Surgical Treatment of Acute and Chronic Paronychia and Felons
Jennifer Etcheson
Jeffrey Yao
DEFINITION
An acute paronychia is an infection of the soft tissue fold around the fingernail.
It is the most common soft tissue infection of the hand.
The most common infecting organism is Staphylococcus aureus, although these infections are commonly mixed infections.
A chronic paronychia is characterized by repeated infection and inflammation of the eponychium.
The eponychium becomes thickened and rounded.
This problem often occurs in the setting of repeated and prolonged exposure to water.
The most commonly isolated organisms are Candida albicans, gram-positive cocci, gram-negative rods, and Mycobacterium spp.
Herpetic whitlow is caused by an outbreak of herpes simplex virus in the skin of the finger and can be confused with acute paronychia or felon.
Herpetic whitlow is common in children and medical personnel who come into contact with oral secretions.
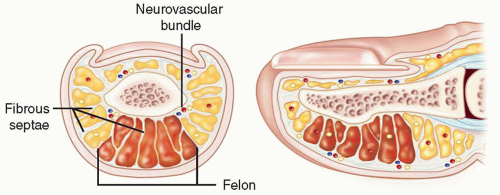
A felon is a tense abscess of the distal pulp of the finger or thumb that involves multiple septal compartments (FIG 1).
ANATOMY
The nail complex consists of the nail bed, nail plate, and perionychium (FIG 2).
The nail plate sits below the proximal nail fold.
The perionychium is the border tissue which surrounds the nail.
The eponychium is the tissue that attaches closely to the nail plate proximally, commonly referred to as the cuticle.
The nail folds consist of skin, which continues underneath the visible edges to form a protective barrier.
The pulp of each digit consists of multiple compartments separated by fibrous septa.
These vertical septa extend from the periosteum of the distal phalanx to the epidermis, lending structural support to the fingertip.
PATHOGENESIS
Acute paronychia results from the introduction of bacteria into the space between the nail fold and the nail plate, either proximally or laterally.
This commonly occurs as a result of a hangnail, nail biting, artificial nails, or an overzealous manicure.
Chronic paronychia results from colonization and infection by organisms that enter the space between the nail plate and the cuticle, eponychium, and nail fold.
Infection may result from repeated exposure to moisture.
This chronic infection and inflammation lead to fibrosis of the eponychium, which, in turn, leads to decreased vascularity of the dorsal nail fold.
This decreased vascularity predisposes to repeated bacterial insults, resulting in the characteristic clinical exacerbations.
Felons often result from penetrating trauma or from bacterial inoculation through the exocrine sweat glands contained within the pulp.
Cellulitis and local inflammation lead to local ischemia, which, in the setting of the closed spaces defined by septa, leads to increased pressure.
Fat necrosis and abscess formation result from the increased pressure, which, in turn, causes a further increase in pressure and, in effect, a compartment syndrome.
NATURAL HISTORY
If acute paronychia is left untreated, an early infection will turn into an abscess along the nail fold.
The abscess may then extend into the pulp space or into the eponychium and then to the opposite side of the nail.
Purulence at the base of the nail may cause ischemia of the germinal matrix, which then may lead to temporary or permanent nail growth arrest.
Herpetic whitlow improves without any intervention in approximately 3 weeks.
Many cases of herpetic whitlow are misdiagnosed as acute paronychia or felon.
Subsequent incision and drainage may lead to secondary bacterial infection.
Chronic paronychia are characterized by induration of the eponychium punctuated by episodes of swelling and drainage.
A felon, if left untreated, may lead to osteomyelitis or septic flexor tenosynovitis.
PATIENT HISTORY AND PHYSICAL FINDINGS
In acute paronychia, the patient will complain of swelling and pain immediately adjacent to the nail.
If an abscess has formed, there may be erythema and purulent drainage.
In chronic paronychia, the patient will present with a chronically indurated and rounded eponychium characterized by repeated episodes of inflammation and drainage.
Herpetic whitlow is characterized by pain and swelling followed by the appearance of multiple vesicular lesions.
The pain typically is out of proportion to the physical findings, and the fingertip is not tense (in contrast to a felon).
A patient with a felon will present with severe throbbing pain, swelling, and a tense fingertip pad.
A felon will not extend proximal to the distal interphalangeal (DIP) joint flexion crease unless it is associated with septic flexor tenosynovitis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs are indicated to rule out osteomyelitis or if a foreign body is suspected.
The diagnosis of herpetic whitlow is confirmed by Tzanck smear, which will show multinucleated giant cells.
Patients suspected of having a systemic illness should have the appropriate laboratory workup.
DIFFERENTIAL DIAGNOSIS