Surgical Treatment of Injection Injuries in the Hand
Joshua Choo
Rimma Finkel
Morton Kasdan
DEFINITION
Injuries caused by high-pressure injection equipment, which can generate pressures of 2000 to 12,000 pound per square inch (psi),9 are more than sufficient force to break the skin.15
Substances typically injected include grease, paint, paint thinners, diesel fuel, oil, water, and cement. Cases involving molten metal,3 dry cleaning solvents,11 and veterinary vaccines5 have also been documented.
Hallmark of injury is an innocuous-appearing superficial wound that can greatly underestimate the true extent of injury (FIG 1).
The three most important determinants of morbidity are the (1) type of substance injected, (2) anatomic location of injury, and (3) delay in treatment.
Treatment of injection injuries is urgent and thorough surgical débridement.
High-pressure injection injuries occur most frequently in young men, particularly among those who are manual laborers.
Previously, it was thought that most of these injuries occurred to people who had been on the job for less than 6 months, but more recent studies show that the mean time on the job was 11 years.12,32
Typical scenarios include grasping pressurized tubing in which there is a break in the seal or attempting to unclog the nozzle of a high-pressure injector with the guard removed (FIG 2).
With the increasing use of power contrast injection in computed tomography (CT), contrast extravasation injuries may be classified under injection injuries of the upper extremity. However, the pressures involved are generally much lower (100 psi),33 the associated injuries are more proximal, and the natural history is generally benign, with surgery rarely being required.
ANATOMY
Quick facts
The index finger, thumb, palm, and small finger are afflicted in descending order.
The site of injection is an important determining factor in predicting the zone of deep injury and morbidity.
Experimental reproductions of high-pressure injections have shown that the anatomic location of entry is an important factor in predicting the distribution of injury:
Eccentric sites of injury tend to bypass the palmar tissue and result in dorsal involvement.
Injections in the tough glabrous skin overlying and the thicker portions of the fibrous flexor sheaths (annular pulleys) of the finger (midphalanx) tend to be deflected circumferentially in the superficial tissue, as the flexor sheath is less likely to be penetrated.
Injection sites in the skin creases, that is, thinner parts of the flexor sheath (cruciate pulleys) overlying the distal or proximal interphalangeal joint, are more likely to result in penetration of the flexor sheath and proximal spread through the tenosynovial space.
Injuries that penetrate the tenosynovial space of the index, long, and ring fingers do not spread beyond the distal palmar crease; injuries to these fingers are more likely to be concentrated in the finger itself and cause local inflammation and ischemia.15,16
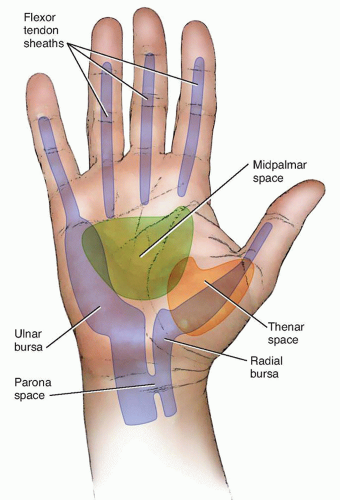
In contrast, the tenosynovial sheaths of the thumb and little finger extend into the proximal palm via the radial and
ulnar bursae and may communicate with the myofascial spaces of the palm (FIG 3).15 Thus, injections in the thumb and little finger tend to propagate in a more proximal direction and may fill the radial and ulnar bursae.

FIG 2 • Injury commonly occurs to the nondominant hand while attempting to clean the nozzle of a high-pressure injector. Note that the nozzle guard has been removed.
In 85% of cases, the radial and ulnar bursae are connected by Parona space, leading to potential spread of injury between the radial and ulnar bursae.21
Similarly, the palm contains deep myofascial spaces that allow injected material to be dispersed within a larger space (thenar and midpalmar space; see FIG 3). Consequently, injections in the thumb, palm, thenar, and hypothenar eminences are more likely to require a wider débridement but are less susceptible to ischemic injury and permanent impairment.
In general, distal injuries are more likely to require amputation than proximal ones and finger injuries are associated with higher morbidity and amputation rates than thumb or palm injuries.14
The anatomic studies on which many of these observations were made used pressures of 750 psi. Injections at much higher pressures may be enough to overcome tissue resistance, leading to less predictable patterns of injury.
PATHOGENESIS
Two key pathogenic mechanisms are responsible for the morbidity of high-pressure injuries: (1) mechanical injury directly resulting from the injected material, which is a function of viscosity, velocity, and volume, and (2) the inflammatory host response, which is a function of the irritant/chemical properties of the injected material.
The degree of mechanical injury has been shown to be inversely proportional to the viscosity of the material and proportional to the volume of material delivered and the pressure at which it was delivered.9,13,27 For example, injected material with relatively low viscosity, such as paint thinner,10 has been shown to result in wider zones of injury and greater morbidity.
The type of inflammatory response incited by the injected material also has an important effect on degree of injury. Only rare cases of water or air injection have been found to result in amputation. In contrast, organic solvents such as oil paint have been found to have a 10-fold increased incidence of amputation compared to other materials such as hydraulic fluid or grease (58% vs. 6%). The inflammatory response to various materials is clearly different.14
Controversy continues as to which aspect dominates in these injuries; however, they are more likely synergistic, with the inflammatory response compounding the mechanical injury.
Time elapsed before intervention has a major influence on prognosis (see Natural History, next section). Most agree that surgery should be done within 6 hours after injury to decrease morbidity.29
NATURAL HISTORY
The natural history of high-pressure injuries can be divided into three stages.
Acute stage
The acute stage occurs immediately.
The injection causes external compression and spasm of the vessels, leading to compromised blood flow that is manifested by white, mottled tissue; numbness; severe pain; or a combination of these findings.
Any initial paresthesias that occur are due to local compression or chemical irritation of the involved nerves.
During this stage, the site of injection is key in determining where the material has spread.
The volume of material injected also determines the degree of tissue distention and impairment of blood flow.
Intermediate stage
During the intermediate stage, a foreign body reaction induces granuloma formation and fibrosis.
Severity of inflammation that occurs is determined by the volume and type of substance.
Injection of paint solvent has a significantly higher morbidity due to its low viscosity, allowing diffusion through the soft tissues. Its corrosive effects cause severe tissue necrosis.9
Grease injections have more chronic inflammatory reactions, leading to prolonged sequelae (foreign body granulomas).13,28
Schoo et al27 reported that amputation rates associated with various injection injuries were as follows: paint thinner, 80%; paint (soya alkyl base), 58%; automotive grease, 23%; and hydraulic fluid, 14%.
Late stage
Late stage of injury occurs when the granulomas break open, resulting in draining sinuses and cutaneous lesions.8,27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree