Surgical Decompression of the Forearm, Hand, and Digits for Compartment Syndrome
Marci D. Jones
Rodrigo Santamarina
Lance G. Warhold
DEFINITION
Acute compartment syndrome is a condition in which increased tissue pressure compromises the circulation within the enclosed space of fascial compartments. As a result of this elevated interstitial pressure, the blood supply to the soft tissues is impaired. If left untreated, elevated pressures can cause irreversible muscle and nerve damage resulting in fibrosis and contracture.
ANATOMY
Compartment syndrome is most common in the forearm and hand but can occur in the arm and in the finger.
The arm is divided into two fascial compartments, the forearm into three compartments, the hand into ten compartments, and the finger into two compartments.
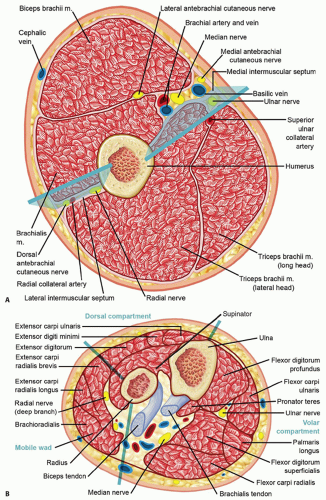
The two arm compartments are the anterior and posterior, separated by the medial and lateral intermuscular septa (FIG 1A).
The anterior arm compartment contains the biceps brachii, brachialis, and coracobrachialis.
The posterior arm compartment contains the triceps brachii.
The forearm consists of three compartments: the volar, the dorsal, and the mobile wad of three (FIG 1B).
The contents of the volar compartment include the flexor muscles and can be subdivided into superficial and deep components. The superficial muscles are the flexor carpi ulnaris, palmaris longus, pronator teres, and flexor carpi radialis. The deep muscles are the flexor digitorum superficialis and profundus, the flexor pollicis longus, and distally the pronator quadratus.
The dorsal compartment of the forearm contains the extensor muscles. The superficial extensors include the extensor digitorum communis, extensor digiti minimi, and extensor carpi ulnaris. The deep layer includes the supinator, abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, and extensor indicis.
The mobile wad of three is a distinct muscle compartment that contains the brachioradialis, extensor carpi radialis longus, and extensor carpi radialis brevis.
The wrist has one significant closed space, the carpal tunnel. Although not a compartment in the strictest sense, increased pressure in this tunnel can be detrimental to the median nerve.
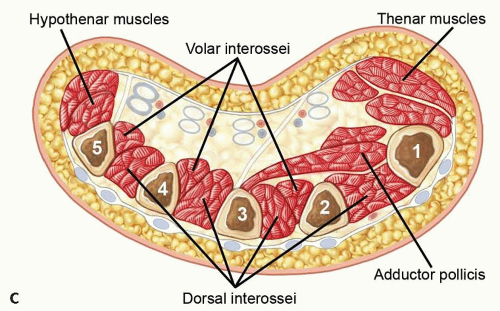
The hand contains ten distinct compartments (FIG 1C).
There are seven compartments for the interossei. Each of the four dorsal and three palmar interossei has a separate compartment.
The adductor compartment contains the adductor pollicis.
The thenar compartment contains the abductor pollicis brevis, the opponens pollicis, and the flexor pollicis brevis.
The hypothenar compartment contains the abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi.
Compartment syndrome can also occur in the finger due to the limited skin compliance from the multiple fascial attachments.
PATHOGENESIS
The blood flow to a compartment is determined by several factors, including venous pressure, arterial pressure, and local interstitial pressure. Increased pressure within a compartment decreases the blood supply to the soft tissues and can result in tissue ischemia and ultimately necrosis. Increased capillary permeability results from muscle ischemia. This increased permeability leads to intramuscular edema, increases the tissue pressure, decreases blood flow and oxygen transport, and leads to more tissue damage. It is easy to appreciate the vicious cycle that escalates the pathophysiology of the compartment syndrome.
Many conditions are associated with compartment syndrome. These can be divided into two major categories3:
Conditions that decrease compartment volume: tight casts or dressings, burn eschar, limb lengthening or application of traction, and increased external pressure on limb from prolonged weight (lying on limb or entrapment under a weight)
Conditions that increase compartment contents: bleeding (arterial or venous injury, anticoagulation, trauma), reperfusion injury, edema, infiltrated infusion, snakebite, infection, high-pressure injection
NATURAL HISTORY
Compartment syndrome results in hypoxic cell damage and ultimately anoxic cell death. Functional changes occur in muscle after 2 to 4 hours of total ischemia. Hypoxia to nerves causes paresthesia and hypoesthesia within 30 minutes of ischemia, but irreversible nerve damage may not occur until 12 hours or more of total ischemia.
An untreated compartment syndrome can result in permanent neural deficit, tissue necrosis, growth arrest, Volkmann contracture, and even wet gangrene.
PATIENT HISTORY AND PHYSICAL FINDINGS
It is important to elicit a detailed history and evaluate the possible causes of compartment syndrome (discussed earlier).
Pain out of proportion to physical findings is the most important finding. For patients with this finding, one must have a high clinical suspicion regardless of the presumed severity of the inciting event.
Most commonly, patients will present with a history of trauma or a crushing injury; however, other causes must not be overlooked.
Compartment syndrome may involve single or multiple compartments in the extremity.
Physical examination findings include the following:
A tense, swollen, and tender compartment (FIG 2)
Pain with passive stretch of the muscles within the compartment
Paresthesias or sensory disturbances in the nerve distribution of the compressed nerve are intermediate findings. This can be accompanied by motor weakness. Motor paralysis is a later finding.
Pallor and pulselessness are late findings.
The findings of pain out of proportion to physical examination, a tense compartment, and pain with passive stretch are sufficient to warrant intracompartmental pressure measurements. One should not delay definitive diagnosis and treatment until later findings are present.
In obtunded or sedated patients, a tense, swollen compartment is sufficient to warrant intracompartmental pressure measurements.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Clinical examination is the cornerstone of the diagnosis, and it is important to have a high degree of suspicion for compartment syndrome.
Immediate fasciotomy is indicated in patients with unequivocal symptoms and signs of compartment syndrome. Direct measurement of compartment pressures is indicated in all cases when the patient’s symptoms and physical examination signs are indicative of compartment syndrome, and it is especially important in patients who are obtunded or sedated.
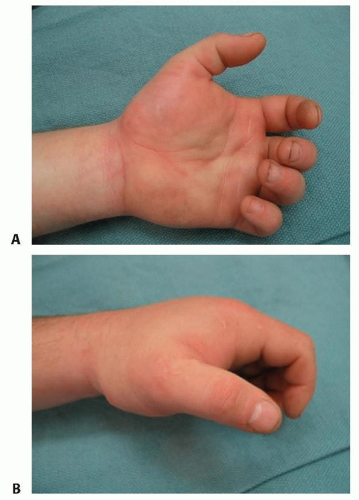
FIG 2 • Diffuse, tense swelling of the hand. A. Palmar view with loss of palmar concavity. B. Radial view.
Diagnosis of compartment syndrome of the finger is made clinically and not through the use of pressure measurement.
Pressure measurement in the arm is made in both anterior and posterior compartments. Anteriorly, the pressure is measured over the biceps muscle and posteriorly over the triceps muscle.
The physician must be careful not to injure the radial nerve when measuring the arm compartment pressure. The nerve courses deep to the triceps in the spiral groove of the humerus. Ten centimeters proximal to the lateral epicondyle, it passes through the lateral intermuscular septum to the anterior compartment.
In the forearm, the pressure is measured over the volar, mobile wad, and dorsal compartments.
The median and ulnar nerves are at risk during measurement of the volar compartment. The ulnar nerve courses deep to the flexor carpi ulnaris in the ulnar forearm; the median nerve is between the flexor digitorum superficialis and profundus muscles.
When measuring the mobile wad, the superficial branch of the radial nerve is deep to the brachioradialis in the forearm but emerges between the brachioradialis and extensor carpi radialis longus tendons about 8 cm proximal to the radial styloid.
The posterior interosseous nerve courses around the radial neck in the proximal radial forearm and should be avoided when measuring the mobile wad and dorsal compartments.
In the hand, pressure measurements should be made in the affected compartments; measurements are generally made in the area of the planned incisions.
There is not an absolute increased compartment pressure that warrants fasciotomy. When the pressure approaches 30 to 45 mm Hg, or 30 mm Hg less than the diastolic pressure, with concordant physical examination findings, decompressive fasciotomy should be performed.4 In the hand, lower pressures (15 to 20 mm Hg) may indicate compartment syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree