Functional activities of the upper extremity are limited in most individuals with a diagnosis of cerebral palsy (CP). However, surgical interventions are applied in less than 20% of pediatric patients with an upper extremity affected by CP. This article covers the surgical interventions used for the reconstruction of the upper limb in patients with CP. The optimal surgical approach for each deformity type is described. In addition, the various evaluation techniques of the upper extremity, the general principles of an operative treatment plan, and the appropriate postoperative care of these patients is presented.
Functional activities of the upper extremity are limited in most individuals with a diagnosis of cerebral palsy (CP). However, surgical interventions are applied in fewer than 20% of pediatric patients with an upper extremity affected by CP, in marked contrast to the lower extremity in which surgery is more frequently indicated. Apart from improving function, surgical procedures may decrease pain, prevent or fix upper limb deformity, and have a positive impact on the patient’s caregiving, self-esteem, and appearance. Several conservative treatment methods are also available (eg, therapy, casting, electrical stimulation, oral spasmolytic medications, and parenteral neuromuscular blocking agents). These methods are primarily used to preserve joint range of motion (ROM), to delay tendon and muscle contractures, and to prevent upper extremity osseous deformities. In patients without competently functional antagonist muscles, passive stretch for a minimum of 6 out of 24 hours is required to maintain muscle length and to avoid development of a fixed contracture. Occupational therapy and splinting alone do not accomplish long-term reduction of the involuntary spasm. Moreover, pharmacologic agents designed to decrease spasticity have not been validated as a definitive means of providing lasting improvement. In selected cases, surgery following conservative treatment has been reported to give satisfactory results.
This article covers the surgical interventions used for the reconstruction of the upper limb in patients with CP. The optimal surgical approach for each deformity type is described. In addition, the various evaluation techniques of the upper extremity, the general principles of an operative treatment plan, and the appropriate postoperative care of these patients is presented.
Evaluation
History and Physical Examination
A team approach to the management of the patient with CP is important; medical history and physical examination is the basis for the successful assessment of each individual. Input from the patient and his or her caregiver, and any involved health care worker should be provided. Functional classification systems (eg, House scale) as well as standardized testing regimens, such as the Melbourne Assessment of Unilateral Upper Limb Function (Melbourne), are helpful evaluation tools. The Melbourne scale allows objective measurement of the upper extremity function in patients with CP. Both active and passive ROM of the upper extremity joints should be assessed in a reliable and reproducible manner. In the authors’ institution, the Upper Extremity Rating Scale (UERS) is used for this purpose. The UERS provides a composite score of the active and passive ROM of the shoulder, elbow, forearm, and wrist. Degree of spasticity, and absence or presence and magnitude of involuntary movement disorders should also be evaluated and recorded. For patients with mild to moderate involvement, the use of the Melbourne scale and the Jebsen-Taylor Hand Function Test is suggested. A global instrument such as the WeeFIM (Uniform Data System for Medical Rehabilitation, University at Buffalo Foundation Activities, Inc, New York) is also available to measure self-care and functional skills. If possible, the patient is observed during ambulation, standing, and sitting to evaluate certain posturing and motion patterns. Several factors including fatigue level, anxiety, and even time of the day may affect the clinical findings; therefore, serial evaluations are necessary. Preoperatively, sensibility testing including evaluation of proprioception, stereognosis, and 2-point discrimination should also be performed.
Imaging Studies and Ancillary Testing
Evaluation of patients with CP is complex. Several examinations are necessary as part of the surgical planning process. Plain radiographs, computed tomography scans, and magnetic resonance imaging studies are helpful in assessing preoperative joint congruity. An individualized and detailed functional evaluation is also a critical component for developing the appropriate surgical plan. Dynamic electromyography (EMG) provides a qualitative and quantitative assessment of voluntary motor control and the type of motor activity of muscles being considered for transfer. A videotaped evaluation of the upper extremity in children with CP provides an objective assessment of a patient’s motor performance and functional capacity. Carlson and colleagues reported changes to the initial preoperative plan following the study of videotaped evaluations, especially for procedures addressing the wrist, digit, and thumb. Motor blockade produced by injections of botulinum toxin A (BTX-A) or a topical anesthetic agent (eg, bupivacaine) into the muscles identified for surgery may serve as a diagnostic tool to select the proper operative interventions.
General Principles of an Operative Treatment Plan
Diagnostic evaluation is helpful in identifying the suitable candidates for complex reconstructive procedures of the upper extremity. Selection of the appropriate intervention is required to achieve both specific and global outcomes individualized for each patient. However, it must be recognized that although some improvement in function and appearance may be a realistic goal for properly selected patients, normality can rarely, if ever, be achieved. The type of joint deformity, the underlying neuromuscular disorder, the preoperative sensibility and functional capacity of the limb, the patient’s intellectual status and goals, and the surgeon’s preferences are the factors used to devise a treatment plan.
Global surgical goals for best outcomes include (1) improved function, (2) facilitation of care, (3) pain reduction, and (4) enhancement of self-esteem. Specific surgical interventions may be performed at one or more levels (ie, shoulder, elbow, wrist, hand) to release overactive muscle groups, stabilize joints, and augment selective motor control of weak muscles by tendon transfer to achieve each patient’s specific goals. Surgical interventions may be reduced to a checklist of options ( Table 1 ). Proactive planning with multiple team members, including the development of an immediate postoperative regimen (eg, period and type of immobilization) and rehabilitation program, is the key to the success of the operative procedure.
| Joint | Aim | Options |
|---|---|---|
| Shoulder | Joint stabilization | Fusion, capsular reconstructions |
| Improve external rotation | Lengthen pectoralis major/subscapularis; transfer LD and/or teres major; humeral osteotomy | |
| Improve internal rotation | Lengthen/release infraspinatus/teres minor | |
| Elbow | Joint stabilization | Fusion |
| Improve extension | Lengthen biceps brachii/brachialis; BR release; flexor-pronator mass release (slide); capsulotomy | |
| Forearm | Improve supination | Reroute, lengthen, or release PT; radius/ulna osteotomy; flexor-pronator release (slide) |
| Wrist | Stabilization | Fusion |
| Improve extension | Flexor tendon release; proximal row carpectomy; ECU transfer; FCU transfer to ECRB/ECRL/EDC | |
| Thumb | Stabilization | Volar plate arthroplasty; MCP fusion |
| Improve extension | Release/lengthen FPL; reinforce EPL | |
| Improve abduction | Release adductor pollicis; reinforce APL; EPL rerouting | |
| Fingers | Flexion deformity | FDS to EDC transferflexor/pronator release (slide); FDS/FDP lengthening;FDS to FDP transfer |
| Swan-neck deformity | PIP joint tenodesis; central slip tenotomy; intrinsic origin release |
Operative Procedures
Shoulder
Adduction and internal rotation shoulder deformity is common in patients with CP; the deformity is due to unbalanced spasticity of the internal rotators of the arm at the glenohumeral joint (pectoralis major, latissimus dorsi, subscapularis, and teres major). A fixed contracture of the muscles (mentioned earlier) and the joint capsule may contribute to the deformity posture. Surgical interventions may need to address (1) the muscle/tendon and/or capsule contractures, and (2) the subluxation or dislocation of the humeral head in one or more planes of the shoulder joint. Inferior subluxation is the most common form in the hemiplegic shoulder. Moreover, dysplasia of the glenoid or humeral head and/or arthritis of the glenohumeral joint should be encountered in the treatment plan. In dynamic deformities, the glenohumeral articulation is typically stable with congruous articular surface contact. Treatment options include muscle lengthening, tendon transfer, humeral osteotomy, and shoulder joint fusion.
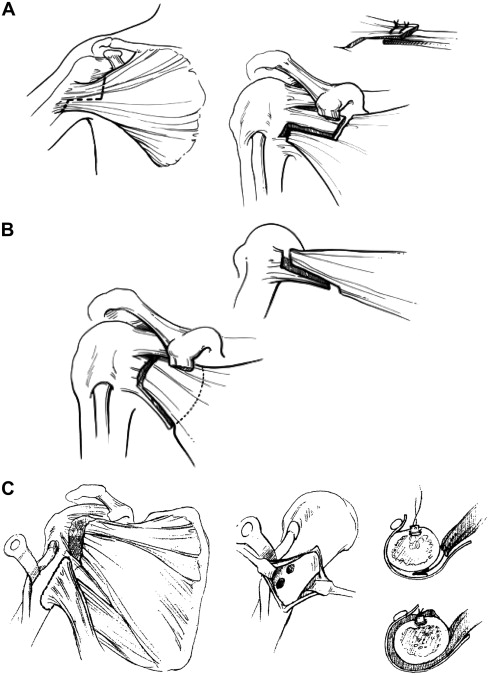
Although surgical treatment is rare, the pectoralis major and subscapularis muscles should be lengthened to correct shoulder adduction and internal rotation deformity; capsular release may also be performed. Transfer of the latissimus dorsi and teres major may augment active external rotation of the arm ( Fig. 1 ). In severe cases, release of the latissimus dorsi and teres major muscles in conjunction with the procedures described above may be required. If tendon/muscle release and/or transfer fail, a proximal or distal osteotomy of the humerus may be used to improve rotation of the arm. Osteotomy is also indicated for patients with dysplastic/subluxed or arthritic shoulder joints. Refractory arthritic pain may be addressed by shoulder fusion in individuals with CP; however, there is no experience with this procedure in the authors’ institution.
Elbow
Flexion contracture of the elbow may interfere with the use of the limb by limiting reach activities of the hand. The associated abnormal attitude of the extremity, appearing during gait, is also a cosmetic disability and may impair self-image unless addressed. Increased muscle tone of the biceps brachii, brachialis, and brachioradialis muscles results in dynamic motor imbalance around the elbow joint. Secondary fixed contractures of the capsule and the adjacent flexor-pronator muscle/tendon units may contribute to elbow flexion deformity. Subluxation/dislocation of the radial head due to associated hyperpronation of the forearm, accompanied with secondary dysplasia of the head may be an additional feature of elbow flexion deformity in children with CP. Pletcher and colleagues identified a radial head dislocation in approximately one-fourth of the children, with a combination of a flexion deformity of the elbow and a pronation contracture of the forearm. Most dislocations were posterior. The investigators proposed that preoperative elbow radiographs are required for all children with this combined deformity type.
Anterior elbow release is indicated for spastic elbow flexion deformity in patients with a diagnosis of CP. Operative treatment is seldom indicated unless extension loss exceeds 30°. For elbow deformities between 30° and 60°, soft tissue procedures (including excision of the lacertus fibrosus, Z-lengthening of the biceps, and fractional lengthening of the brachialis aponeurosis) are usually sufficient, and reliably decrease the degree of deformity ( Fig. 2 ). For deformities exceeding 60°, a flexor-pronator origin slide accompanied with anterior elbow capsulotomy may also be required.
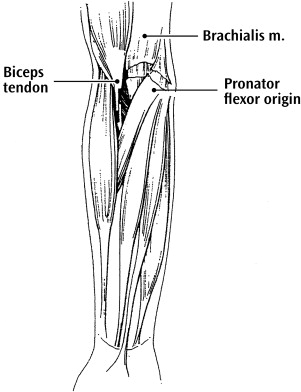
Anterior elbow release can improve active extension of the elbow, as well as both the functional use and aesthetic appearance of the involved upper extremity. Mital reported the only large series of patients in whom elbow flexion deformity was addressed by weakening of both the brachialis (fractional lengthening) and the biceps muscles (release of lacertus aponeurosis, tendon Z-lengthening). Following this procedure the flexion posture angle was decreased, and the patient’s ability to flex the elbow or supinate the forearm was retained. However, the risk of increasing pronation deformity following a biceps-lengthening procedure should be noted; rerouting or lengthening of the pronator teres (PT) muscle may prevent increased pronation deformity after anterior elbow release.
Elbow fusion is considered as the last option for operative treatment of the elbow flexion deformity. It is reserved for patients who experience intractable elbow pain. However, this procedure is seldom used and has never been performed at the authors’ institution.
Forearm
Pronation of the forearm is part of the typical pattern of the upper limb in patients with CP. The deformity may be fixed, dynamic, or a combination of both; hypertonicity of the PT and pronator quadratus muscles is the primary cause. Inability to supinate the forearm in the absence of shoulder compensation interferes with hand function and compromises activities such as turning a doorknob or using a key. Multiple nonsurgical measures (muscle stretching, plaster casts, splints, braces, and BTX-A) have been advocated. Following extensive conservative treatment, operative procedures in properly selected patients are appropriate to improve forearm position and function. Allowing active supination to neutral should be considered a successful outcome.
Operations can be classified into 2 groups. In group I, procedures primarily designed to improve functions such as wrist dorsiflexion, elbow motion, and hand grasp and release are included. The release of the pronation contracture is incidental to these procedures. The flexor-pronator release, primarily advocated to decrease flexion deformity of the wrist and fingers, has been reported to improve supination of the forearm. However, the risk of supination deformity following excessive flexor-pronator release is increased. Green described a method to correct dynamic flexion deformity of the wrist; the flexor carpi ulnaris (FCU) tendon is transferred to augment either the extensor carpi radialis brevis (ECRB) or the extensor carpi radialis longus (ECRL) muscles. By transferring the FCU tendon from ulnar to radial, a supination moment is created and pronation deformity is potentially decreased.
In group II, procedures are designed exclusively for pronation deformity of the forearm. PT release tenotomy, fractional lengthening, Z-lengthening, and rerouting are described. In addition, rerouting of the brachioradialis has been reported to improve supination. In none of the techniques mentioned here is the pronator quadratus released at the same time; thus, the risk of loss of active pronation is minimized. Dynamic EMG as well as clinical examination of the forearm helps decide the treatment plan. In the presence of passive supination, PT release, Z-lengthening, or fractional lengthening is appropriate for patients with a continuously firing PT by EMG. However, for patients with a phase-dependent PT muscle activity, PT rerouting is the preferred surgical option at the authors’ institution ( Fig. 3 ). If soft tissue procedures fail, radial osteotomy may be performed to improve forearm position. In severe cases, inferior radioulnar joint fusion may also be an option.










