Surgical Treatment of Carpal Bone Fractures Excluding the Scaphoid
Kenneth R. Means Jr.
Thomas J. Graham
DEFINITION
These injuries include fractures of the lunate, triquetrum, pisiform, hamate body or hook, capitate, trapezoid, and trapezial body or ridge.
Any fracture involving the carpal bones should raise suspicion of associated carpal instability.
ANATOMY
Certain anatomic features of the carpal bones make them more susceptible to injury. These include the unique osteologic regions of some of the carpal bones, such as the hook of the hamate, the ridge or tubercle of the trapezium, and the neck of the capitate.
The slender shape and projection of the hamate hook make it an obvious injury target for direct trauma to the palmar-ulnar surface of the wrist (FIG 1A). Surgeons can identify the hook by placing their thumb interphalangeal joint on the patient’s pisiform and flexing their thumb toward the patient’s first web space. The surgeon’s thumb tip will land directly on top of the patient’s hamate hook.
The trapezial ridge may be considered a radial-sided analogue to the hamate hook in that it is a relatively prominent volar projection, further accentuated by the deep groove for the flexor carpi radialis (FCR) tendon that runs along its ulnar side (FIG 1B).
The strong, inelastic transverse carpal ligament attaches to the hamate hook ulnarly and the trapezial tubercle radially.
These facts make the ridge of the trapezium more susceptible to fracture after direct trauma to the thenar region of the hand.
The constricted neck portion of the capitate lies between the dense head proximally and the body distally. The body, which accounts for the distal half of the capitate, is rigidly constrained by its associations with the index, middle, and ring finger metacarpal bases; the trapezoid; and the hamate. As a result the capitate neck is a biomechanically vulnerable area.
Transverse plane fractures through the capitate neck are reported as being the most common.
Fractures across the neck place the capitate head at risk for avascular necrosis because the blood supply to the capitate flows retrograde toward the head proximally.
PATHOGENESIS
Traumatic fractures of the carpal bones may occur via direct or indirect mechanisms.
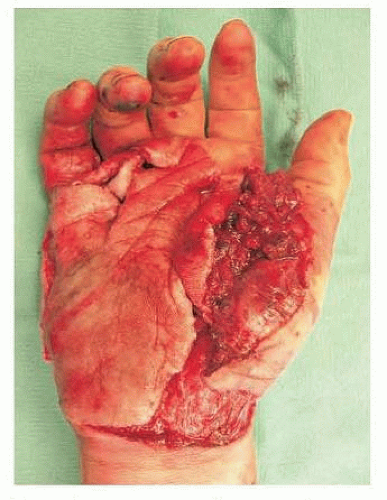
Direct mechanisms include crush injuries, which should alert the physician to the possible development of compartment syndrome of the hand. Compressive trauma to the hand in the anteroposterior (AP) plane will flatten the palmarly directed concave longitudinal and horizontal arches of the carpus and should raise suspicion for potential carpal body fractures and axial disruptions.
The presence of a seemingly unusual carpal bone fracture may be a herald of a globally destructive injury to the hand and other associated injuries, such as carpometacarpal (CMC) fracture-dislocations, longitudinal fractures of the metacarpals, severe thumb damage, and significant soft tissue injuries. This constellation of pathologies has been referred to as the “exploded hand” (FIG 2).
More focused direct trauma to individual carpal bones may also cause a fracture. Examples of this include direct blows to the dorsum of the hand, typically causing capitate, hamate body, triquetrum, or trapezium fractures, or direct injury to the palmar surface of the hand usually from a racquet or club, often causing a hamate hook or trapezial ridge fracture.
Indirect trauma includes the progressive perilunate instability patterns that are well described and may lead to fractures of the lunate, capitate, triquetrum, or other carpal bones.
Scaphocapitate syndrome involves a dorsiflexion and radial deviation mechanism by which the scaphoid bone fractures and is followed by a fracture of the capitate through the neck in the coronal plane. The capitate head may rotate up to 180 degrees from its anatomic position.
A progressive perilunate instability pattern can produce a similar coronal fracture through the capitate neck but normally without such a severe degree of capitate head rotation.
Minor indirect trauma can cause isolated carpal bone fractures.
The commonly seen avulsion fractures from the dorsum of the triquetrum may occur when a fall onto the palmar flexed wrist causes the dorsal radiotriquetral (also known as dorsal radiocarpal) ligament to avulse a portion of the dorsal cortex. However, this seemingly innocuous injury can be associated with significant radiocarpal and/or intracarpal instability patterns and the practitioner should carefully exclude these more severe injuries whenever treating a dorsal triquetral avulsion fracture.
An impaction type of fracture of the triquetrum body may be seen more often in patients with an elongated ulnar styloid.
NATURAL HISTORY
The natural history of carpal bone fractures depends both on the specific bone in question as well as associated impairment of other structures.
All of the carpal bones have at least three articular surfaces, except the pisiform, which articulates only with the triquetrum. Anatomic reduction of articular facets is a primary surgical goal in an effort to decrease the incidence and severity of posttraumatic arthritis.
Avascular necrosis can have a profoundly negative impact on final outcome after carpal bone fracture.
Concerns of vascular disruption arise when lunate and capitate fractures occur, although generally, fractures of the lunate are not associated with avascularity.
The potential for nonunion is most often seen with hamate hook fractures, capitate neck fractures, and trapezial ridge fractures, especially Palmer type II fractures that involve the tip and not the base of the ridge.
Barring nonunion, the related instabilities and involvement of other hand components in association with carpal fractures excluding the scaphoid are the most troublesome issues and will most significantly affect patient outcome.
PATIENT HISTORY AND PHYSICAL FINDINGS
Determining the mechanism of injury is the most important component of taking the patient’s history.
Neurovascular symptoms should be explored, especially when a severe crush or high-energy mechanism is involved, or in cases of hamate hook or pisiform fractures, with special attention to the ulnar neurovascular structures within Guyon’s canal.
A complete evaluation of the median, radial, ulnar, and digital nerves is warranted. Assessment of capillary refill, color, temperature, and Doppler signal determines the vascular status. Clinical or Doppler Allen examination may be warranted if radial and/or ulnar artery thrombosis or disruption is suspected.
The examiner should observe the patient’s hand and wrist for swelling, deformity, and skin and soft tissue injuries, including possible open fractures or fracture-dislocations.
Swelling and soft tissue damage give an indication as to the severity of the injury. The presence of deformity alerts the examiner to possible carpal dislocations that require emergent reduction. Open fractures and fracture-dislocations will guide surgical management.
The examiner should ask the patient where the pain is most significant. The examination should start away from, and progress toward, this point. The hand, forearm, and elbow should also be palpated to assess for possible associated injuries.
The most obvious area of pain and tenderness is usually the most structurally significant. However, it may mask other more subtle injuries that should be detected by a more thorough global examination.
IMAGING AND OTHER DIAGNOSTIC STUDIES
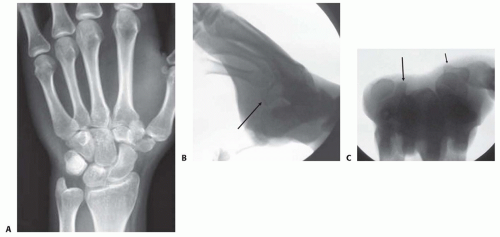
Routine AP, lateral, and oblique views of the wrist and hand are obtained (FIG 3A).
Radiographs of the elbow and forearm are ordered if indicated.
Dynamic radiographic images, including stress and distraction views, help to rule out carpal instability and may determine the ability to obtain closed reduction.
Special views, often best performed with fluoroscopy, help to profile difficult-to-see structures.
The hook of the hamate is evaluated with the carpal tunnel view or the supinated/oblique/radial deviation view with the thumb abducted (referred to as the papillon view) (FIG 3B).
The trapezial ridge is visualized on the carpal tunnel view (FIG 3C).
The pisotriquetral joint is best seen on a 45-degree supinated lateral view of the wrist.
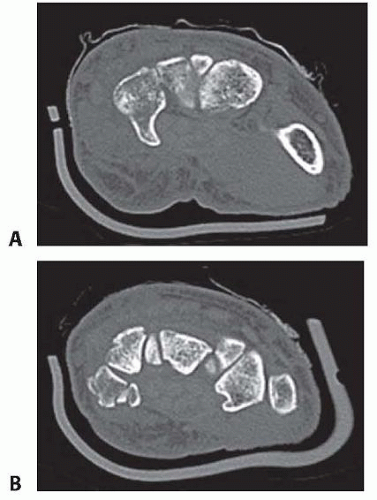
Computed tomography (CT) scans effectively assess osseous detail and will often detect more subtle associated carpal fractures that may be missed on routine radiographs.
CT is considered the imaging modality of choice for confirming a hamate hook fracture if plain films are nondiagnostic.
NONOPERATIVE MANAGEMENT
Isolated carpal bone fractures without associated carpal instability, significant displacement, or intra-articular step-off may be managed nonoperatively.
This usually includes use of a cast or brace for several weeks (usually 4 to 6 weeks) until symptoms have improved, tenderness is resolving, and radiographs are stable.
Short-arm thumb spica casts or splints have been recommended for isolated trapezium and capitate fractures.
The fingers should be left free for gentle range of motion but nothing more than light activities of daily living.
A specific fracture of note is the hamate hook.
These fractures can be treated with cast immobilization if nondisplaced and acute (<1 month).
There is a relatively high rate of symptomatic nonunion, and surgical intervention may eventually be necessary. Close follow-up to determine whether union has occurred is warranted because nonunions may lead to flexor tendon rupture.
Similar to the treatment of the hamate hook, trapezial ridge fractures may be initially immobilized and later excised if symptomatic nonunion develops.
SURGICAL MANAGEMENT
Indications
Indications for surgical management of these fractures include those that significantly involve an articular surface or are structurally destabilizing to the remainder of the carpus, such as a displaced or unstable capitate body fracture.
Other operative indications include those that are true for most fractures, such as open injuries and those requiring nerve, vessel, tendon, ligament, or soft tissue repair.
If stable and near-anatomic reduction of carpal fractures is not possible, primary limited arthrodesis or carpectomy may be indicated.
Because of the unique nature of each carpal bone, more specific indications will be considered for each fracture.
Late reconstructive options include partial or total wrist arthrodesis or proximal row carpectomy for symptomatic arthritic changes.
Trapezial excision with or without thumb metacarpal suspensionplasty may be used for posttraumatic arthritis after trapezial body fractures. Thumb trapeziometacarpal fusion is also an option in these situations but is usually reserved for young heavy laborers.
Total or hemi-wrist arthroplasty for select cases may become a more popular option as techniques improve.
Lunate Fractures
In general, fractures that are of sufficient size and displacement should be reduced and internally fixed.
Fractures that involve the palmar surface of the lunate where stout volar extrinsic wrist ligaments (long and short radiolunate) and vascular conduits (radioscapholunate ligament of Testut) attach should be stabilized.
If the capitate is subluxated volarly relative to the lunate and radius, such as when there is a lunate palmar lip fracture, this must be corrected with reduction and fixation of the lunate palmar fragment.
These fractures are routinely approached palmarly as described in Techniques.
Alternatively, a standard third and fourth interval dorsal exposure (described under Capitate Fractures) can be used if the fracture pattern dictates a dorsal approach and fixation.
Dorsal lip fractures of the lunate typically involve the scapholunate ligament, and if they are displaced, they should be reduced and stabilized to try to prevent scapholunate advanced collapse (SLAC). This is usually performed with small interfragment screw fixation.
Triquetral Fractures
In general, displaced fractures of the triquetral body that are of sufficient size are best treated by open reduction and internal fixation (ORIF).
This can be accomplished through use of pins or screws into the triquetrum alone or in combination with pinning to the lunate or to the hamate as dictated by the fracture.
The triquetrum may be removed in its entirety if it is not amenable to repair, although a volar intercalated segment instability (VISI) pattern may occur if performed in isolation.
An apparently isolated fracture of the triquetrum may in fact be part of a reverse perilunate instability pattern (in which the portal of energy entry is at the ulnar wrist) and may be associated with other fractures and ligament disruptions.
Pisiform Fractures
The pisiform, similar to another sesamoid bone, the patella, most often fractures in a transverse pattern via an indirect avulsion mechanism through the flexor carpi ulnaris (FCU) or in a pattern of comminution from a direct blow.
Virtually all pisiform fractures are treated nonoperatively initially and then excised late if immobilization of the fracture fails to relieve symptoms after 2 or 3 months.
Fractures that are of sufficient size and displacement can be reduced and internally fixed, although this is rarely indicated.
The approach described in Techniques can be used for fixation or excision of the pisiform.
The pisiform is the last carpal bone to ossify, usually by age 12 years, and may have a nonpathologic fragmented appearance before complete ossification.
Hook of Hamate Fractures
If an acute hamate hook fracture is truly nondisplaced, it can be treated nonoperatively initially. If the fracture is displaced or remains persistently symptomatic or nonunited, excision is indicated, even for base fractures (FIG 4A).
ORIF is associated with relatively high complication rates and provides little or no advantage over simple fragment excision.
If ORIF is desired, the hook is exposed as described in Techniques and standard internal screw fixation principles are used.
Hamate Body Fractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree