pointed out a significant improvement in hip scores after the THA procedure.
Results of THA after proximal femoral osteotomy improved dramatically with newer implant designs and a shift toward greater reliance on uncemented instrumentation techniques. Breusch and colleagues reported 10-year results of 44 uncemented stems implanted after failed intertrochanteric osteotomy and a 96% survivorship rate when aseptic loosening was selected as the endpoint. They concluded that this was comparable to patients with normal anatomy undergoing a standard primary THA. They noted 2 fissures that occurred during instrumentation, but these did not require any further treatment. Another more recent study investigating 30 uncemented THAs performed after failed valgus osteotomy in the setting of acetabular dysplasia demonstrated a stem survivorship of 100%. Eleven of these patients received modular stems that allow for version variability, with the remainder receiving monoblock stems (with modular femoral head sizing). The investigators noted cortical hypertrophy at the tip of 6 monoblock stems and concluded that, secondary to this radiographic finding and the ease of addressing version abnormalities, modular stems should be preferentially used in this patient population.
THA after rotational osteotomy has also been evaluated in isolation. Kawasaki and colleagues compared THA after rotational osteotomy for AVN to primary THA for AVN. At midterm follow-up, there were no differences in Harris hip scores, radiographic loosening, or survivorship between groups. In a similar subsequent study by Lee and colleagues comparing postrotational osteotomy THA with standard primary THA, the investigators noted a higher percentage of malpositioned femoral stems with respect to varus/valgus alignment. Acetabular cups in the conversion group were also found to have a greater chance of being underanteverted and underabducted. This study failed to correlate these findings with differences in clinical outcomes, however.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







