Fig. 6.1
Anteroposterior (a) and lateral (b) radiograph of the elbow showing slightly decrease of the joint line width, subchondral cysts, and mild widening of the trochlear notch (corresponding to a grade III in the Arnold-Hilgartner classification)

Fig. 6.2
Anteroposterior (a) and lateral (b) radiograph of the patient in Fig. 6.1 5 years later. The articular surface is narrowed and the widening of the trochlear notch is increased. The radiocapitellar joint is the first part of the joint to show signs of the disease
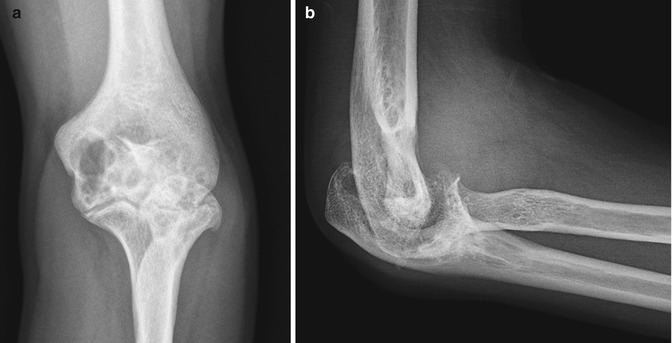
Fig. 6.3
Anteroposterior (a) and lateral (b) elbow radiographs with marked hypertrophy of the radial head that limited forearm pronation. Additionally, some signs of advanced hemophilic arthropathy can be seen
Magnetic resonance imaging (MRI) and ultrasound may show marked signs of synovial hypertrophy in radiologic stages I and II. High-quality MRI may show the different degrees of cartilage erosion in stages II and III and can be decisive to make a correct indication for surgery. Specifically, MRI is the most useful technique to detect persistent synovitis and joint effusion and is particularly useful to detect early degrees of arthropathy [4]. MRI has increased costs and a combined method of radiographic and ultrasound follow-up may be a feasible alternative.
6.5 Management
6.5.1 Conservative Management
Conservative management predates any form of surgical management of elbow hemophilia. Primary pharmacologic prophylaxis is the treatment of choice as it may reduce the chance of having the first hemorrhagic episode that can start the cascade of synovial hypertrophy with increasing risk of subsequent bleeding episodes. Delaying prophylactic treatment has shown in a definite deterioration in radiological scores for every year after the first joint bleeds [5]. The forms of prophylaxis may vary from weekly injections to full form treatment that may require a central venous access, and the choice has to be made depending on patient and attending to center factors, including cost issues.
When a bleeding episode ensues, all efforts are directed towards aggressive medical treatment of major hemorrhages and chronic hemophilic synovitis to prevent hemophilic arthropathy. Other conservative measures such as radiosynovectomy with different chemical agents have been very effective in the treatment of persistent synovitis. Physiotherapy is important in managing these patients to prevent flexion deformities and maximizing range of motion.
The range of surgical options in the hemophiliac elbow depends on the degree of symptoms and pathology. Persistent synovitis after adequate medical treatment is subject to synovectomy which can be performed open or arthroscopically. Many patients with chronic synovitis may have radiocapitellar degeneration and an associated radial head removal can be performed. Only patients with persistent pain and loss of function and severe destruction of the joint are candidates for total elbow replacement.
6.5.2 Synovectomy
It is yet unclear if there is a direct relationship between synovitis and cartilage degeneration or if the cartilage is in fact directly affected by the contact with blood, but synovectomy may be indicated with persistent symptoms of synovitis with no response to conservative measures. It seems that synovectomy is an appropriate treatment to delay joint degeneration, more so if performed early [6].
While the incidence of bleeding is significantly decreased after surgical synovectomy, it is not necessarily associated with a cessation of the progression of joint pathology. Reduced incidence of bleeds following postsurgical synovectomy may serve to delay reconstructive operations until a later period in life. Eventually, the disease proceeds to end-stage arthropathy and joint function correspondingly decreases with age. Patients should be managed conservatively with therapeutic doses of factor concentrate replacement for a reasonable period of time in an effort to avoid surgical treatment [7].
Indication for Synovectomy
The senior author (ECR-M) favors using radiosynovectomy in children older than 12 years of age, arthroscopic synovectomy in patients under that age, limiting open surgery for adults requiring radial head removal due to severe limitation and synovectomy in the same surgical session [8]. However, recent advancements in surgical technique and instrumentation have fostered the use of arthroscopic surgery as a valuable tool in the treatment of these patients [9].
Open Surgical Synovectomy
Patients are positioned supine with the arm resting on an arm rest. The limb is exsanguinated and a Kocher approach to the elbow is used. The interval between the anconeus and the extensor carpi ulnaris is identified by palpation or identification of a fat strip in the distal part of the interval. The dissection is carried out to the capsule and it is incised just anterior to the lateral collateral ligament. Working with the forearm in pronation increases the safe distance to the posterior interosseous nerve. If a radial head resection is to be performed, Hohmann retractors are placed around the radial neck and a subcapital osteotomy using an oscillating saw is performed. The axis of the neck cut should be perpendicular to the axial alignment of the radius and the height should be just distal to the lesser sigmoid notch. Synovectomy is easily performed with dedicated rongeurs through the space provided by the radial head resection including the anterior and posterior aspects of the joint. If access to the posterior part of the joint is limited, extension of the elbow and slight elevation of the triceps may improve the exposure.
If the radial head is not resected, access may be limited by the presence of the radial head. Extending the approach proximally may facilitate synovectomy of the hypertrophied synovial tissue. In these cases, it is probable that an arthroscopic technique increases our ability to remove all the diseased tissue.
Osteophytes limiting flexion and extension should be removed and waxed to prevent postoperative bleeding. Standard closure is performed with interrupted closure of the forearm fascia with a deep suction drain. A compressive dressing is applied with a posterior plaster splint in 90° elbow flexion and supination is applied.
Arthroscopic Synovectomy
We place patients in the lateral decubitus with the affected arm on a dedicated arm holder and under tourniquet control. We insufflate the joint with saline through the soft spot to facilitate introduction of the arthroscope. Our first portal is a proximal anteromedial portal. Patients should be assessed preoperatively as to the existence of ulnar nerve subluxation. If this is the case, we perform an anterior transposition of the nerve through an open approach and then proceed to the arthroscopic synovectomy.
Our second portal is an anterolateral portal performed with an outside-in technique and it should give access to remove all the disease synovium in the anterior compartment by exchanging viewing and working portals. Synovectomy is achieved with the use of a motorized shaver. Posterior synovectomy is used through a mid-triceps portal, an accessory lateral portal, and a soft spot portal. If there is bony impingement, bone resection with a burr can be achieved. The portals are closed with horizontal mattress sutures over a drain placed in the posterior compartment. Postoperative indications are similar to the open technique.
Results of Synovectomy
Le Balc’h et al. reported their results in 23 elbows in 18 patients in young patients (mean, 14 years of age) with a severe deficiency (>1 %) with a minimum follow-up of 18 months. The indication for surgery was recurrent episodes of bleeding despite substitutive treatment for each episode, mainly with lateral elbow pain. The age was related to the degree of pain. An increase in motion was observed in 23 elbows (pronosupination in 9 elbows and flexion-extension in 14 elbows). Four patients reported recurrent bleeding episodes and pain persisted in three. They reported the use of radial head removal in the oldest patients (the oldest being 25 years old) if radiocapitellar wear was present and considered the presence of inhibitor a contraindication to the procedure [10].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








