Fig. 4.1
Anteroposterior (a) and lateral (b) lateral radiograph has to be turned 90º to the right, on the same way as a watch (arrows)
One study assessing both intra- and interobserver variability of the two scoring systems demonstrated generally good correlation if there is minimal or maximal joint disease, but poor levels of agreement if there is mild or moderate HA [8]. The World Federation of Hemophilia recommends the Pettersson score for universal use [9].
Once radiographic changes are present, the clinical course of the arthropathy is usually progressive and irreversible. Improved therapy has led to the need for more sensitive tools for the assessment of the degree of joint damage, which can evaluate the subtle joint changes not seen on plain film. However, once the disease is advanced, it can usually be monitored with x-ray alone [5]. Soft tissue swelling can be suggested, but is often not clearly delineated (Fig. 4.2).
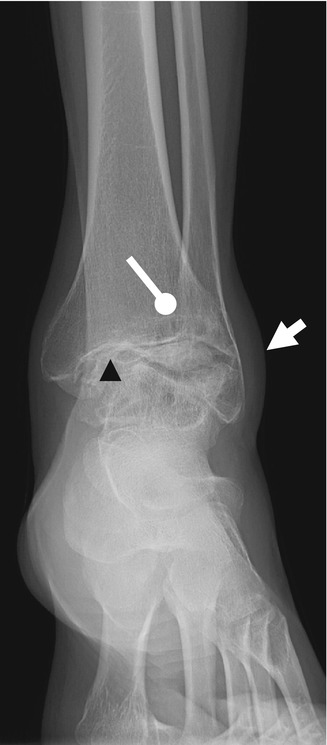
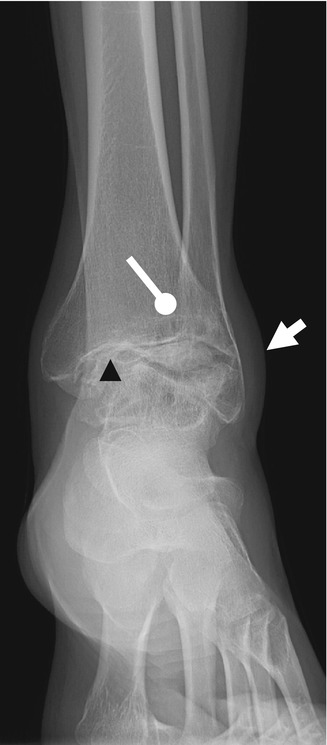
Fig. 4.2
X-ray anteroposterior (AP) view of the ankle demonstrating soft tissue swelling (arrow), osteoporosis, epiphyseal overgrowth, subchondral bone cyst (round arrow) with significantly narrowed joint space (arrowhead)
4.3 Ultrasonography
US is an imaging technique with a progressive and extensive use in the musculoskeletal system and can be a useful complementary technique in the evaluation of HA, which is readily available and does not require the child to be sedated. US has some other potential advantages, including lack of ionizing radiation, cost- and time-effectiveness, accessibility, and real-time and dynamic examinations. In this way, US can be used as a first diagnostic imaging procedure instead of MRI. The major disadvantage of US is its operator dependence, requiring a long learning curve and a limited value of images for orthopedic surgeons and physicians that prefer a more anatomical imaging modality, such as MRI [10].
Linear high-resolution (7–17 MHz) probes are typically used for assessing HA [11], enabling the visualization of superficial musculoskeletal structures such as synovium, tendons, musculature, and the cartilage/osteochondral interface at the edge of the joints on grayscale sonograms. US can also be used to follow the progression or regression of soft tissue hematomas and pseudotumors [2].
US can be used to assess joint effusions in acute episodes. US as a diagnostic technique in the initial stages of hemophilia permits the differentiation between effusion and synovial thickening (Fig. 4.3). A selective compression with the US probe may help to distinguish both entities; the fluid will be displaced out, while the synovium remains incompressible [10, 12]. A hemarthrosis may demonstrate a different echogenicity, depending on the stage of degradation of the blood products [11]. The normal synovium is a thin membrane. When it becomes inflamed, diffuse or nodular thickening of the membrane is seen, which may show increased vascular flow on Doppler US. Differentiation between hemarthrosis and synovial hypertrophy helps to determine when factor replacement is necessary for patients treated on demand [5]. The selective implementation of prophylaxis would require the availability of a more sensitive tool to monitor for the development of synovitis than is currently possible with clinical surveillance or x-ray. MRI is such a tool and is utilized for the evaluation of HA [13]. However, MRI is expensive and requires sedation in younger children, precluding its utility for monitoring synovitis [14].
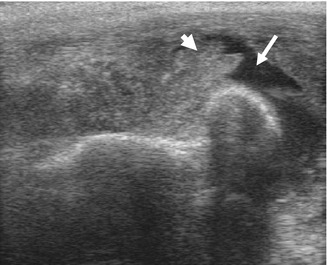
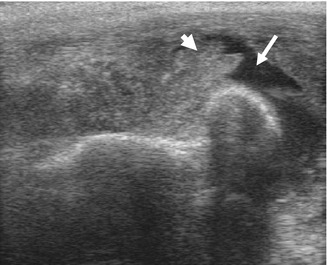
Fig. 4.3
Elbow. US longitudinal view of the radial head with joint effusions (arrow) and severe synovial thickening (arrowhead) demonstrated as a hypoechoic tissue
US with power Doppler has been used to detect and quantify vascularity in other arthritides [15] and has the capability of evaluating synovial vascularity in hemophilic joints. A recent study [16] showed a strong correlation between Doppler and dynamic contrast-enhanced MRI measurements in hemophilic knees, elbows, and ankles.
In fact, contrast-enhanced US may be comparable to MRI in estimating synovial vascularity for the diagnosis of active synovitis as seen with rheumatoid arthritis [17]. US also reveals early cartilaginous involvement and partial visualization of the joints [17] (Fig. 4.4).
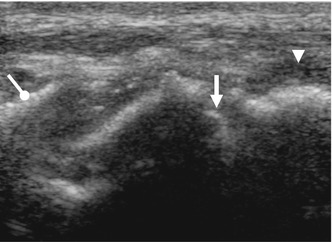
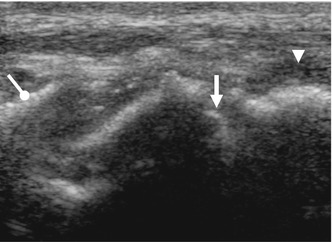
Fig. 4.4
Ankle. US longitudinal view over the anterior tibiotalar joint shows narrowing of the joint space, tibial bony spur (round arrow), mild synovial hyperplasia (arrowhead), and irregularity of the hyaline cartilage and subchondral plate of the talar dome (arrow)
Previous studies evaluated the US findings of HA [11, 18] and described a systematic protocol for data acquisition of US findings in hemophilic joints [12, 19]. Nevertheless, the value of this technique for the assessment of HA in comparison with MRI and physical examination has not been fully evaluated so far. As a result, this technique has been underemployed in clinical practice. Another challenge of US relates to the interpretation of images and comparison with other diagnostic tests.
4.4 Magnetic Resonance Imaging
MRI was introduced as a medical imaging modality in the 1980s, and it uses radio waves and magnetic fields [3].
MRI has been shown to more accurately assess a HA than radiography. MRI has obvious advantages, including the increased level of detail of soft tissue and cartilage changes and lack of ionizing radiation, but it is more costly, less accessible, and more time consuming and requires sedation in younger children [6, 14].
MRI provides information on all aspects of HA, demonstrating early arthropathic changes such as hemarthrosis, effusion, synovial hypertrophy, hemosiderin deposition, and small focal cartilage defects without joint space narrowing, which cannot be delineated by x-ray imaging. Moreover, MRI can provide information about more advanced changes, such as erosions, subchondral cysts, and cartilage destruction with joint space narrowing [5, 17] (Fig. 4.5).


Fig. 4.5
The T1-weighted MRI coronal view of an elbow shows erosions, subchondral cysts (arrowhead), and cartilage destruction with joint space narrowing (arrow)
There has been shown to be a high correlation between the presence of osseous changes on x-ray and the presence of synovial or cartilaginous changes on MRI, especially in the advanced stages of the disease. The sensitivity of MRI to detect the changes of early HA is high [20], but is lower for the elbow than for the knee or ankle [5].
Exact recommendations of the sequences to be performed in HA have not been established [6]. A T1-weighted sequence is always useful to demonstrate anatomy and osteochondral lesions. A short T1 inversion recovery (STIR) sequence is very sensitive for demonstrating bone edema (Fig. 4.6), and gradient-echo (GRE) sequences improve the visualization of the cartilage, synovium, and hemosiderin [17, 21]. T2* GRE sequence results in enhanced visibility of blood products in the acute stage (deoxyhemoglobin) and the chronic stage (hemosiderin) and can identify even the smallest amount of hemosiderin deposition in a joint [21] (Fig. 4.7). However, when there is a significant amount of hemosiderin in the joint, the degree of susceptibility artifact may be too great to enable interpretation.
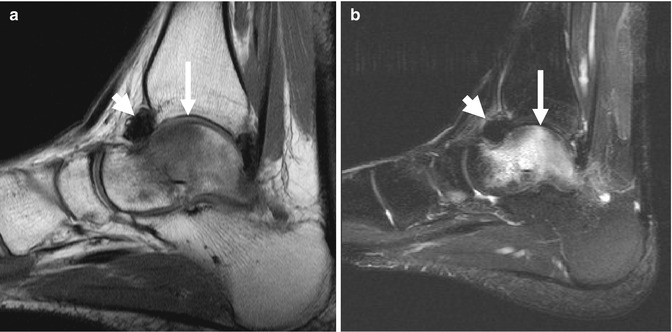
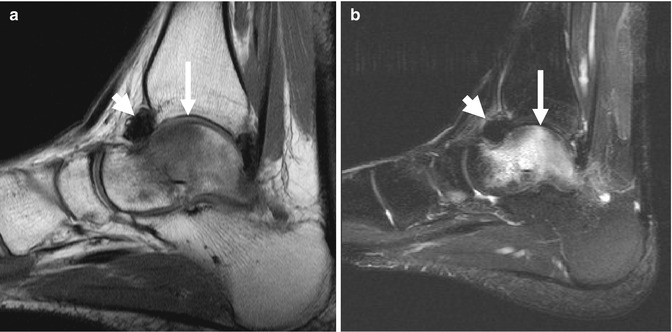
Fig. 4.6




Sagittal T1 (a) and STIR (b) images of the ankle, demonstrating bone edema of the talar dome (arrow) and synovial hypertrophy with iron deposit in the tibiotalar joint (arrowhead)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








