Surgical Hip Dislocation for the Treatment of Femoroacetabular Impingement and Slipped Capital Femoral Epiphysis
Young-Jo Kim
Rachel Yvonne Goldstein
Surgical hip dislocation is an approach that can be utilized in the treatment of a wide variety of hip pathologies in order to improve or restore normal acetabular and/or femoral head-neck anatomy. Treatment of hip pathology through this approach seeks to preserve hip motion, prevent impingement, and delay or avoid early degenerative changes. This approach preserves the medial femoral circumflex artery (MFCA), the main blood supply to the femoral head, by maintaining intact external rotator muscles through the creation of a trochanteric flip osteotomy. Once performed, multiple procedures can safely be undertaken to address the specific pathology.
INDICATION/CONTRAINDICATIONS
Surgical dislocation is an approach to the hip that can safely be performed to treat a variety of intra- and extra-articular hip conditions.
Indications
Femoroacetabular impingement (FAI)
Extra-articular impingement
Labral tears
Chondral injuries
Femoral head-neck deformities
Fractures of the acetabulum, femoral head, or femoral neck
Tumors
Slipped capital femoral epiphysis (SCFE)
Post-Perthes deformities
Contraindications
Instability (may require a concomitant acetabular-sided procedure)
PREOPERATIVE PLANNING
Thorough history and physical examination is essential to identify the main source of symptoms.
Decreased femoral head-neck offset is best appreciated on:
The 45-degree Dunn lateral view of the hip
Radial reformats of CT or MR scans around the femoral neck axis
Three-dimensional reconstructions of a CT scan
Evaluation of a patient with SCFE requires AP and frog lateral views of the pelvis to evaluate slip severity.
After general anesthesia is administered, true hip flexion and hip rotation in both flexion and extension should be evaluated.
SURGICAL PROCEDURE
Patient positioning
The patient is placed in the full lateral position with the operative hip up (Fig. 20-1).
Secure the patient with a pegboard or lateral hip positioner. Care must be taken to ensure that positioners do not impede hip adduction, external rotation, or flexion.
A flat-top cushion with a half-moon-shaped cutout for the down leg is placed beneath the operative leg to stabilize the leg during the approach.
A hip drape with a sterile side bag is used to capture the leg during the dislocation maneuver. Alternatively, a sterile Mayo stand cover secured to the drapes may be utilized.
Approach
An anterior dislocation through a Kocher-Langenbeck or a Gibson approach with a trochanteric flip osteotomy
The Gibson approach
Proceeds between the gluteus medius and maximus muscles
Spares the abductors and gluteus maximus
Results in less hip extensor dysfunction
May make anterior exposure more difficult in patients who are obese or who have a very anterior border of the gluteus maximus
Kocher-Langenbeck approach
Splits the gluteus maximus muscle
Improves anterior exposure
Incision
A curved, longitudinal skin incision is made, centered over the junction between the anterior and middle thirds of the greater trochanter.
Subcutaneous tissue and fat are incised down to the iliotibial band and fascia overlying gluteus maximus.
Identify anterior border of gluteus maximus, which is marked by perforating branches of superior gluteal artery that run within the thin fascia between the gluteus medius and maximus muscles and perforate the fascia lata overlying the maximus and medius.
Because the vessels are accompanied by branches of the inferior gluteal nerve for the anterior portion of the gluteus maximus, the fascia is kept with the gluteus maximus.
The fascia lata is split distally in line with the incision.
The anterior border of the gluteus maximus is palpated, and the fascial incision is carried proximally along this line, taking care to bring gluteus maximus posterior off of fascia.
The space between the maximus and medius is opened, and the posterior border of the medius is identified.
The bursa at the posterior border of the greater trochanter is identified and reflected anteriorly.
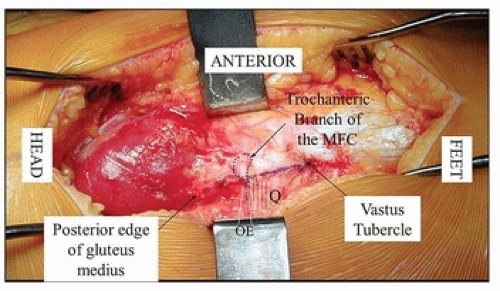
The trochanteric branch of the MFCA is visualized and coagulated (Fig. 20-2).
The hip is internally rotated 20 to 30 degrees, and the posterior border of the medius is identified. The border between the medius and the piriformis tendon is identified.
The proximal 4 to 5 cm of fascia of the vastus lateralis is incised, and the vastus muscle fibers are reflected anteriorly. Care is taken to stay superficial to the periosteum of the femur as the periosteum is contiguous with the hip capsule.
Trochanteric flip osteotomy
The osteotomy starts at posterosuperior edge of greater trochanter, about 5 mm anterior to the most posterior insertion of the medius on the greater trochanter, and runs distally toward the posterior border of the vastus lateralis muscle on the vastus ridge.
A 1- to 1.5-cm-thick osteotomy is made with an oscillating saw blade, leaving the piriformis tendon and short external rotators intact on the stable base of the greater trochanter (Fig. 20-3).
The osteotomy should stop at the anterior cortex and osteotome used to create a controlled fracture. This creates an anterior ridge to improve stability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree