The patella plays a crucial role in the extensor mechanism to increase the mechanical advantage of the quadriceps. Fractures can be classified based on displacement, comminution, and fracture pattern, which often guide treatment. Modern treatment options include internal fixation using tension bands with Kirschner wires or cannulated screws, lag screw fixation, partial patellectomy, and rarely total patellectomy. Nondisplaced, closed patellar fractures or fractures with less than 2-mm articular steps can be successfully treated conservatively. Open fractures, articular step of 2 mm or greater, and loss of knee extension are indications for surgical intervention.
Key points
- •
The patella is a crucial component of the extensor mechanism.
- •
Modern surgical techniques provide good results with proper indications.
- •
Management of patella fractures depends on the fracture morphology.
- •
Symptomatic implants often lead to additional surgery.
- •
New techniques aim to reduce implant complications.
Introduction: nature of the problem
The patella plays a crucial role in the extensor mechanism to increase the mechanical advantage of the quadriceps. Forces up to 5 times the body weight have been recorded from the extensor mechanism; the patella displaces the quadriceps tendon-patellar tendon link away from the axis of knee rotation, effectively increasing the moment arm of the quadriceps.
Every year, roughly 1 in every 100 fractures will involve the patella. Fractures can be classified based on displacement, comminution, and fracture pattern and often involve concurrent injury to the proximal tibia, distal femur, or knee ligaments. Although conservative treatment remains an option, open reduction and internal fixation (ORIF) and/or partial patellectomy have emerged as the preferred treatment options. Numerous biomechanical and long-term studies highlighted the importance of the patella and tempered enthusiasm for total patellectomy as the treatment of choice for all patella fracture. In the 1950s, the Arbeitsgemeinschaft für Osteosynthesefragen (AO) introduced and promoted the use of anterior tension band principles for patella fracture fixation. Subsequent studies validated its stability. Modern treatment options include internal fixation using tension bands with Kirschner (K) wires or cannulated screws, lag screw fixation, and partial patellectomy, all with reasonably good clinical results.
Introduction: nature of the problem
The patella plays a crucial role in the extensor mechanism to increase the mechanical advantage of the quadriceps. Forces up to 5 times the body weight have been recorded from the extensor mechanism; the patella displaces the quadriceps tendon-patellar tendon link away from the axis of knee rotation, effectively increasing the moment arm of the quadriceps.
Every year, roughly 1 in every 100 fractures will involve the patella. Fractures can be classified based on displacement, comminution, and fracture pattern and often involve concurrent injury to the proximal tibia, distal femur, or knee ligaments. Although conservative treatment remains an option, open reduction and internal fixation (ORIF) and/or partial patellectomy have emerged as the preferred treatment options. Numerous biomechanical and long-term studies highlighted the importance of the patella and tempered enthusiasm for total patellectomy as the treatment of choice for all patella fracture. In the 1950s, the Arbeitsgemeinschaft für Osteosynthesefragen (AO) introduced and promoted the use of anterior tension band principles for patella fracture fixation. Subsequent studies validated its stability. Modern treatment options include internal fixation using tension bands with Kirschner (K) wires or cannulated screws, lag screw fixation, and partial patellectomy, all with reasonably good clinical results.
Indications/contraindications
Indications for treatment of patellar fractures are largely determined by the type of fracture encountered. However, the goals of treatment remain the same: (1) restoration of the extensor mechanism and (2) maintenance of a congruous articular surface. Thus, the literature often has focused on treatment type rather than fracture type.
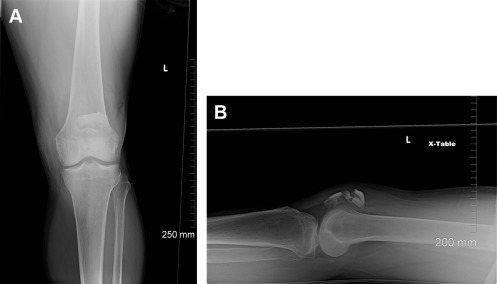
Conservative Management
Nondisplaced, closed patellar fractures, including stellate, transverse, and vertical, or fractures with less than 2-mm articular steps can be treated conservatively. Stellate, transverse, and vertical fractures of the patella often spare the medial and lateral retinaculum, maintaining knee extension. Transverse fractures can present with significant displacement, such as 4 to 5 mm. However, if patients are able to extend their leg actively, the retinaculum is likely intact and can be managed conservatively. Because the distal portion of the patella is extra-articular, fractures of the inferior pole can also be managed conservatively.
Conservative management usually includes weight-bearing-as-tolerated (WBAT) ambulation with the knee in fixed extension supported by a splint, knee immobilizer, or hinged knee brace. At 2 to 3 weeks, patients begin passive range of motion (PROM) from 0° to 30°, increasing the arc of motion by 15° per week. At approximately 8 weeks, patients should have nearly a full PROM of the knee and can begin advancing WBAT without immobilization.
Surgical technique/procedure
Surgical Indications
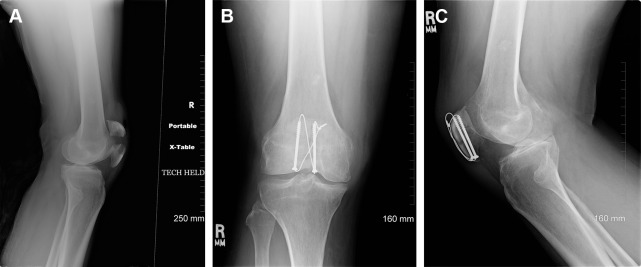
Indications for surgery include open fracture, articular step of 2 mm or greater, and loss of knee extension ( Fig. 1 ). Comminuted stellate fractures typically present with intact retinaculum; however, because of the articular incongruity, surgical intervention may be recommended ( Fig. 2 ). Highly comminuted and displaced fractures can present as transverse fractures with massive comminution or stellate fractures with massive diastasis. These injuries are often open.
Preoperative Planning
Standard radiographic views for the patella fractures include anteroposterior and lateral radiographs. The patella position and height are readily assessed with this view. A lateral radiograph will often provide an excellent survey of the fracture as well as an opportunity to determine patellar height ( Fig. 3 A, B ). Most reliably, this is accomplished using the Insall technique. A computed tomography scan can provide more detailed information regarding fracture character and articular step, though it is not routinely obtained (see Fig. 3 C–E).

Prep and Patient Positioning
In addition to the implants necessary for fixation, a small-fragment instrument and implant set and pointed bone reduction forceps can be useful. Additionally, wire instruments, such as tensioners, wire forceps, and crimpers, can be helpful ( Fig. 4 ). Angiocatheters can provide a convenient conduit for passing suprapatellar and infrapatellar wires. Patients are placed supine on the operating table with an optional tourniquet placed on the proximal thigh. Care should be taken to ensure that the tourniquet is placed as high as possible and inflated during knee flexion to avoid quadriceps trapping.
Surgical Approach
A midline longitudinal or lateral para-patellar incision is most frequently used. This approach facilitates reduction and is safe for future arthroplasty. In addition, this approach avoids the saphenous branch of the femoral nerve, which safely lies medial to the incision. Several case series promote arthroscopically assisted reduction and fixation of minimally displaced patellar fractures. However, this technique may not be appropriate for highly comminuted or displaced fractures.
Surgical procedure (steps)
Cannulated screw fixation with supplemental wiring
- 1.
A midline longitudinal incision is made through skin and bursa.
- 2.
The fracture edges are cleaned, and the joint is irrigated to remove debris.
- 3.
The K wire is passed in a retrograde fashion through the proximal fragment starting within the fracture line, roughly 5 mm from the articular surface of the patella, and at the junction of a line separating the patella into thirds. The K wire is driven proximally until flush with the fracture edge.
- 4.
A second K wire is passed in a similar fashion parallel to the first K wire.
- 5.
The fracture is reduced and held with Weber or patellar reduction clamps.
- 6.
K wires are advanced across the fracture and out through the patellar tendon.
- 7.
A cannulated drill is used to drill over the K wires followed by placement of 3.5- or 4.0-mm cannulated screws.
- 8.
An 18-gauge wire is passed through one cannulated screw and then through an 18-gauge angiocatheter through the patellar tendon. The wire is then loop through the other screw in the opposite direction followed by passing it through the quadriceps tendon. The wire is then tightened on the dorsal surface of the patella.
- 9.
Reduction of the articular surface is examined with the knee in extension by palpation through the retinacular rent and by fluoroscopy.
- 1.
Postoperative Care
Following anatomic reduction and stable fixation of the patellar fracture, patients are encouraged to begin careful and protected motion. Use of a continuous passive motion machine can be used; however, caution is recommended to prevent failure of fixation. Starting on postoperative day 1, patients are allowed to begin quadriceps isometric exercises. All drains in place are removed on postoperative day 2. Patients can then be placed in a removable knee brace locked in extension and unlocked for physical therapy targeting range of motion. Physical therapy is instructed not to begin these exercises until the wound is completely healed, typically at 2 to 3 weeks following surgery.
At 6 weeks, radiographic evidence of healing is available and progressive resistance exercises are introduced. Gradually, the brace is weaned and can be discarded at 3 months when fracture healing can be confirmed. Physical therapy may be continued up to 6 months following surgery, at which point restrictions on sport are lifted.
The protocol is modified if operative fixation failed to produce a stable construct. A hinged knee brace is locked in extension, with isometric quadriceps strengthening exercises delayed until 2 weeks following surgery. Flexion is limited to the degree determined during surgery. Active flexion exercises are restricted until there is evidence of fracture healing. Although weight bearing in full extension is permitted as tolerated, weight bearing in flexion is deferred until fracture healing is confirmed. Under these circumstances, it is important to counsel patients that these precautions to protect the repair often lead to stiffness and weakness. Once fracture healing is confirmed, aggressive physical therapy is permitted to improve range of motion and strength.
Outcomes
Nondisplaced fractures treated conservatively have good outcomes, defined as no arthrosis, weakness, or pain as well as full range of motion. Boström examined 422 patellar fractures, of which 219 were treated nonoperatively. All had less than 4-mm articular incongruity, and 98% exhibited good or excellent results. Other studies agree with these findings.
Surgeons often allow the type of fracture to dictate the surgical technique used. Therefore, many report results based on fracture type and surgical technique, seldom with direct comparison. Modified anterior tension band wiring currently gives the best results, with 85% of patients reporting good or excellent outcomes according to 2 studies providing a combined cohort of 59 patients. The same studies also compared it with cerclage wiring, showing only 19 of 31 (61%) with good or excellent outcomes. Additionally, Weber and colleagues reported the biomechanical superiority of tension band wiring compared with cerclage wiring. However, the high occurrence of symptomatic fixation implants has spurred the development of novel constructs. Chen and colleagues proposed a transosseous suturing technique indicated for transverse or comminuted fractures of the patella. They reported good results with lower complication rates compared with tension bands; however, their case series was only 25 patients. Hoshino and colleagues compared the use of K wires with cannulated screws in the tension band construct. They found cannulated screws to have a higher rate of failure (7.5% vs 3.5%) but a much lower rate of elective implant removal (23% vs 37%). Other constructs that have been biomechanically tested include locking plate with tension band, fixed-angle plate, and compressive cannulated locking bolt and nut, though rigorous studies evaluating clinical results have not been published. A recent Cochrane review identified 5 randomized controlled trials and concluded that evidence overall is limited for guiding the management of patellar fractures in adults.
More recent reports have evaluated outcomes using validated outcome instruments. LeBrun and colleagues evaluated 40 patients with isolated patellar fractures treated with ORIF or partial patellectomy. On the Knee Injury and Osteoarthritis Outcome Score, all showed significant disability, with longitudinal anterior banding with cerclage scoring the highest in the small sample size. Lazaro and colleagues evaluated 30 patients with low-energy patellar fractures treated with ORIF. Using the Knee Outcome Survey–Activities of Daily Living Scale, they reported that significant deficit persists at 1 year. Bonnaig and colleagues retrospectively compared ORIF with partial patellectomy and found both methods resulted in similar functional scores and complication rates. However, higher-energy injuries were more likely to have received a partial patellectomy compared with ORIF in their system, complicating the data.
Because of the important role played by the patella in the extensor mechanism, patellectomy would seem to significantly decrease function. In fact, the literature supports this notion. Einola and colleagues reported outcomes of 28 patients an average 7.5 years following patellectomy. Only 6 patients reported good results (21%), with the most predominant complaint being weakness and pain on movement and exertion. Quadriceps atrophy was also a problem, with power being within 75% of the normal knee in only 7 cases (25%). Another study by Scott reported that out of 71 patients, only 4 (6%) were happy with their long-term outcome following patellectomy. Nearly everyone experienced aching in the joint, and 60% complained of weakness. All patients exhibited quadriceps wasting. Given the poor outcomes, patellectomy should be considered only in massive comminution in which repair is futile. There are no studies to provide guidance on how much patella should be saved to preserve function.
Complications and Management
The most common complications are related to fixation implants and postoperative pain. Often, an additional surgery is necessary to remove the symptomatic implant. Lazaro and colleagues reported 11 of 30 (37%) patients with patellar fracture requiring removal of symptomatic implants. Additionally, 24 (80%) of the patients reported anterior knee pain. Functionally, decreases in strength, power, and endurance of knee extension by about 40% persisted at 1 year. Lebrun and colleagues reported 14 of 27 patients (52%) requiring removal of symptomatic implants and 5 of 13 (38%) with retained implants reporting anterior knee pain.
Other complications of patellar fracture treatment include infection, fixation failure, delayed union and malunion, loss of motion, osteoarthritis, and tendon rupture. Infection can be treated by standard protocols depending on the soft tissue involvement. If severe osteomyelitis develops, a total patellectomy may be required. Tension band failure may occur with premature motion and requires revision if the fracture fragments are displaced by more than 3 mm or the articular surface has a step of more than 3 mm ( Fig. 5 ). With modern surgical techniques, nonunion is rare. However, if detected, a period of restricted motion will often unite the fracture. Loss of knee motion is uncommon because of the early motion therapy protocols; however, if flexion is restricted several months following fixation, aggressive physical therapy to restore motion is recommended. In severe cases, manipulation under anesthesia may be beneficial, exercising extra caution in patients with a patellectomy. Arthroscopy to lyse intra-articular adhesions is also a reasonable option. If no improvement is noted after 12 months, a quadricepsplasty may be necessary. Osteoarthritis may develop and can be associated with an incongruous joint surface. Rarely, the extensor mechanism may rupture following total patellectomy, usually occurring at the proximal edge of the patellar tendon.








