Talus Fractures: Open Reduction Internal Fixation
Paul T. Fortin
Patrick J. Wiater
Talus fractures are uncommon, and most surgeons have limited experience within the management of this challenging injury. These fractures usually occur as the result of high-energy trauma, which often produces fracture comminution, displacement, and soft-tissue injury. The long-term consequences following a talus fracture can be devastating often leading to significant lower extremity impairment.
Two-thirds of the talus is covered in articular cartilage, and all fractures are articular injuries affecting one or more of the adjacent joints. The talus is divided into three major parts—head, neck, and body. The body of the talus has five articular surfaces: superior, lateral, medial, posterior, and inferior. The neck of the talus has multiple vascular foramina distributed along its longitudinal axis, which may compromise its strength by increasing porosity making it more vulnerable to fracture. The head of the talus rests in a deep socket, similar to the acetabulum, formed by the navicular, the anterior and middle calcaneal facets, the calcaneonavicular component of the bifurcate ligament, superomedial calcaneonavicular ligament, and the plantar calcaneonavicular ligaments. The relative displacements of the talar head, calcaneus, and navicular with weight bearing are accommodated by the flexibility of this articulation that can adapt in form and size.
The extraosseous blood supply to the talus comes from three main arteries and their branches. These arteries, in order of significance, are the posterior tibial, anterior tibial, and perforating peroneal (Fig. 34.1). The artery of the tarsal canal (branch from the posterior tibial) and the artery of the tarsal sinus (perforating peroneal and anterior tibial) form an anastomotic sling on the inferior neck of the talus. The main blood supply to the talus is from the artery of the tarsal canal, which supplies the majority of the talar body. The posterior tibial artery also provides anterograde flow through branches that penetrate the posterior tubercle of the talus. The anterior tibial and the artery of the tarsal sinus supply the head and neck regions. Extensive intraosseous anastomoses within the talus may contribute to its survival in complex fractures. Initial fracture displacement is believed to be the most important factor affecting talar blood supply. Soft-tissue handling at the time of surgery also plays an important role, and every effort should be made to preserve the deltoid ligament attachment on the talus and avoid excessive soft-tissue stripping.
Because of the highly variable nature of talus fractures, classification of these fractures is difficult. Talar neck fractures are classified into one of four types based upon initial fracture displacement and involvement of adjacent joints (Fig. 34.2). The classification for fractures of the talar neck is based upon the radiographic appearance at the time of injury. One important distinguishing characteristic among talar neck fracture types is that type I fractures are truly nondisplaced. Any displacement is significant and precludes classification as a type I injury. Hawkins type II fractures involve a talar neck fracture with subluxation or dislocation of the subtalar joint. Hawkins type III fractures are characterized by a fracture of the neck with displacement of the body of the talus from the tibiotalar and subtalar joints. Over half of type III fractures are open and are often associated with neurovascular and/or skin tissue compromise. Type IV injuries involve subluxation or dislocation of the ankle, subtalar, and talonavicular joints.
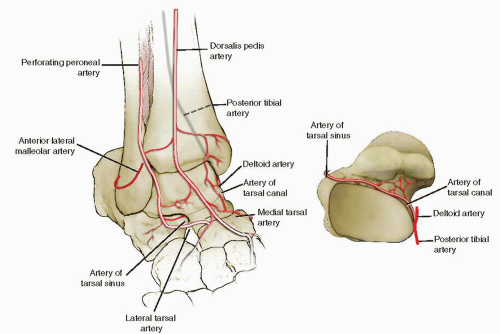 FIGURE 34.1 The talus receives its blood supply from all three main arteries perfusing the foot. The posterior tibial artery is the main contributor to talar body blood supply. |
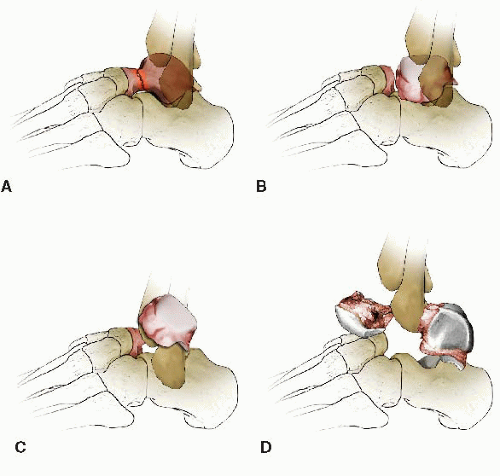 FIGURE 34.2 Hawkins classification of talar neck fractures. A. Type I. B. Type II. C. Type III. D. Type IV. |
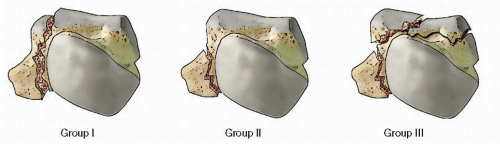 FIGURE 34.3 Talar body fractures. A. Group I cleavage fractures (horizontal, sagittal, coronal). B. Group II process or tubercle fractures. C. Group III crush with compression/impaction. |
Talar body fractures can be classified into cleavage, crush, tubercle, or process fractures (Fig. 34.3). The Marti-Weber classification system is less-commonly used but is a more comprehensive classification system that incorporates nearly all types of talus fractures: type I fractures include talar head, process, and osteochondral fractures. Type II fractures are nondisplaced head and neck fractures. Type III fractures include displaced neck and body fractures with subluxation of either the ankle or subtalar joint. Type IV fractures are displaced neck or body fractures with complete dislocation of the body as well as major crush injuries to the talus.
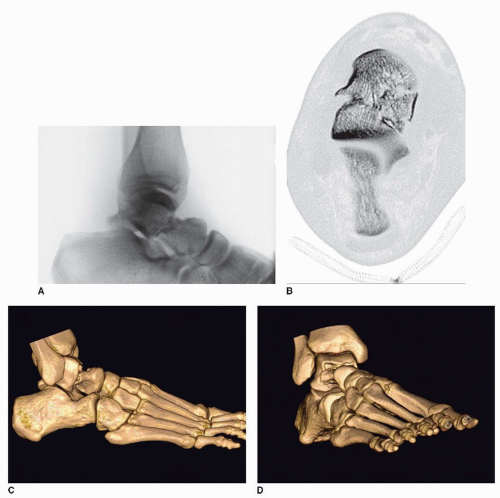
Unless substantially displaced, talus fractures are often difficult to visualize on plain radiographs and uncommonly go unrecognized particularly in multiply injured patients (Fig. 34.4A-D). The late treatment of missed talar injuries often results in suboptimal outcomes giving increased importance to initial diagnosis and treatment. Of the bones in the foot and ankle, the talus is the most common site of missed injuries. Occult talar injuries should always be suspected when swelling and ecchymosis of the foot and ankle are present, even when radiographics appear normal.
INDICATIONS AND CONTRAINDICATIONS
Although implants for talus fracture fixation have been improved over the last decade to smaller more site-specific designs, the principles of fracture management are the same. Displaced fractures require internal fixation. Operative treatment is usually necessary to restore joint congruity and hindfoot mechanics. Disruption of articular congruity and/or loss of talar length, alignment, and rotation are strong indications for operative treatment. Even small amounts of fracture displacement can result in a significant compromise of subtalar, ankle, or talonavicular function.
There are five major types of talus fractures: talar head, neck, body, process or tubercle, and osteochondral fractures, and each type has site-specific indications for operative treatment. In general, talar neck and body fractures should be treated operatively if the fracture is displaced more than 1 to 2 mm. The magnitude of displacement is often difficult to properly evaluate with plain x-rays alone, and additional imaging studies such as computed tomography (CT) scanning are typically required. Nonoperative treatment can be employed in a few fractures that are displaced 1 mm or less. Some authors advocate operative treatment of even nondisplaced talar neck and body fractures to allow early range of motion or prevent late fracture displacement. All open fractures as well as fracture dislocations of the neck/body require immediate operative intervention. Regardless of fracture type, talar neck and body fractures that result in skin compromise from fracture displacement should be treated promptly with either an attempt at closed reduction or operative reduction and fixation to minimize the risk of soft-tissue necrosis. Displaced talar neck and body fractures without joint dislocation, compromised skin, and/or neurovascular compromise can safely be treated in a delayed fashion, usually within 24 to 48 hours.
Talar head fractures are often associated with disruption of the talonavicular joint and operative reduction and fracture fixation are necessary to restore function to the joint (Fig. 34.5A-C). There are two types of talar head fractures: shear fractures and compression or impaction fractures. Shear fractures may involve a locked dislocation of the talonavicular joint where the fractured talar head becomes perched on the lateral portion of the navicular. Failure to recognize and properly reduce these injuries can lead to permanent loss of midfoot and hindfoot function. The other type of talar head injury is an impaction fracture usually in the medial portion of the head. Minor degrees of compression are difficult to repair and should be treated nonoperatively. Larger areas of talar head compression may benefit from elevation of the compressed region with bone grafting to restore articular congruity. It is important to remember that talar head fractures can occur simultaneous with lateral column injuries such as calcaneal or cuboid fractures, which may also need to be addressed.
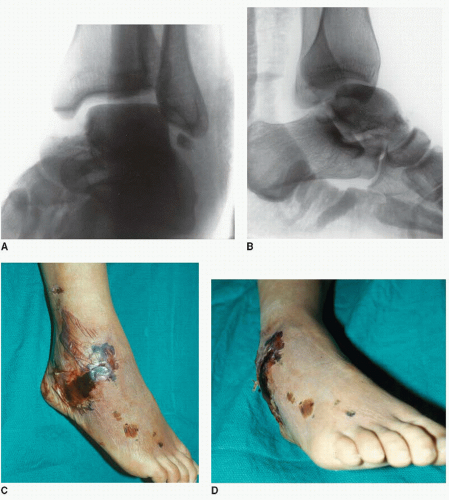 FIGURE 34.4 A,B. AP and lateral x-rays of a displaced talar neck fracture. C,D. Clinical photos of the same patient 3 days later with soft-tissue compromise and impending full-thickness necrosis because of a delay in diagnosis and failure to perform a timely reduction. (Copyright 2001 American Academy of Orthopaedic surgeons, reprinted with permission from Fortin PT, Balazsy JE. Talus fractures: evaluation and treatment. J Am Acad Orthop Surg 2001;9(2):114-127. |
Talar process or tubercle fractures typically involve the lateral talar process or posterior process (medial and/or lateral tubercle). They can occur as an isolated injury or in combination with a talar body or neck fracture. Although seemingly innocuous injuries, they often involve significant portions of articular cartilage and can compromise ankle and/or subtalar joint stability if unrecognized. When these fractures are displaced and/or compromise a significant portion of the articular surface, they should be treated surgically. This typically involves open reduction and internal fixation but fragment excision may be appropriate if the fragment is small or when comminution exists.
Osteochondral fractures of the talar dome can occur in conjunction with talar body fractures or as an isolated entity. Acute displaced osteochondral fractures most commonly involve the anterolateral area of the talar dome and can encompass significant portions of the dome with varying degrees of displacement. Large displaced osteochondral fragments should be treated surgically with either fixation or excision depending upon the size or amount of comminution.
Significant neuropathy, peripheral vascular disease, soft-tissue compromise, and limited ambulatory capacity are relative contraindications to surgical management. Peripheral neuropathy is highly variable
in severity, and many elderly patients have some degree of peripheral neuropathy that should not preclude operative treatment. Loss of protective sensation, however, as judged by the ability to differentiate a 5.07 monofilament, is a sensitive indicator of significant neuropathy; therefore, failure to differentiate the monofilament should be considered a relative contraindication to surgery. Even in patients with loss of protective sensation, the decision to operate depends upon the fracture pattern, ankle stability, and presence of dislocation or significant joint subluxation and should be made on a case-by-case basis. A minimally displaced talar body fracture in a patient with significant neuropathy may be best treated nonoperatively, whereas a Hawkins III talar neck fracture with posteromedial extrusion of the talar body should be treated surgically to relieve soft tissue and/or neurovascular compromise regardless of the presence of neuropathy. Elderly patients with limited ambulatory capacity, similarly, may be best treated nonoperatively if the joint is not significantly displaced or dislocated.
in severity, and many elderly patients have some degree of peripheral neuropathy that should not preclude operative treatment. Loss of protective sensation, however, as judged by the ability to differentiate a 5.07 monofilament, is a sensitive indicator of significant neuropathy; therefore, failure to differentiate the monofilament should be considered a relative contraindication to surgery. Even in patients with loss of protective sensation, the decision to operate depends upon the fracture pattern, ankle stability, and presence of dislocation or significant joint subluxation and should be made on a case-by-case basis. A minimally displaced talar body fracture in a patient with significant neuropathy may be best treated nonoperatively, whereas a Hawkins III talar neck fracture with posteromedial extrusion of the talar body should be treated surgically to relieve soft tissue and/or neurovascular compromise regardless of the presence of neuropathy. Elderly patients with limited ambulatory capacity, similarly, may be best treated nonoperatively if the joint is not significantly displaced or dislocated.
On occasion, poor soft-tissue conditions complicate the operative treatment of these fractures. For example, a dual incision approach to a talar neck fracture may be contraindicated in situations where the anterolateral skin is compromised (see Fig. 34.4A-D). Also, extensile exposures may be contraindicated in patients with marginal perfusion of the extremity.
PREOPERATIVE PLANNING
History and Physical Exam
Knowledge of the mechanism of injury can be helpful in determining the energy imparted and the likelihood of comminution, articular cartilage damage, and associated ligamentous injuries. When the injury is the result of significant axial loading, there is an increased risk of irreversible cartilage damage that may lead to posttraumatic arthritis. A thorough history should also include any comorbidities such as diabetes and peripheral vascular disease that may adversely impact the decision to operate. The physical examination should document the presence of dorsalis pedis and posterior tibial pulses, skin integrity, skin ulceration or tenting, sensory exam (preferably with a 5.07 monofilament), and abnormal posturing of the toes that may indicate tethering/entrapment of tendons. Type III and IV talar neck injuries are commonly associated with tibial nerve compromise from posterior displacement of the talar body stretching the posterior tibial neurovascular bundle. Type II talar neck injuries commonly involve medial displacement of the talar head segment resulting in prominence and skin tenting over the anterolateral aspect of the talar body segment that can lead to soft-tissue compromise (Fig. 34.4A-D).
IMAGING STUDIES
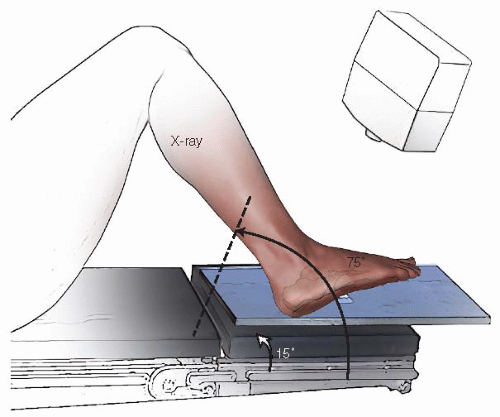
The standard radiographic evaluation for ankle and foot injuries includes anteroposterior (AP), lateral, and oblique views of the foot and ankle. The talus is both a foot and ankle bone, and fractures are commonly missed with inadequate radiographs. The Canale oblique view is helpful to assess length and alignment of the talar neck (Fig. 34.6). Shortening of the medial column of the foot secondary to impaction is common in talar neck fractures and is best seen on the Canale view.
Because of the unusual shape of the talus, numerous articular surfaces, and variability of fracture patterns, CT scans are an essential part of the radiographic evaluation of a talus fracture. CT is useful in defining the fracture morphology and detecting occult fractures in the ankle and foot. Concomitant osteochondral fractures are common with talar neck fractures and are not well visualized on plain x-rays.
TIMING OF SURGERY/REDUCTION
The urgency of reduction and timing of surgical intervention following talus fractures remain controversial. The initial fracture displacement, amount of comminution, and presence of an open fractures are thought to be factors associated with the development of posttraumatic osteonecrosis. Fractures that produce joint subluxation or dislocation, as well as those with significant soft-tissue compromise due to fracture displacement, require emergent reduction to avoid neurovascular compromise and/or skin necrosis. Because of the need for expedient reduction in these circumstances, preoperative planning is invariably limited. If the peritalar joints are reduced and fracture displacement is not significant, operative fixation can be performed when soft-tissue swelling and bruising have recovered and proper imaging studies have been obtained. In most patients, a well-padded splint provides adequate temporary support and pain relief. Provisional spanning external fixation to restore length and stability may occasionally be necessary in unstable fracture patterns or when the soft-tissue injury precludes early open reduction.
Knowledge of the fracture pattern and classification is very helpful when planning the surgical approach, methods of reduction, and fixation techniques. For example, talar body fractures and type III talar neck fractures with posteromedial extrusion of the talar body often require a transmalleolar exposure either through an existing medial malleolar fracture or an osteotomy of the medial malleolus. Reduction aids such as a femoral distractor may be necessary to reduce an extruded talar body. Chondral and osteochondral fractures that commonly accompany talar neck and body injuries often necessitate small diameter subarticular screws or bioabsorbable implants. Since talus fractures are articular injuries, it is helpful to have an assortment of small-diameter plates and screws to facilitate anatomic restoration of the joint surface and rigid fracture fixation to allow early motion.
SURGICAL TECHNIQUE
Access to the talus for fracture surgery is limited, and extensile approaches are not recommended. Fracture pattern and associated soft-tissue disruptions may indicate areas of potential compromised vascularity. The goal of fracture surgery is to gain access to the bone for reduction and fixation without further insult to the remaining blood supply. Unnecessary dissection should be avoided, and ligamentous attachments should be protected.
Imaging studies are carefully assessed to determine fracture pattern, areas of comminution, medial neck shortening, and associated osteochondral fractures (Fig. 34.7A-D). The patient is positioned supine on a radiolucent table with a bolster placed beneath the affected extremity. Intraoperative C-arm fluoroscopy is essential and should enter from the opposite side of the table. A well-padded pneumatic tourniquet is placed on the proximal thigh (Fig. 34.8). General anesthesia with muscle paralysis is preferred to regional techniques to better counteract the strong deforming forces in the hindfoot. Spinal or regional anesthesia may be preferable in a small number of patients with significant cardiopulmonary comorbidities but is not routinely employed because it interferes with evaluation of the postoperative neurovascular status. This is particularly
true in patients with other lower extremity injuries. A first-generation cephalosporin is given prior to the incision, and two additional postoperative doses are administered. In patients with open injuries, the duration of antibiotics is increased.
true in patients with other lower extremity injuries. A first-generation cephalosporin is given prior to the incision, and two additional postoperative doses are administered. In patients with open injuries, the duration of antibiotics is increased.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree