Surgical Technique for Knee Dislocations
Bryan T. Kelly
Struan H. Coleman
Russell F. Warren
INDICATIONS/CONTRAINDICATIONS
Knee dislocations occur whenever the articular surfaces of the distal femur and proximal tibia displace completely from one another (Fig. 23-1). Dislocations are most usefully described according to the associated degree of local soft-tissue injury (e.g., closed or open grade I, II, III), and the primary direction of displacement. The direction of a particular knee dislocation is designated according to the direction of displacement of the tibia with respect to the femur (6,7). Anterior, posterior, medial, lateral, and rotatory dislocations have been described. Straight anterior or posterior dislocations are the most commonly reported. Other forms of dislocation (medial, lateral, or rotary) are far less common and are often combined with anterior or posterior dislocation (6,7,9,13,14,15).
The majority of reported dislocations of the knee occur in association with motor-vehicle accidents. The high velocity and ultra-high-force nature of this type of trauma often leads to associated head and thoraco/abdominal injuries of higher priority and, not uncommonly, to rapid mortality. Of primary importance in the multiple trauma victim is the immediate treatment of life-threatening conditions. Once these issues have been properly addressed, attention should be given to a dislocated knee.
We believe it is appropriate to attempt immediate closed reduction and immobilization of all knee dislocations if possible. The massive displacement of the bony architecture that occurs during dislocation causes extensive disruption of the joint capsule and ligaments. Usually, at least three major ligaments and the posterior joint capsule are damaged. Therefore, the degree of instability is usually so severe that gentle manipulation will easily achieve reduction. Once reduced, a thorough evaluation of the neurologic and vascular status of the injured extremity is critical. Adequate determination of pedal pulses, in addition to ankle-brachial indexes bilaterally, should be performed routinely in this setting. Failure of early diagnosis of vascular injuries has resulted in extremely high amputation rates, up to 90% in some series (2,4).
In some medial dislocations, it may be impossible to reduce the knee by closed manipulation, since the medial femoral condyle may have “button-holed” through the medial joint capsule and retinaculum. These cases require open reduction. Furthermore, the joint is often rendered so unstable in medial and lateral dislocations that closed reduction, once achieved, is very difficult to maintain. Under these circumstances, after a careful vascular and neurologic examination, the knee should be immediately immobilized in a brace, cast, or splint and a radiographic evaluation made of the reduction, with adjustment if required. In some cases placement of an external fixator is required to maintain the reduction. Immobilization in a significant degree of flexion (45 degrees or more) may be needed to achieve and maintain an adequate reduction. In contrast, reduction is often relatively easy to maintain after manual reduction of straight anterior or posterior dislocations in which the medial and lateral soft tissues have simply been “peeled off” anteriorly or posteriorly in a longitudinally intact sleeve of tissue. When these tissues are reduced to their original positions, they tend to provide enough stability to maintain adequate reduction with relatively minimal external support.
NONOPERATIVE TREATMENT
In closed dislocations, without intra-articular fracture, and where a good reduction can be easily maintained in a cast or brace, nonoperative treatment with early range of motion (ROM) therapy may achieve an acceptable functional outcome. However, if this course is chosen, frequent radiographic assessment of the adequacy of the reduction must be performed during the first several weeks. This is because posterior subluxation will often lead to a poor outcome, and later attempts at surgical correction of this problem will have a low success rate once the soft tissues have “matured,” creating a fixed, posteriorly subluxed position. A hinged external fixator may be used to prevent posterior subluxation but allow for progressive ROM in cases where the reduction is difficult to maintain.
Delayed Arthroplasty or Arthrodesis
In older patients with massively comminuted intra-articular fractures, the most prudent course of action may be to simply immobilize the knee in a position of acceptable alignment for a period of time, during the initial phase of bone and soft tissue recovery and healing, before performing a primary knee arthroplasty or arthrodesis as the definitive surgical treatment. Immobilization may take the form of a cast, brace, or external fixator device.
PREOPERATIVE PLANNING
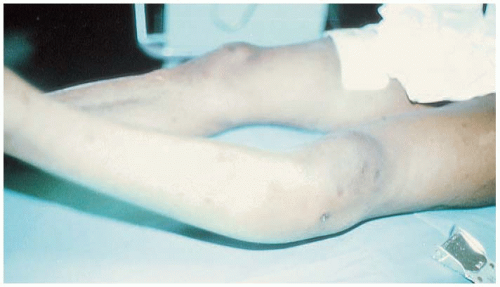
It is of the utmost importance to assess the condition of the local skin and soft tissues (Fig. 23-2), neurologic status, and, particularly, the vascular status of the involved extremity, both initially and at frequent intervals after initial evaluation. Accurate monitoring of the pedal pulses is critical. Determination of the status of the knee ligaments, although of interest, is an issue of lower priority early after a knee dislocation. The evaluation and early management of a dislocation should be done in a manner that does not jeopardize or hinder the evaluation of the vascular status of the limb.
After the initial reduction, the factors that we consider most important in making surgical decisions about dislocations of the knee include:
The adequacy of the reduction. If closed reduction is impossible because of interposed soft tissue, open reduction should be performed at the earliest opportunity (within several hours after dislocation). If an adequate closed (or open) reduction can be achieved but cannot be maintained, the surgical repair of damaged ligaments should be performed as soon as the patient’s general condition and the condition of the local soft tissues permit (from several hours or days to 2 weeks after dislocation). If the interval between injury and definitive fixation is anticipated to be a prolonged period, the use of an external fixator may be employed.
The condition of the soft tissues. In open injuries, surgical irrigation and debridement should be performed at the earliest opportunity (within several hours after injury). In most of these cases, and in closed dislocation with severe blunt injury to the local skin and soft tissues, attention to surgical stabilization of the knee should be delayed until the condition of these tissues improves to a level appropriate to the performance of extensive open-knee ligament surgery (within several days to 2 weeks after injury).
The status of arterial blood flow to the distal extremity. The impairment of popliteal arterial blood flow is the most common and severe complication of knee dislocations, with a reported incidence ranging from 5% with low energy trauma to 40% with high energy, anterior or posterior dislocations (2,5,15). Our plans for surgery are guided by the following criteria. The absence of pulses at the ankle and foot is an absolute indication for immediate surgical exploration and repair of the popliteal artery. Arterial blood flow must be re-established within 6 hours after the initial injury; otherwise, severe ischemic effects leading to amputation are inevitable in a great majority of cases. The absence or diminution of pulses obviates the need for preoperative angiography in favor of immediate exploration and repair of the popliteal artery, with intraoperative angiography, in this setting, reserved for identifying the site of injury. Patients with normal pulses may be monitored by careful vascular examination. In a study by Treiman et al (16), of 115 unilateral knee dislocations, the incidence of popliteal artery injury was 23%. However, there was a 79% incidence of popliteal injury associated with abnormal pedal pulses. In the remaining 86 patients with normal pulses, the arteriogram was normal in 77, showed spasm in 5 patients, and revealed an intimal flap in 4 patients. None of the patients with normal pedal pulses required arterial repair. Hollis et al (4) also concluded that routine arteriography is unnecessary in patients with a normal physical examination after reduction of the knee dislocation. The role of magnetic resonance angiography in making the diagnosis of a vascular injury in this setting remains to be determined, but appears to be particularly useful for evaluating those patients with extensive soft tissue injury and normal pulses when surgery is being planned (10,11).
In approaching soft-tissue reconstruction in a dislocated knee, the surgeon should consider and prepare options for repairing and grafting any or all of the main stabilizers of the knee, including the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament
(MCL), lateral collateral ligament (LCL), popliteus tendon and popliteofibular ligament, patellar tendon, patella, and quadriceps tendon. These may include autografts from the injured or contralateral knee, allografts and, very occasionally, ligament augmentation devices (LADs). The surgeon should assess the availability of these resources and obtain appropriate informed consent for their use before taking the patient to the operating room.
(MCL), lateral collateral ligament (LCL), popliteus tendon and popliteofibular ligament, patellar tendon, patella, and quadriceps tendon. These may include autografts from the injured or contralateral knee, allografts and, very occasionally, ligament augmentation devices (LADs). The surgeon should assess the availability of these resources and obtain appropriate informed consent for their use before taking the patient to the operating room.
If vascular reconstruction has been performed, the use of a tourniquet may be contraindicated. Intraoperative fluoroscopy is often helpful in the placement of bone tunnels, which may be required for reconstruction of the PCL. Intraoperative plain radiographs should also be available to assess the correction of posterior subluxation before the conclusion of surgery.
Inspection of the menisci and articular surfaces, and preparation of the intercondylar notch for ligament reconstruction, is most easily and thoroughly accomplished arthroscopically. However, capsular disruption may preclude routine arthroscopy because of excessive extravasation of fluid into the soft tissues. Under these circumstances, we usually favor a brief arthroscopic inspection, with low-pressure flow and systemic wrapping of the calf, before proceeding to an open approach. We have also found “dry” or “semi-wet” arthroscopy, with intermittent fluid flushes, to be a viable option in inspection, debridement, and reconstruction in the intercondylar notch. The surgeon should be prepared, however, to perform the entire procedure in an open fashion, if necessary, and if arthroscopy is used, an awareness of fluid extravasation is paramount. Significant fluid extravasation may make open procedures (e.g., MCL and LCL reconstruction) more difficult, and can lead to a lower-leg compartment syndrome.
SURGERY
Technique
The patient is placed supine on an operating table that is adjustable to allow variable amounts of flexion at the hip and knee. We position the patient longitudinally on the table in such a way that the patient’s knee-flexion crease is just distal to the distal flexion joint of the table, so that the foot of the table may be dropped to allow up to 90 degrees of knee flexion during the surgical procedure. If available, an operating table that has these features and is also designed for use with an image intensifier is optimal. Our preferred method of anesthesia is continuous lumbar epidural blockade. In our experience, this has provided excellent, adjustable, and long-lasting muscle relaxation and pain relief.
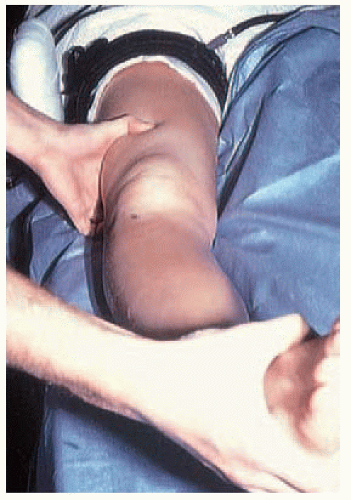
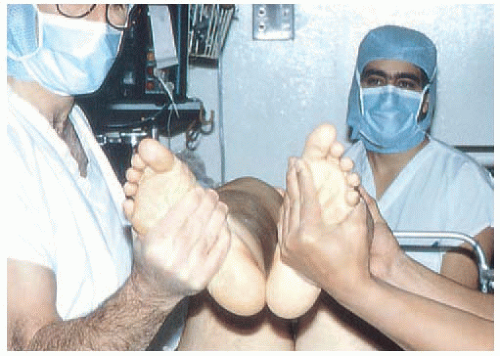
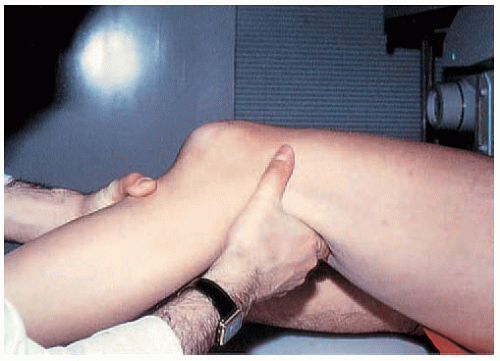
The first event after reaching an appropriate level of anesthesia should be a thorough examination of the knee. This should be done before prepping and draping the patient to allow easy manipulation of the knee and comparison with the opposite knee. A thorough assessment should be made of the status of the ACL, PCL, MCL, LCL, and posterolateral corner (Figs. 23-3, 23-4, 23-5 and 23-6).
If possible, a tourniquet is then placed around the upper thigh at as high a level as possible, over a layer of protective cast-padding material. We then seal off the tourniquet area with adhesive plastic drapes to avoid the skin irritation occasionally seen when Betadine (povidone/iodine) solution seeps under the tourniquet and remains there during periods of tourniquet inflation. The entire extremity is then prepped by first scrubbing with Betadine scrub solution and then painting with concentrated-Betadine swabs. We seal off the lower leg and foot with an adhesive plastic dressing. Further standard draping is done with sterile paper drapes. If the use of contralateral autografts is anticipated, the opposite leg is also prepped and draped in the same manner.
A separate sterile table is set up away from the primary surgical field, at which an assistant is provided with the appropriate instruments for preparing graft material. If allografts are to be used, an assistant may begin graft preparation simultaneously with the start of the surgical procedure on the knee.
If arthroscopy is to be performed as part of the procedure, it is often done first. We occasionally harvest an autograft from the middle third of the patellar tendon, before the arthroscopic examination, to allow the assistant to prepare the graft while the rest of the procedure continues. We avoid using the tourniquet during arthroscopy by adding 1 mg of epinephrine to each 3,000-mL bag of arthroscopic irrigation solution, and have been quite satisfied with the level of hemostasis and clarity of visualization this affords. Arthroscopy begins with a routine visual inspection of the entire knee in a predetermined sequence as follows: suprapatellar pouch, patella, lateral gutter, popliteus recess, femoral trochlea, medial gutter, medial compartment, intercondylar notch and ligaments, and lateral compartment. Once the visual inspection is complete, we proceed to the required repairs (Fig. 23-7).
At this point, we may discontinue arthroscopy to harvest patellar tendon, semitendinosus, and gracilis grafts, as necessary. After the graft harvest is completed, we resume arthroscopy to perform any required meniscal work, as well as a debridement and preparation of the intercondylar notch. If fluid extravasation precludes further arthroscopy, we proceed to an open approach.
All remnants of ruptured ligaments, if unusable in the reconstruction, are removed. Enough bone is also removed from the roof and sides of the intercondylar notch to allow unencumbered movement of the knee so as to prevent impingement of the intended grafts.
At this stage, we prepare the tibial attachment site of the PCL arthroscopically using a posteromedial portal for visualization while debridement is performed through an anterior portal and the intercondylar notch (Fig. 23-8).
As previously mentioned, extensive capsular injury may compromise or even contraindicate arthroscopy in a fluid medium. If fluid loss is marked, the repair medially may be performed before addressing the ACL or PCL to allow better arthroscopic evaluation and ligament reconstruction. For open reconstruction of the knee ligaments, we have been satisfied with the utility of a long, oblique skin incision that courses over the front of the knee in a proximal-lateral to distal-medial direction (Figs. 23-9 and 23-10). With appropriate extension of the incision and the elevation of skin flaps, this type of incision allows access to all aspects of the knee.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree