Supramalleolar Tibial Osteotomy
Beat Hintermann
Markus Knupp
Asymmetric loading of the ankle joint often results in degenerative disease with chronic pain, disability, and instability. The underlying cause is in many instances misalignment and/or malrotation deformity of the distal tibia, resulting from malunited fractures of the distal tibia and fibula. In these cases, the tibiotalar joint surfaces usually remain parallel. Additional ligamentous incompetence and muscular deficiency may destabilize the ankle joint, which typically result in tilting of the talus in frontal plane or anterior extrusion of talus out of ankle mortise.
The cause of ankle osteoarthritis is posttraumatic in over 80%, and typically younger patients are involved (1,2). Malunited fractures may cause asymmetric loading and thus asymmetric wear of tibiotalar joint over time. Early results with correcting osteotomy of the distal tibia have shown the benefit of rebalancing the ankle joint in terms of pain relief and improvement of function (3, 4, 5 and 6). This benefit is even more important, as mostly younger and active patients are concerned and long-term results after arthrodesis and total ankle replacement are not always predictable (7).
The question remains, however, which patient with advanced asymmetric ankle osteoarthritis may benefit from such correcting osteotomies and soft tissue balancing. Based upon surprisingly good results in a preliminary series of 35 patients with symptomatic unilateral osteoarthritis of the ankle joint (4), we attempt to correct the deformity to achieve a well-aligned and balanced tibiotalar joint. If necessary, total ankle replacement is considered in a second stage. Furthermore, most authors recommend not implanting a total ankle replacement if a deformity of more than 10° to 15° in any plane is present (7). Therefore, a supramalleolar osteotomy may also be indicated before a prosthesis is implanted or to correct malpositioned implants.
INDICATIONS AND CONTRAINDICATIONS
The aim of the osteotomy is to unload the affected area. Some attention should be paid, however, to severe hindfoot instability (“floppy hindfoot”) and severe vascular and neurologic deficiency in the affected extremity.
A contraindication for correcting osteotomy of distal tibia is seen in neuroarthropathic disorders such as Charcot ankle or arthritis in a patient with peripheral neuropathy. Another contraindication is altered bone quality due to medications, large cysts, osteopenia, rheumatologic disorders, and advanced age. Tobacco use is a relative contraindication. Local factors that may cause postoperative wound problems include ischemia due to peripheral vascular disease, scars, and infections around the foot.
PREOPERATIVE PLANNING
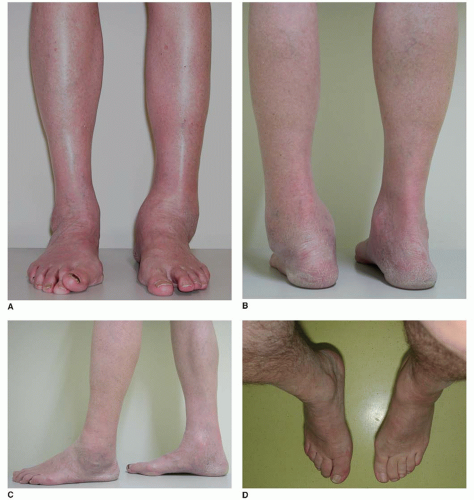
Careful assessment of the deformed ankle and the underlying causes is mandatory for success of the surgical procedure. The history obtained should elucidate any previous trauma, fractures during and after adolescence, and their consecutive treatment. The clinical investigation should include inspection of the feet for any swelling, prominence, and scar formation. The feet should be palpated for tenderness and bone formation. Feet should be examined in the standing position to recognize and quantify overall deformity/misalignment in coronal and sagittal planes (Fig. 34.1), to clarify whether the hindfoot deformity is correctable while moving to tiptoe position, and to
clarify whether there is a forefoot-related hindfoot problem while underlying a block beneath lateral forefoot (Coleman block test). The unloaded feet should be examined in the sitting position to assess the abduction/adduction position of the affected and nonaffected foot to exclude a malrotation deformity (Fig. 34.1D), to clarify whether the deformity is correctable, to assess the lateral stability of the ankle (varus tilt test), to assess the medial stability of the ankle (valgus tilt test), to assess the anterior stability of the ankle (drawer test), to determine eversion power of peroneus brevis muscle to exclude a tendon dysfunction, to determine inversion power of posterior tibial tendon to exclude a tendon dysfunction, to assess the remaining dorsiflexion-plantarflexion (motion at ankle joint), and to assess the remaining pronation/supination (motion at subtalar joint).
clarify whether there is a forefoot-related hindfoot problem while underlying a block beneath lateral forefoot (Coleman block test). The unloaded feet should be examined in the sitting position to assess the abduction/adduction position of the affected and nonaffected foot to exclude a malrotation deformity (Fig. 34.1D), to clarify whether the deformity is correctable, to assess the lateral stability of the ankle (varus tilt test), to assess the medial stability of the ankle (valgus tilt test), to assess the anterior stability of the ankle (drawer test), to determine eversion power of peroneus brevis muscle to exclude a tendon dysfunction, to determine inversion power of posterior tibial tendon to exclude a tendon dysfunction, to assess the remaining dorsiflexion-plantarflexion (motion at ankle joint), and to assess the remaining pronation/supination (motion at subtalar joint).
The radiologic assessment should include weight-bearing x-rays of both lower extremities including an anteroposterior (AP) view of the ankle including a major portion of tibia (Fig. 34.2A), a lateral view of the foot (Fig. 34.2B), an AP view of the foot (Fig. 34.2C), a Saltzman view of the hindfoot (Fig. 34.2D), and radiograph of both lower extremities. Additional imaging methods may be advised such as CT scan, hybrid imaging of single-photon emission computed tomography (SPECT), and MRI.
Plain radiographs are helpful to assess degeneration (8) and axial deviation, but cannot identify early degenerative changes. CT scans or MRI is sensitive to detect cysts, osteochondral defects, or concomitant lesions, such as alterations of the ligaments or the tendons, but give only limited information on cartilage pathology. Additionally, bilateral CT scans are used to detect and quantify malrotation at any level of the lower extremity. Recently, hybrid imaging of single-photon emission computed tomography (SPECT) and computed tomography were introduced, which allow for direct fusion of morphologic (CT) and functional (SPECT) data sets (9). With regard to pedal skeletal abnormalities, this approach appears to be extremely useful because it combines the advantages of both techniques (high-resolution imaging of bone morphology and high-sensitivity imagining of bone metabolism) (10).
Measurement of the deformity (11):
Center of rotation of angulation (CORA)—coronal plane, sagittal plane
Lateral distal tibial angle (LDTA)—coronal plane
Medial proximal tibial angle (MPTA)—coronal plane
Tibial and fibular malrotation—horizontal plane
Planning of correction:
Osteotomy of tibia at the level of deformity (CORA)—isolated angular correction
Osteotomy of tibia at a level different from that of the CORA—angular correction, translation of the distal fragment accordingly
Osteotomy of fibula at the level of tibial osteotomy
Frontal Plane Ankle Deformities
Varus deformity of the tibial plafond is usually tolerated less than valgus deformity because there is normally half the compensatory range of motion of subtalar eversion compared with inversion. Because the area of weight bearing between tibia and talus may actually be increased resulting in an increased load transfer from the medial facet of the talus to the very wide medial malleolus, varus deformity is less likely to lead to degenerative changes (12). This explains why the limitation in the ability of the foot to compensate for varus creates problems in the forefoot and subtalar joint but not in the ankle joint. In contrast, valgus deformity of tibial plafond may lead to degenerative changes of the ankle joint, as it further lateralizes the ground reaction forces and thereby increases the overload of lateral tibiotalar joint (13). Furthermore, valgus deformity places increased loads on the fibula and therefore on the distal tibiofibular joint. This joint can widen under load, resulting in decreasing contact area of tibia to talus (14). As a principle, the closer the CORA is to the ankle joint, the greater is the malrotation (greater LDTA) of the ankle joint (15). Whereas, the closer the CORA is to the knee, the greater is the effect on the knee joint (greater MPTA). Congenital deformities usually have a CORA at the level of the plafond, developmental deformities a CORA just proximal to the distal tibial physis, and postfracture deformities a CORA at various levels, depending on the level of the original fracture and the magnitude and direction of associated translation deformity.
Sagittal Plane Ankle Deformities
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree