Surgical Treatment of Osteochondritis Dissecans of the Knee
Christina R. Allen MD
Marc R. Safran MD
History of the Treatment of Osteochondritis Dissecans
Osteochondritis dissecans (OCD) of the knee is a condition that causes separation or fragmentation of a segment of subchondral bone and overlying cartilage from the remaining underlying subchondral bone. With progression of the condition, this pathology may result in signs or symptoms correlating with the disease stage as it impacts on the integrity of the overlying articular cartilage.
Early signs or symptoms associated with intact cartilage over an OCD lesion may be related to cartilage softening or an alteration in the mechanical properties of the cartilage. At this early stage, the patient may complain of vague anterior knee pain and a variable amount of swelling that is typically intermittent and often related to activity level. In later stages, due to lack of underlying support of the cartilage, the patient may present with signs or symptoms of articular cartilage separation (cartilage flaps or “loose bodies” causing locking or catching symptoms), inflammatory synovitis, or a persistent or intermittent effusion. Because lesions may become symptomatic, surgical intervention may often be required. In 1840, Paré was the first to describe the removal of joint loose bodies, which were presumably osteochondral fragments.1 Operative treatment for unstable lesions has been traditionally attributed to Smillie,2 who developed a nail for open reduction and internal fixation of displaced and unstable lesions.
The incidence of OCD has been estimated at between 0.02% to 0.03% (based on a survey of knee radiographs) and 1.2% (based on knee arthroscopies).3,4 The highest rates appear among patients between 10 and 15 years of age, with rare instances in children under 4 or patients over 50 years of age. Higher rates among males are historically reported, with an approximate 2:1 ratio compared with females, though recent data suggest that this difference is lessening.5 Bilateral lesions, typically in different phases of development, are reported in 15% to 30% of cases and mandate assessment of both knees in all those presenting with this diagnosis.6 OCD lesions of the knee most commonly involve the lateral aspect of the medial femoral condyle (Fig. 56-1A,B). The lateral femoral condyle is less frequently involved, and patellar OCD lesions are even more rare.6,7
The etiology of osteochondritis dissecans remains unclear. König8 originally described the condition in 1888 and gave it a name indicative of his initial belief that OCD was due to an inflammatory reaction of both the bone and the cartilage. Current consensus regarding etiology is debatable, although an inflammatory etiology is unlikely, as recognized by König a decade later. Repetitive microtrauma, ischemia, epiphyseal abnormalities, osteochondral fracture, genetic predisposition, and endocrine abnormalities have all been postulated as potential contributors to development of OCD.
Clinically, Cahill5 and Mubarak and Carrol9 emphasized a distinction between two types of OCD as recognized by the osseous age of the patient at the time of symptom onset. Those with open physes are considered to have juvenile onset OCD, while those who are skeletally mature at the time of symptom onset have the adult form. Paradoxically, adult onset OCD may simply be a delayed onset of previously asymptomatic juvenile OCD that failed to heal and manifests later with loosening and joint degeneration. Skeletal age at onset of symptoms appears to be the most important determinant of prognosis and remains an essential factor directing the timing and nature of treatment decisions. Paletta et al.10 found that all patients with open physeal plates and increased activity on bone scan were more likely to heal their OCD lesion, while those without increased activity did not heal. In contrast, among patients
with closed growth plates only 33% healed despite having a similar increase in activity within the lesion.
with closed growth plates only 33% healed despite having a similar increase in activity within the lesion.
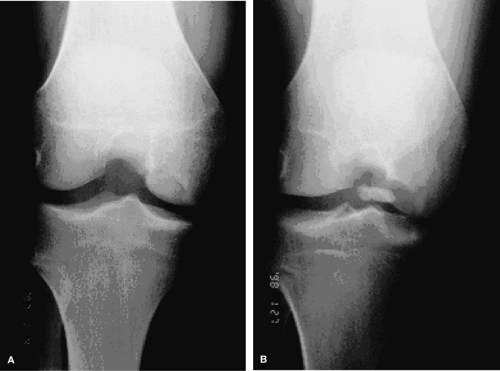 Fig. 56-1. The classic location for osteochondritis dissecans. AP radiographs demonstrates a lateral aspect of the medial femoral condyle OCD lesion before (A) and after (B) displacement. |
Both radiographic and surgical classification systems for OCD lesions have been described, with few having clear prognostic significance. Using plain radiographs of the talus, Berndt and Harty11 classified OCD in four stages that describe the condition and position of the osteochondral fragment, ranging from compression of the subchondral bone to complete detachment of the fragment (loose body). Cahill and Berg12 describe a method of dividing the AP and lateral radiographs into 15 distinct zones. This alphanumeric system provides standardization for research and descriptive purposes, but has found limited clinical application to date with regard to treatment or prognosis.5
DiPaola et al.13 classified lesions according to appearance on magnetic resonance imaging (MRI) and correlated specific findings with the potential for fragment detachment. They described lesions containing fluid (high T2 signal) behind the subchondral fragment as potentially unstable, as this suggested a breach of the cartilage surface.The presence of a low T2 signal behind the fragment suggests that there is no fluid behind the fragment, indicating a stable fibrous attachment and potentially intact cartilage surface. Other reports suggest a similarly high level of confidence for predicting lesion stability using intra-articular gadolinium contrast.14
DiPaola’s classification system has proven to be reasonably accurate and predictive of the stability of lesions on arthroscopic examination. O’Connor et al.15 found an 85% correlation between preoperative MRI findings using DiPaola’s criteria and arthroscopic findings graded with Guhl’s arthroscopic classification system for OCDs.In Guhl’s16 system, OCD stages are defined by cartilage integrity and fragment stability. Type I lesions have softening of cartilage but no breach of the cartilage surface; type II lesions have breached cartilage but are stable. Type III osteochondral defects have a definable fragment that remains partially attached (flap lesion), type IV lesions constitute an osteochondral defect at the donor site with a resultant loose body in the knee joint.
Indications and Contraindications
No randomized, controlled clinical trials exist for either operative or nonoperative interventions for OCD of the knee. In general, physis maturity, dissection of the lesion from the adjacent subchondral bone or stability, size, and location of lesions and cartilage surface integrity have been used as predictive criterion for necessity of operative intervention.
Recently, a large multicenter review of the European Pediatric Orthopedic Society’s experience with treatment of OCD lesions was performed.6 Lessons from this study are derived from the knees of 318 juvenile patients and 191 adults. The authors of the study made several important distinctions and conclusions. They determined that if there are no signs of dissection (loosening), the prognosis is significantly better and that pain and swelling are not good indicators of fragment dissection. Additionally, plain radiographs and computed tomography (CT) scan are not useful in predicting dissection. Sclerosis on plain radiographs predicts a poor response to drilling. Further analysis demonstrated that lesions greater than 2 cm in diameter had a worse prognosis, and when there is evidence of dissection, surgical treatment results are better than nonsurgical. Lesions in the classical location of the lateral aspect of the medial femoral condyle had a better prognosis. Finally, although patients with adult onset symptoms had a higher proportion of abnormal findings on radiographs after the treatment period (42%), more than one in five of those with open epiphyseal plates (22%) had abnormal knee radiographs at an average of 3 years after starting treatment.
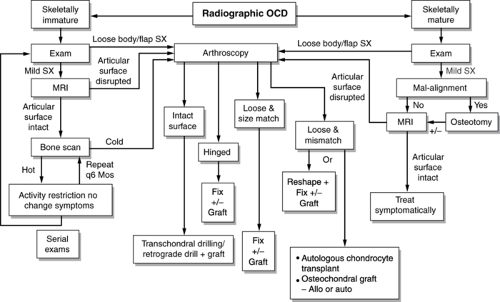
An algorithm for treatment decisions is outlined in Fig. 56-2, with the primary goal being to promote healing of lesions in situ and preventing displacement.
Nonoperative treatment through activity modification may include a wide spectrum of approaches that have historically included crutches for limited weight bearing, braces, or even casts for non-compliant patients. In patients without significant sports participation, prescribing a non–weight-bearing status and range of knee motion exercises may be beneficial to cartilage and help avoid the potential disaster of “cast disease” and arthrofibrosis. Our approach is to limit sports activities without immobilization, casting, or crutches, except for the noncompliant patient.
Choosing surgical intervention for managing OCD of the knee and selecting a strategy for repair, reconstruction, or removal of osteochondral lesions depends upon the stability of the osteochondral lesion and the integrity of the overlying cartilage. Essentially, the indications for operative treatment in skeletally immature patients are a symptomatic osteochondral fragment that is attached but not healing, a partially or completely detached fragment with a disrupted articular surface, and loose bodies. In skeletally mature individuals, lesions are less likely to heal with conservative treatment once fluid is dissecting under the fragment; therefore, symptomatic lesions and loose bodies are generally treated surgically.
Preoperative Imaging Studies
Three standard roentgenograms of the knee, bilateral posterior-anterior (PA) 30-degree bent knee (Rosenberg or notch
view), axial (Merchant) view, and lateral weight-bearing exams are routine in the initial evaluation for OCD.17 Lesions of the weight-bearing surface of the femur are best seen with a flexed knee PA view and may help identify the lesions in the posterior condyles (Fig. 56-1A,B). Lateral radiographs allow recognition of the relative anterior-posterior location and identification of normal benign accessory ossification centers in the skeletally immature patient as described by Caffey et al.18 An axial view of the patella should be added, as it may uncover the unusual patella lesion. Plain radiographs also allow a baseline assessment of the lesion size, presence or absence of sclerosis, presence or absence or lesions in the contralateral knee, potential dissection, and assignment to one of several classification systems that are based on radiographic criteria.
view), axial (Merchant) view, and lateral weight-bearing exams are routine in the initial evaluation for OCD.17 Lesions of the weight-bearing surface of the femur are best seen with a flexed knee PA view and may help identify the lesions in the posterior condyles (Fig. 56-1A,B). Lateral radiographs allow recognition of the relative anterior-posterior location and identification of normal benign accessory ossification centers in the skeletally immature patient as described by Caffey et al.18 An axial view of the patella should be added, as it may uncover the unusual patella lesion. Plain radiographs also allow a baseline assessment of the lesion size, presence or absence of sclerosis, presence or absence or lesions in the contralateral knee, potential dissection, and assignment to one of several classification systems that are based on radiographic criteria.
MRI studies are also useful in quantifying the size of the lesion. Again, the studies of DiPaola et al.13 have shown that lesions containing fluid (high T2 signal) behind the subchondral fragment tend to be unstable and may require surgical treatment (Fig. 56-3), whereas lesions that demonstrate a low T2 signal behind the fragment indicate a stable fibrous attachment.
The use of bone scans may be beneficial in monitoring the healing progress of a stable lesion and may also be useful in predicting the healing potential of a lesion. As previously noted, Paletta et al.10 found that all patients with open physeal plates and increased activity on bone scan went on to heal their OCD lesions, while those without increased activity did not heal without surgical intervention. In contrast, among patients with closed growth plates only 33% healed despite having a similar increase in activity within the lesion.
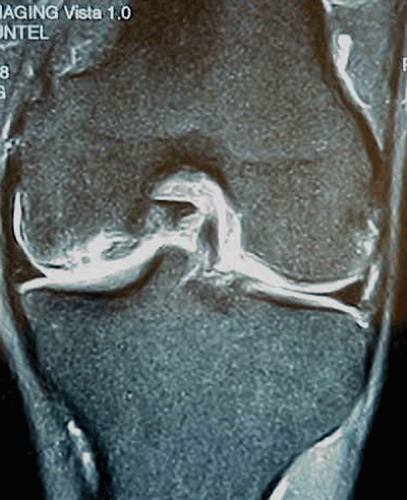 Fig. 56-3. T2-weighted MRI of the knee demonstrating high signal behind osteochondral fragment, indicating an unstable fragment.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|