Surgical Treatment of Cavus Foot
Richard M. Schwend
Brad Olney
DEFINITION
A cavus foot deformity in children develops from muscle imbalance that leads to forefoot pronation in relation to the hindfoot. When well established, it is readily recognizable by an abnormally high medial arch that persists with weight bearing (FIG 1).
Commonly a result of hereditary sensory motor neuropathy (HSMN), it is frequently difficult to determine the underlying cause.
ANATOMY
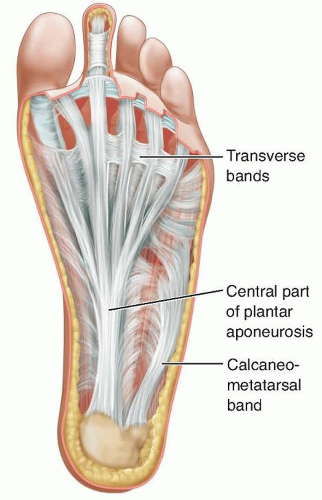
The plantar fascia is an extensive fibrous structure that spans the foot between the medial aspect of the calcaneal tuberosity and the transverse metatarsal ligaments at the metatarsal heads (FIG 2). It stabilizes the arch of the foot and protects the underlying neurovascular structures from injury.
During the gait cycle, the plantar fascia assists in the dynamic changes of the arch.
At heel strike, there is forefoot supination and heel inversion, whereas eccentric contraction of the quadriceps muscles absorbs much of the energy.
During midstance, there is unlocking of the midtarsal joints with hindfoot pronation and internal tibia rotation.
At toe off, the plantar fascia helps lock the midtarsal joints to assist the foot to be a rigid lever for forward propulsion.
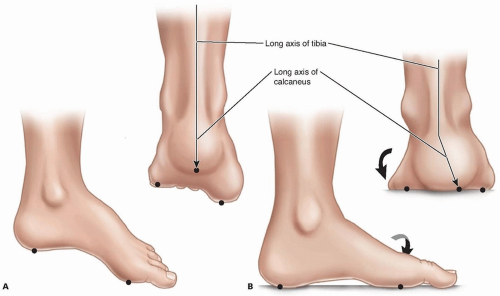
This is termed the windlass effect, when passive dorsiflexion at the metatarsophalangeal joints tightens the plantar fascia, leading to elevation of the medial arch and tarsal joint stability (FIG 3).
PATHOGENESIS
In progressive conditions such as HSMN, there is muscle imbalance with weakness of the intrinsic, tibialis anterior, and peroneus brevis muscles. This can lead to a relative overpull of the peroneus longus and posterior tibialis muscles.

FIG 1 • A 17-year-old girl with HSMN type 1A. Cavus right foot deformity with high arch, plantar crease, apex of deformity at the midfoot, and claw toes.
Clinical muscle testing shows that although both peroneal muscles are weak, the larger peroneus longus muscle retains relatively more strength. Differential peroneal nerve compression at the proximal fibula is postulated to cause relative sparing of the peroneus longus innervation.5
Computed tomography (CT) imaging studies in Charcot-Marie-Tooth disease, a major category of HSMN, showed early foot intrinsic muscle atrophy with sparing of the abductor hallucis and involvement of the peroneus brevis, peroneus longus, and flexor hallucis longus muscles.13
Magnetic resonance imaging (MRI) studies have shown dominance in the size of the peroneus longus muscle versus the tibialis anterior.16
The muscle imbalance and intrinsic muscle weakness lead to an unopposed extensor digitorum longus, hyperextension of the lesser toe metatarsophalangeal joints, and phalangeal joint flexion by the long and short toe flexors.
There is an exaggeration of the windlass effect with claw toe deformities.
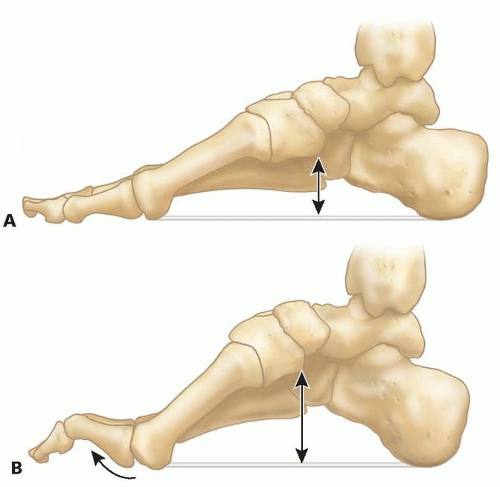
FIG 3 • A,B. Windlass effect. The foot is an arch. If the plantar tissues tighten and become shorter, the fixed length of the arch forces it to become taller.
The first metatarsal becomes even more plantarflexed by the action of the peroneus longus and with time becomes fixed in this position.
The plantar aspect of the foot assumes a tripod position, resulting in hindfoot varus (FIG 4).
The cavus foot remains a rigid lever throughout stance phase, leading to increased stress and lack of shock absorption, pain, and callosities.
NATURAL HISTORY
Cavus foot is rarely present at birth but develops with time.
The natural history depends on the underlying diagnosis. The underlying cause affects the outcome, so determination of cause is essential. An underlying diagnosis can be found in the brain, spinal cord, peripheral nerves, or the foot itself.
Cavus foot deformity can be either progressive or nonprogressive.
Cavus foot deformity involves either a dorsiflexion deformity of the calcaneus or a forefoot plantarflexion deformity.
The most common cause of progressive bilateral cavus foot deformity is HSMN. HSMN is a group of progressive peripheral nerve diseases and has a heterogeneous genetic classification.
Charcot-Marie-Tooth disease involves types I and II HSMN, with HSMN IA the most common type seen in 60% of patients with HSMN.
HSMN type I has myelin degeneration, type II is the axonal degeneration form, and type III (Dejerine-Sottas disease) is more severe and presents in infancy.
There are more than 17 different genetic loci determined for Charcot-Marie-Tooth disease.
The prognosis for these progressive conditions is less favorable than for the nonprogressive disorders.
The natural history of HSMN is related to the underlying type.
Progression of muscle involvement begins initially in the intrinsic muscles, followed by the anterior compartment, the peroneal muscles, and then the posterior muscles.14
The foot can assume a cavovarus, calcaneocavus deformity, or even a valgus deformity and may have more unilateral severity (HSMN type III).4
Associated hip dysplasia may be asymptomatic or may present with symptoms. Acetabular dysplasia may be the first indicator of HSMN.3
In progressive conditions that are left untreated, a flexible and correctable foot may become rigid with structural bony changes. This can lead to inability to participate in athletics and pain and difficulty with shoe wear and normal walking. Treatment is recommended when the foot is still flexible.
Unilateral cavus foot can have a number of causes. The idiopathic variety may be progressive, with an unpredictable natural history.
Patients with nonprogressive conditions, as seen in cerebral palsy or spinal cord disorders, may fare better but still can have long-term problems with athletics, metatarsalgia, plantar fasciitis, and iliotibial band syndrome.9
Calcaneocavus deformity is often seen with nonprogressive conditions such as spina bifida or clubfoot deformity with an overlengthened heel cord. Problems include heel pain or heel pad ulceration if sensation is deficient and weak or no push-off or crouch gait if not braced.
PATIENT HISTORY AND PHYSICAL FINDINGS
The physical examination is used to determine the underlying diagnosis and to determine characteristics of the cavus foot deformity that would indicate surgical correction is needed.
Physical examination should include observation of the spine and its range of motion. Skin changes, scoliosis, or kyphosis may represent an underlying spinal cord abnormality.
The upper extremities are evaluated for intrinsic muscle wasting and weakness. Atrophy or weakness in the hand suggests HSMN.
The clinician evaluates hip range of motion and looks for Trendelenburg gait. Bilateral hip dysplasia newly diagnosed in a teenager is highly suggestive of HSMN.
Lower extremities are evaluated for size, muscle strength, and firmness and tenderness along the course of major nerves. Bilateral calf atrophy is seen with spina bifida and may be present in severe HSMN. Unilateral atrophy may be seen with diastematomyelia, tethered spinal cord, or split cord malformation.
A neurologic examination is performed. Patients with HSMN may have decreased sensation to light touch, position sense, or vibration. There may be obvious weakness of the anterior tibialis muscle, preventing ability to heel walk. Deep tendon reflexes may be decreased or absent in HSMN and Friedreich ataxia.
The foot is examined for deformity (cavus, cavovarus, or calcaneocavus). Bilateral deformity is typical for HSMN. Unilateral deformity may be present with a structural abnormality. The clinician locates the apex of the midfoot deformity and determines whether the foot is rigid or flexible. The hindfoot is rarely in equinus.
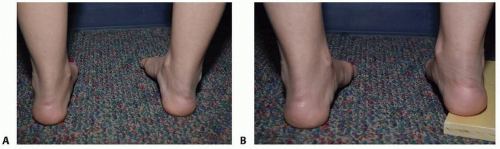
The Coleman block test is performed (FIG 5).
The toes are examined for any deformities. Cavus foot may not have associated toe abnormality. Rigid claw toe abnormality requires surgical treatment.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Bilateral standing anteroposterior (AP) and lateral radiographs are standard.
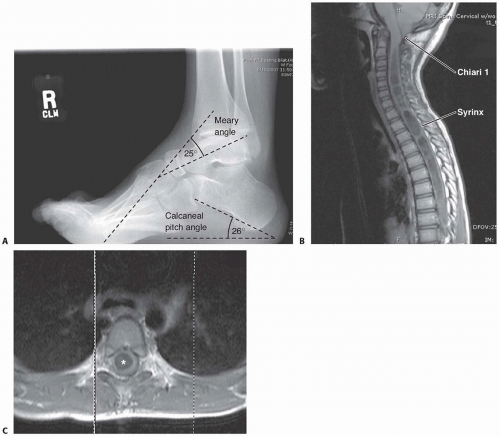
On the lateral weight-bearing radiograph, the clinician should determine the calcaneal pitch; greater than 30 degrees indicates chronic gastrocnemius-soleus weakness (FIG 6A).
The Meary angle, the angle between the shaft of the first metatarsal and the axis of the talus, is normally 0 degree.
Ankle equinus, forefoot equinus, the amount of cavus, and the apex of the midfoot deformity are determined.
With the foot positioned for the Coleman block test, a lateral radiograph of the foot can document the degree of hindfoot correction.1
In the patient with known or possible HSMN, a standing AP pelvis view is obtained to screen for the presence of hip dysplasia.17
Standing full-length posteroanterior and lateral spine radiographs are obtained when a spinal abnormality is suspected or if the underlying diagnosis is in question.
MRI of the entire brainstem and cervical, thoracic, and lumbar spine is performed when a spinal cord tumor, syrinx, tethered cord, or Chiari I malformation is of concern (FIG 6B,C).
Nerve conduction and electromyelographic (EMG) studies may be done to evaluate for HMSN. In HMSN type I, motor nerve conduction is markedly slowed. In HMSN type II, there is near-normal motor nerve conduction but EMG
evidence of denervation. Molecular DNA testing of peripheral blood may be used for diagnosing HSMN; therefore, sural nerve biopsy is generally not necessary.
DIFFERENTIAL DIAGNOSIS
Hemiplegic cerebral palsy
Spastic diplegic cerebral palsy with calcaneocavus foot deformity if the Achilles tendon has been overlengthened
Friedreich ataxia
Myelodysplasia
Chiari I malformation with syringomyelia and scoliosis
Diastematomyelia and split cord malformation
Poliomyelitis
Spinal cord tumors
Guillain-Barré syndrome
Peripheral nerves: HSMN types I and II
Sciatic nerve injury
Peripheral nerve tumor
Silent compartment syndrome after tibia or foot fracture
Residual deformity of clubfoot
Idiopathic
Subtalar tarsal coalition (rare)
Severe limb length discrepancy leading to a fixed equinus gait
NONOPERATIVE MANAGEMENT
Nonoperative management is appropriate for mild or nonprogressive deformity.
Inserts that support the lateral forefoot and eliminate hindfoot inversion may be helpful.
Gel heel cups and replacing worn athletic shoes assist the stiff foot in energy absorption.
Extra-depth shoes and orthotics that unload pressure points may help in more advanced cases.
SURGICAL MANAGEMENT
Surgical treatment is necessary for more severe nonprogressive cases or for progressive cases. The functional goal is to correct the cavus deformity and to obtain a mobile, plantigrade, and well-balanced foot while avoiding common pitfalls. Treatment is best performed when the foot is still
flexible. Staged procedures, correcting deformity first and balancing muscles at a later stage, may be safer for the foot.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree