Surgical Treatment of Nerve Injuries in Continuity
Matthew E. Hiro
Randy R. Bindra
DEFINITION
A nerve injury in continuity occurs when there is loss of axonal function with preserved structure of the supportive connective tissue.
By definition, the epineurium is preserved in a nerve injury in continuity.
Because varying degrees of axonal interruption may occur, the extent of functional loss in terms of numbness and paralysis is variable.
The severity of injury varies with degree of preservation of the endoneurium and the perineurium.
ANATOMY
The cross-sectional anatomy of the peripheral nerve is discussed in detail in Chapter 88.
Endoneurial tubes form the basic conduit for the Schwann cell-encased axon.
PATHOGENESIS
Several mechanisms may cause a nerve injury in continuity, but the most common is nerve stretch.
When a nerve is subject to blunt injury or stretch, axonal disruption can occur without externally visible injury to the nerve.
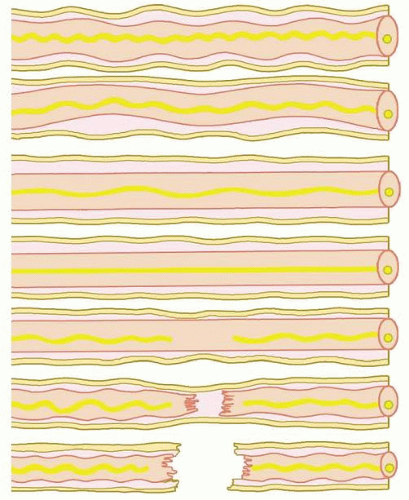
Stromal elements are more resilient to stretch and remain preserved to a variable extent (FIG 1).
The type of recovery seen after an injury depends on preservation of the endoneurial tube.
In the mildest forms of injury, with preserved endoneurial tubes, regenerating axons follow their original path. The destination is reached with good outcome. There is no axonal mismatch, and the recovery is termed uncomplicated regeneration.
When the endoneurial tube is disrupted, axonal regeneration is disorganized. Axons sprout and grow in a different direction and mismatch occurs. This form of repair, termed complex regeneration, is associated with a clinically less satisfactory outcome.
With more severe forms of stretch injury, additional disruption of the perineurium occurs, resulting in a greater fibrotic response and resultant scarring of the nerve.
The nerve trunk, which externally appears uninterrupted due to the intact epineurium, demonstrates an injured segment that is enlarged due to intraneural fibrosis surrounding a mass of disorganized axons. This is referred to as a neuroma in continuity (FIG 2).
NATURAL HISTORY
Pathoanatomy associated with the injury, pathologic changes resulting from this altered anatomy, and functional recovery are closely related.
More anatomic disruption results in a stronger pathologic response and worse outcome.
Sunderland’s classification of injury severity is useful to categorize injury and plan treatment.
Type I
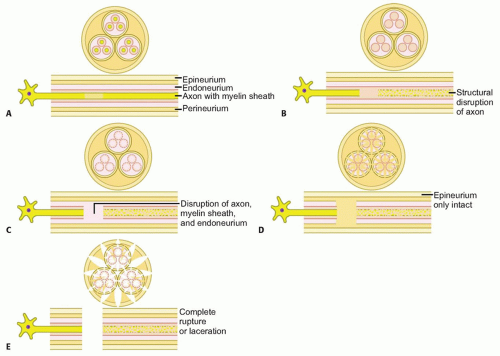
The mildest form of injury involves loss of axonal function without actual structural interruption: neurapraxia (FIG 3A).
Type I injury is seen after mild stretch injuries, tourniquet palsy, and external compression of a nerve, as in radial nerve compression in “Saturday night palsy.”
Although structurally intact, axons fail to conduct impulses, secondary to malfunction of ion channels along the injured segment.
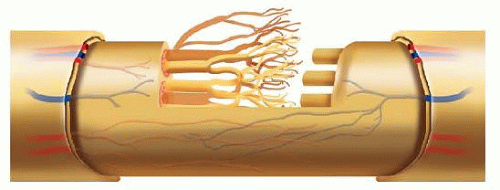
FIG 2 • Neuroma in continuity. The enlarged part of the nerve consists of a mixture of intact and damaged axons surrounded by scar tissue and regenerating axons.
No visible change in the microscopic or macroscopic appearance of the nerve is present, and there is no wallerian degeneration of the distal segment.
Electrophysiologic testing does not reveal a conduction block or denervation potentials.
Recovery starts within a few weeks and can be expected to be complete.
Because axons recover conductivity in a variable pattern, clinical recovery follows a random pattern.
Type II
There is structural disruption of the axon, but the endoneurium is preserved (FIG 3B).
Type II injury is seen after more severe stretch injuries, such as radial nerve palsy resulting from a closed humerus fracture.
Wallerian degeneration results and electrophysiologic tests reveal distal conduction block and denervation.
As regenerating axons progress distally, proximal muscles are reinnervated first. Clinically, recovery occurs in a proximal to distal direction.
Because there is no axonal mismatch, recovery usually is complete but takes longer, usually several months.
Type III
The axon, myelin sheath, and endoneurium are interrupted (FIG 3C).
Recovery is less predictable because regenerating axons may not follow previous pathways (complicated regeneration).
With the perineurium preserved, recovery can take place without surgical intervention but usually is incomplete due to axonal misdirection.
Injury to small vessels within the endoneurium leads to an inflammatory response. Fibroblast activation results in a variable degree of interfascicular scarring that may impede nerve regeneration.
Type IV
In more severe stretch injuries, the internal nerve structure is completely disrupted, leaving only an intact epineurium (FIG 3D).
Retraction of fascicles and scarring within the nerve are present. Even though the nerve is in continuity, no clinically significant recovery can be expected without surgical intervention.
Type V
Type VI
Mixed injuries with components of types I to V
PATIENT HISTORY AND PHYSICAL FINDINGS
Stretch injuries that result in nerve injury in continuity usually are proximal. These injuries often take place as the nerve root exits the spinal cord or involve the brachial plexus in the neck or upper arm.
At more distal levels, nerve stretch injuries usually are the result of displaced fractures or dislocations.
There usually is a history of significant trauma, and patients complain of pain and paresthesias with a variable amount of functional loss distal to the site of injury.
Incomplete loss of function often indicates an incomplete nerve injury.
Severe pain or paresthesias after any closed fracture should alert the clinician to the possibility of an associated nerve injury.
Complete loss of function does not necessarily imply complete disruption of the nerve.
Documented lack of recovery on serial clinical examinations is essential to determine the severity of the injury and the need for surgical intervention.
Muscle strength is charted against a timeline at every visit. Progressive muscle recovery in a proximal to distal direction indicates spontaneous axonal regeneration.
Tinel sign and its gradual progression is also a useful measure of nerve recovery.
Recovery within a few weeks of injury and with a random pattern usually suggests a type I injury or neurapraxia.
After incomplete injury to a peripheral nerve, function is lost in a predictable order: motor, proprioception, touch, temperature, pain, and sympathetic function.
Recovery usually occurs in the reverse order.
In a closed injury without any obvious fractures, the site of nerve injury is not always obvious.
Careful mapping of the motor and sensory deficit will help to distinguish the level of injury.
The pattern of sensory loss is a reliable way to determine the level of injury. A more proximal injury usually follows a dermatomal pattern, whereas a distal injury follows the distribution of the nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree