Surgical Techniques for Failed Medial Ulnar Collateral Ligament Reconstruction
Joshua S. Dines
Neal S. Elattrache
Bernard F. Morrey
CHAPTER 28A: FAILED ANTERIOR BUNDLE RECONSTRUCTION
INTRODUCTION
Elbow ulnar collateral ligament (UCL) injury was once considered career ending; however, numerous studies demonstrate that up to 90% of overhead athletes are able to successfully return to competitive throwing activities with the use of modern UCL reconstruction techniques (1,2 and 3). Various complications after UCL reconstruction have been reported including ulnar neuritis, loss of motion, fracture, and retear (3). In the largest series of UCL reconstruction outcomes, Cain et al. reported that 1% of their patients underwent revision UCL reconstruction. As the number of primary UCL reconstructions performed increases, it stands to reason that over the coming years, more revision surgeries will be performed. Previously, we reported on the outcomes of revision UCL reconstruction in 15 patients (4). Only a third of the athletes returned to their previous level of play, and the complication rate approached 40%. Clearly, this is a difficult group of patients to treat. In order to maximize the potential to return these athletes back to their previous level of play, it is important to have a good understanding of why the retear occurred. Additionally, the treating surgeon needs to have a solid knowledge of the variety of UCL reconstruction techniques commonly used as different causes of failure may necessitate different techniques.
DIAGNOSIS
Patients who retear their UCL after reconstruction can present a difficult challenge to the treating physician. Details of the index operation including technique, hardware used, and postoperative care must be obtained by the treating surgeon. This includes evaluation of the index operative report and
imaging when available. In some cases, reevaluation of these records and studies will help define the cause of failure. The technique at index operation will often define the possibilities at revision UCL reconstruction. The most commonly used reconstruction techniques include the figure-of-8 reconstruction, the docking technique, the DANE technique, and the interference screw reconstruction (please see Chapter 27). In many cases, if the ligament tears due to overuse, the same technique used during the index procedure can be repeated. However, if failed reconstruction is due to fracture of the sublime tubercle or humeral medial epicondyle, options are more limited.
imaging when available. In some cases, reevaluation of these records and studies will help define the cause of failure. The technique at index operation will often define the possibilities at revision UCL reconstruction. The most commonly used reconstruction techniques include the figure-of-8 reconstruction, the docking technique, the DANE technique, and the interference screw reconstruction (please see Chapter 27). In many cases, if the ligament tears due to overuse, the same technique used during the index procedure can be repeated. However, if failed reconstruction is due to fracture of the sublime tubercle or humeral medial epicondyle, options are more limited.
A comprehensive physical examination must be performed. In addition to eliciting symptoms of UCL insufficiency, concomitant nerve injury or posteromedial impingement may also be identified as a cause of failure.
Imaging of the elbow joint and soft tissues is mandatory and critical for proper diagnosis. Plain x-ray views including AP and lateral views can be helpful in assessing fracture and tunnel widening, but in most cases, MRI will better define soft tissue failures. CT scans can better delineate the degree of bone loss, which may have more implications with regards to the appropriate treatment (Fig. 28A-1).
SURGICAL TECHNIQUE
Revision UCL Reconstruction Technique
The technique used for revision UCL reconstruction is predicated on both the original technique used and the cause of failure. In cases where the athlete restore their ligament but the bone tunnels remained in good condition, the same technique used in the index procedure can be repeated with a new tendon graft. Details of index reconstruction techniques are discussed in Chapter 27. If one or more of the bone tunnels is compromised, this poses a much more difficult situation (Fig. 28A-2).
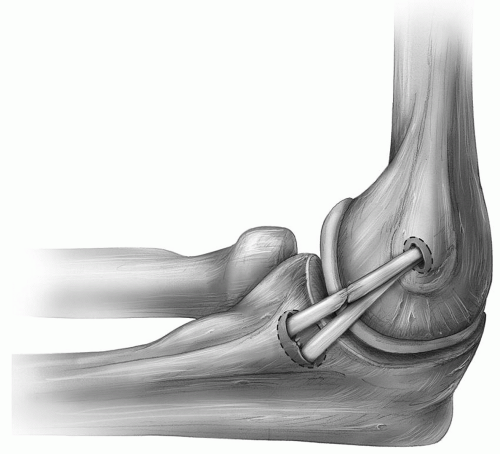 FIGURE 28A-2 The cause of failure can occur either at the humeral tunnel, at the ulnar tunnel (dashed circles), or in the substance of the graft. |
Surgical Approach
Patients are placed supine, and the arm is prepped sterilely on a hand table.
We routinely use a tourniquet for the entire procedure.
Based on preoperative physical exam and discussion with the patient, the graft is harvested. We prefer to use the palmaris (if present) or the gracilis from the contralateral leg (Fig. 28A-3).
If appropriate, the previously used medial incision is made starting proximal to the medial epicondyle and extending distal to the sublime tubercle. At this point, the muscle-splitting approach is used.
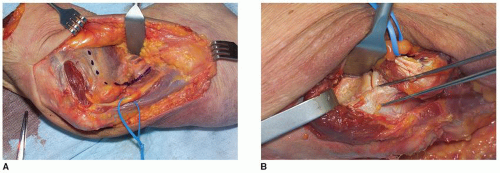
The fibrous raphe along the anterior margin of the flexor carpi ulnaris is split longitudinally, and the underlying muscle is divided exposing the UCL (Fig. 28A-4).
The ulnar nerve is identified but is not moved unless symptomatic.
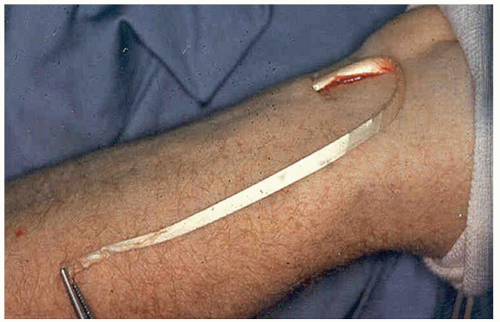 FIGURE 28A-3 Since this is a reoperation, the palmaris longus, shown here, is usually not available for a reconstruction, in which case a gracilis autograft is harvested from the contralateral leg. |
Note: In patients with concurrent flexor-pronator tears, a flexor-elevating approach can be used that allows debridement and repair of the torn tendons while providing excellent exposure of the UCL.
Ulnar Bone Loss In cases with compromise of the bone bridge on the ulna, two viable options can be used: DANE technique and suspensory button fixation (1,5). The DANE technique relies on interference screw fixation on the ulna with the docking technique proximally at the humerus.
The previously harvested graft is folded onto itself, and a running, Krackow stitch is placed in the folded end for approximately 25 mm (Fig. 28A-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree