Surgical Treatment of Calcaneal Fractures
Steven D. Steinlauf
James B. Carr†
Roy W. Sanders
† Deceased.
DEFINITION
An intra-articular calcaneus fracture is an injury that involves the joint surfaces of the calcaneus, usually with displacement.
A fracture-dislocation of the calcaneus occurs when the superior lateral fragment of the posterior facet dislocates from beneath the talus to a position beneath the fibula or interposed between the fibula and the lateral talus. It carries a poor prognosis if treated nonoperatively. Therefore, all patients with this injury should be treated operatively, unless their medical condition precludes surgery.
“Soft tissue” damage refers to the injury to the skin, adipose, tendinous, muscular, and nerve structures that surround the calcaneus and ranges from mild bruising to near-amputation in open fractures.
Fracture blisters and varying degrees of skin contusion occur most commonly.
“Wrinkle sign” refers to the skin wrinkles that appear when the injury swelling response is resolving.
A primary fracture line is one that occurs early in the mechanism of the calcaneal fracture. There are two that occur, and, if their pathogenesis is understood, this can explain the majority of the pathology observed. This will be defined further in the Pathogenesis section.
Minimal-incision surgery refers to all surgical approaches other than the extensile lateral approach.
Anterior process fractures are injuries involving only the anterior portion of the calcaneus. When nondisplaced, they can be treated nonoperatively. Displaced fragments usually require surgery.
A fibular rim fracture represents an avulsion of the superior peroneal retinaculum and is indicative of peroneal tendon instability.
ANATOMY
The calcaneus is the largest bone in the foot. It has a complex shape that makes exact surgical reconstruction difficult.
The calcaneus functions to transmit weight-bearing forces of the leg into the foot.
The articular facets of the calcaneus combined with the corresponding facets on the talus form the subtalar joint. This joint along with the calcaneocuboid joint has a shock absorber function, thus allowing the foot to accommodate to variations in terrain.
The four articular facets of the calcaneus include posterior, anterior, middle, and cuboid. Exact articular alignment is required for full function of this four-joint complex.
The internal structure of the calcaneus reflects its weightbearing role.
There is particularly dense trabecular bone in the juxtaarticular regions, especially below the posterior facet (the thalamic trabecular system).
The tendo Achilles insertion also has dense trabecular bone.
There exists a normal area of relatively little trabecular bone directly below the angle of Gissane called the neutral triangle. For this reason, filling this area with bone graft after fixation of a calcaneus fracture is rarely necessary.
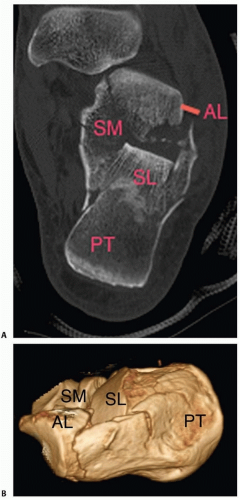
Cortical bone of 3 to 4 mm in thickness occurs in the superomedial region (sustentaculum area) and in the superolateral strut of bone that runs between the cuboid and posterior facets (anterolateral fragment). These regions of cortical bone will come into play when discussing the internal fixation of the calcaneus (FIG 1).
The soft tissues of the calcaneus are easily damaged by trauma. This is especially true in the case of displaced tongue and tuberosity fractures, which can lead to pressure necrosis of the posterior soft tissue. Management of this injury component is essential to avoid iatrogenic surgical complications. The peroneal tendons traverse the retrofibular groove and are located on the lateral aspect of the calcaneus. The sural nerve courses along the lateral calcaneus and can be injured during any lateral exposure of the calcaneus.
The blood supply to the lateral soft tissues of the calcaneus includes the lateral calcaneal artery, the lateral malleolar artery, and the lateral tarsal artery.
In both the extensile lateral exposure and the sinus tarsi approach, the lateral calcaneal artery is at risk for injury.
The lateral calcaneal artery must be preserved to prevent wound healing problems at the apex of the extensile lateral approach.
PATHOGENESIS
Despite the seemingly infinite varieties of fractures that occur, stereotypic fracture lines, fragments, and displacements can be recognized.
The calcaneus is fractured by a combination of shear and compression forces generated by the talus descending on the calcaneus.
Two primary fracture lines occur.
The first occurs in the angle of Gissane and divides the calcaneus into anterior and posterior fragments. It can split either the middle or anterior facet, and the fracture continues on the lateral wall in an inverted Y shape (FIG 2A,B).
The second fracture divides the calcaneus into medial and lateral halves and shears the posterior facet into two or more fragments.
As the talus continues to compress the calcaneus, the lateral half of the posterior facet is impacted into the body of the calcaneus, with the recoil producing a stepoff in the posterior facet.
This same fracture line commonly continues into the cuboid facet and, in combination with the first primary fracture line, produces the anterolateral fragment and superomedial fragment.
In this way, these two fracture lines produce fracture components that include the superomedial fragment, anterolateral fragment, posterior facet, and tuberosity.
The posterior facet is fractured into a superolateral fragment, occasional central fragments, and a portion connected to the sustentaculum tali (the superomedial fragment).
The portion connected to the sustentaculum tali is often referred to as the constant fragment because of the fact that it is rarely displaced to a significant extent. However, a recent study has demonstrated that the “constant fragment” frequently has some displacement and fracture lines.
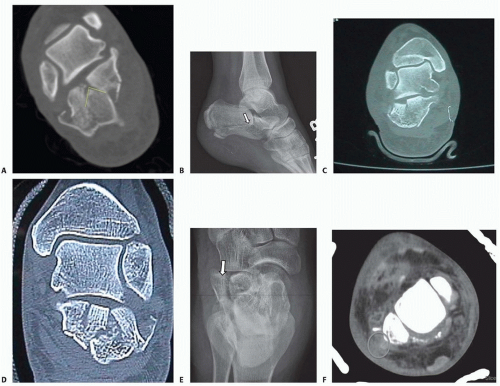
Characteristic displacements of these components occur.
The tuberosity is driven up between the pieces of the posterior facet, can tilt into valgus or varus, and is usually translated laterally. The tuberosity acts as a wedge that prevents reduction of the posterior facet (FIG 3A).
The lateral posterior facet fragments are impacted and rotated plantarly into the body of the calcaneus (FIG 3B).
The posterior facet breaks into one of three patterns, which form the basis of the Sanders classification:
Sanders II: two main pieces (FIG 3C)
Sanders III: three main pieces (FIG 3D)
Sanders IV: multifragmentary
The superomedial fragment retains alignment to the talus by means of its ligamentous attachments but can be subtly displaced by overlap with the anterior portion of the calcaneus. This overlap occurs along the primary fracture line that occurs in the sinus tarsi.
The anterolateral fragment displaces superiorly a variable amount. It typically extends into the cuboid facet, with varying degrees of displacement (FIG 3E).
The lateral calcaneal wall is displaced outward in the area of the trochlear tubercle. This, in combination with tuberosity translation, accounts for the heel widening and peroneal impingement that occur.
In certain cases with significant lateral wall blowout, especially high-energy open fractures, the peroneal tendons will dislocate and may require stabilization (FIG 3F).
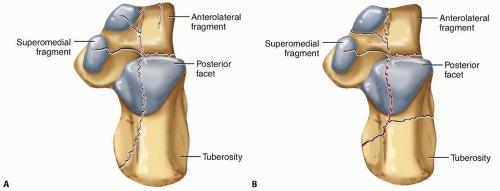
The first fracture types recognized were the joint depression and tongue-type patterns, which are readily identified on a lateral heel radiograph.
The tongue fracture maintains a connection between the tuberosity and the posterior facet, whereas the joint depression separates the fractured joint surface from the tuberosity (FIG 4A,B).
Because of this anatomy, certain tongue fractures have a large portion, or even the entire posterior facet, in continuity with the tuberosity (AO Orthopaedic Trauma Association [AO-OTA] 73 C1). Thus, reduction of the tuberosity will reduce indirectly the posterior facet and restore the angle of Böhler. This particular pattern is well suited for small incision or percutaneous techniques (FIG 4C,D).
Tuberosity fractures involve the insertion of the Achilles tendon. They do not involve the posterior facet.
Secondary to pressure on the skin, tuberosity and tongue fractures will frequently lead to skin breakdown. Therefore, they must be treated in an emergent manner (FIG 4E,F).
Reduction of a joint depression pattern is best performed with an open reduction.
NATURAL HISTORY
An intra-articular fracture of the calcaneus is a serious injury that will diminish foot function.
Nonoperative treatment is with early motion and delayed weight bearing 6 to 8 weeks after injury. This method has the least chance of iatrogenic injury.
In a classic review by Lindsay and Dewar, only 17% of patients had no foot symptoms with long-term follow-up.
The loss of ability to perform manual labor is common, with an average time off work of 4 to 6 months for laborers.
Loss of subtalar motion to varying extents will occur.
Tibiotalar impingement and anterior ankle pain can be produced if the crush deformity is severe enough, leading to settling of the talus into the body of the calcaneus.
It can take 18 to 24 months for the foot symptoms to maximally improve after this injury. Most improvement occurs in the first 12 months.
The key concept here is that patients who continue to improve symptomatically can be observed until maximum improvement occurs.
A recent randomized, prospective study found that the need for late subtalar arthrodesis is five to six times greater if nonoperative treatment is used on all injuries. The overall rate was approximately 17%.
If a subtalar fusion is used to treat posttraumatic arthrosis after a calcaneus fracture that was treated without surgery and allowed to go on to a malunion, the outcome is not as favorable as a subtalar fusion performed after a previous open treatment and internal fixation of the calcaneal fracture.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history is typically one of a fall or vehicle crash. However, calcaneal fractures can occur and are frequently misdiagnosed after minor trauma in older osteoporotic patients and in diabetics with neuropathy.
Important risk factors for operative treatment complications include smoking, diabetes, peripheral vascular disease, and steroid use.
The foot and ankle are visually inspected.
Swelling is graded as mild, moderate, or severe.
Operative treatment in the face of severe soft tissue swelling is prone to wound healing complications.
Fracture blisters are graded as fluid-filled or bloodfilled. If unhealed, fracture blisters are a source of skin bacterial colonization. Blood-filled blisters denote a deeper dermal injury.
Skin contusion is noted.
If present, the wrinkle sign is noted. It means the swelling is resolving and surgical incisions are less likely to experience complications.
Open wounds are noted, and if present, represent a surgical emergency.
The physician palpates the foot and ankle, looks for spine injuries or ipsilateral fractures, and performs a secondary survey for other injuries.
Spine injuries are said to accompany up to 10% of all calcaneal fractures.
The physician assesses for compartment syndrome. Look for pain with passive flexion and extension of the toes, significant foot swelling, and elevated compartment pressure measurements (pressures within 30 mm Hg of diastolic pressure).
Compartment syndrome can occur in 5% to 10% of all calcaneal fractures.
The physician performs a neurologic examination to check the sensory function of the foot and toes, including light touch and pinprick.
Calcaneal fractures, especially fractures with open wounds medially, can damage the posterior tibial nerve and vessels.
IMAGING AND OTHER DIAGNOSTIC STUDIES
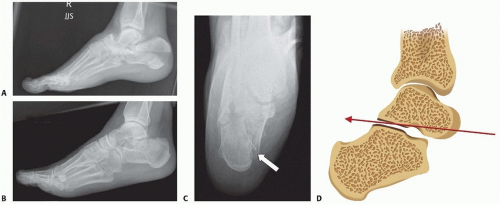
Anteroposterior (AP) and lateral (FIG 5A,B) foot radiographs are the initial screening study.
The axial (Harris) view should also be obtained (FIG 5C). This view will demonstrate the medial wall and show the relation of the superomedial fragment to the tuberosity.
Broden views are radiographs that focus on the subtalar joint. They are taken with the foot internally rotated, and the x-ray beam angled to varying degrees cephalad (FIG 5D,E). By using different degrees of cephalad angulation, different parts of the posterior facet may be imaged.
They are best used intraoperatively to judge the reduction of the posterior facet and the medial wall of the calcaneus.
Three views of the ankle are also helpful. The AP and mortise views can demonstrate fibular rim fractures (indicative of peroneal instability) and fracture-dislocations (superolateral fragment may be displaced into the lateral gutter) (FIG 5F,G).
If a fracture appears to be nondisplaced or minimally displaced but uncertainty exists about the alignment at the joint surface, a computed tomography (CT) scan is ordered.
If the fracture is displaced, a CT scan is needed to define the anatomy and plan surgery (see FIG 3A,C,D,F).
A CT scan with biplanar cuts and reconstructions is needed. This will best delineate the fragments and displacements.
DIFFERENTIAL DIAGNOSIS
Lateral process of talus fracture
Severe ankle sprain
Subtalar dislocation
Stress fractures of the calcaneus can masquerade as a soft tissue disorder of the hindfoot (eg, plantar fasciitis).
NONOPERATIVE MANAGEMENT
The indications for nonoperative treatment include posterior facet displacement less than 2 mm and medical conditions such as peripheral vascular disease or poorly controlled diabetes.
Some surgeons consider smoking a relative contraindication; it certainly predisposes to a higher wound complication rate.
Minimal-incision techniques may be used in this setting with lower risk of wound complications.
Severe fracture blisters or severe soft tissue injury can preclude operative treatment, although open reduction and internal fixation can be performed as late as 4 weeks after injury.
The recommended nonoperative treatment is compression wrapping, early motion, and delayed weight bearing at 6 to 8 weeks after injury. This offers the least iatrogenic risk to the patient while optimizing chances for subtalar motion.
During the first 2 to 3 weeks, the patient should be placed into a cam boot or splint at all times to prevent the development of an equinus contracture.
Once weight bearing is started, the patient continues with range-of-motion exercises.
Strengthening of the foot and ankle muscles is added as fracture consolidation progresses.
A well-cushioned shoe usually offers the best pain relief. Two different shoe sizes may be needed in extreme cases.
A rocker-bottom sole can be added to assist with the toeoff stance phase of gait.
If posttraumatic arthrosis develops, various orthotics can be used in an attempt to relieve symptoms.
Nonoperative treatment is not recommended for calcaneal fracture-dislocations, as a painful deformed foot is practically guaranteed if it is left unreduced.
SURGICAL MANAGEMENT
The displaced intra-articular calcaneal fracture presents a difficult challenge.
Foot pain and stiffness are common even with the best of treatment, and iatrogenic problems such as infection can result in loss of limb in extreme circumstances, and at the least, predispose to a poor result.
Thus, a careful, individualized approach is recommended, with a priority on avoiding iatrogenic problems while attaining an anatomic alignment of the calcaneus.
Indications include displacement of the posterior facet of more than 2 mm and calcaneus fracture-dislocation.
Research shows that certain patient groups, such as those receiving worker’s compensation, are predisposed to a poor result with operative treatment but that does not obviate the benefits of obtaining anatomic foot alignment and lessening the chances of late subtalar fusion.
In addition, not all patients receiving worker’s compensation do poorly, and some do return to gainful employment, although with restrictions in some settings.
The choice of any surgical approach or technique should always have the goal of total anatomic restoration, although extreme comminution can compromise attainment of this goal.
Preoperative Planning
Once operative treatment has been elected, the surgical approach is chosen based on a number of factors, including the surgeon’s training and experience and the pathoanatomy present.
The timing of surgery differs between minimal-incision techniques and the extensile lateral approach. The timing is in general when the wrinkle sign develops and the soft tissue envelope is optimal.
When using a sinus tarsi or similar minimal-incision approach, surgery should be performed before 2 weeks. If the soft tissue envelope is not ready in that time frame, then an extensile lateral approach should be used once the soft tissues are optimal.
The extensile lateral approach can be performed up to 4 weeks after injury if necessary.
The injury pathoanatomy is analyzed first by looking at the posterior facet pattern (Sanders II, III, or IV), displacement, and location of the primary fracture line in the posterior facet.
Fractures that are more medial are more difficult to visualize, and more fragments involving the posterior facet are more difficult to fixate anatomically.
Fractures that separate the entire posterior facet and have a tongue pattern are amenable to percutaneous Essex-Lopresti techniques.
Conversely, joint depression fractures require open reduction of the posterior facet.
A highly comminuted Sanders IV fracture should be treated with open reduction and primary fusion through a sinus tarsi or extensile lateral exposure.
The other fracture components to be analyzed for displacement are the superomedial fragment, anterolateral fragment, and tuberosity. The surgical plan should address each of these pathologies for reduction strategy and fixation.
The typical reduction order is first to correct any superomedial fragment subluxation.
Next, the superomedial fragment is reduced and held to the tuberosity.
The posterior facet is then reduced and fixed.
Finally, the anterolateral fragment is reduced and fixed.
The size and integrity of the superomedial fragment is critical, as fixation techniques largely center on screw placement into its substance. A small or comminuted superomedial fragment makes rigid fixation harder to achieve and may call for alternative techniques.
A significantly displaced superomedial fragment may require a separate medial incision to assist with reduction and fixation.
Restoration of the superomedial fragment to the tuberosity will restore the calcaneal shape and make room for reduction of the displaced posterior facet fragments.
The superomedial fragment may be incarcerated in the sinus tarsi and subtly subluxated. This is recognized by the preoperative CT scan on the sagittal reconstructions and by the lack of congruence of the superomedial fragment with the undersurface of the talus.
Failure to correct this subluxation makes posterior facet reduction very difficult.
The anterolateral fragment should key into location just in front of the reduced posterior facet and restores lateral column length. This is assessed by assuring reconstruction of the hard cortical bone that represents the crucial angle of Gissane.
It can be fixed with either lag screws into the superomedial fragment or a minifragment plate. Some of the perimeter plates have a small extension to pull this fragment into place.
The fixation chosen depends on the approach taken. Fractures splitting the posterior facet will require lag screws inserted from lateral to medial; they range in size from 2 to 4 mm, depending on the fractures present.
Sanders III fractures are converted into two major pieces with the use of countersunk minifragment screws or bioabsorbable pins that fix the intermediate piece to the more medial piece.
The plate chosen depends on the approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree