Subtalar Arthroscopy: Perspective 2
Christopher E. Gross
Mark E. Easley
DEFINITION
Lateral or posterior subtalar arthroscopy confers diagnostic and potentially therapeutic value in treating subtalar trauma, arthrofibrosis, impingement, and cartilage pathology.
One must establish a definitive diagnosis of subtalar pathology based on physical examination and detailed imaging studies improve the likelihood of successful outcome with subtalar arthroscopy.
Exploratory, or diagnostic, subtalar arthroscopy is rarely indicated.
Based on preoperative physical examination and detailed imaging, determination may be made if lateral or posterior subtalar arthroscopy is favored to access subtalar pathology.
ANATOMY
The subtalar joint comprises the talus and three facets of the superior articular surface of the calcaneus: anterior, middle, and posterior facet.
Functionally, the subtalar joint is separated into an anterior (anterior and middle articular surfaces, often confluent) and posterior portion.
The posterior facet is the largest and bears the majority of the body weight.
The tarsal canal (contents: talar body blood supply, talocalcaneal interosseous, inferior extensor retinaculum, and cervical ligaments) separates the anterior and posterior portions of the subtalar joint. Its lateral opening is the sinus tarsi.
The anterior and middle facets are usually inaccessible unless the interosseous ligament is torn.
Subtalar motion is not pure inversion and eversion with inversion/eversion and measuring subtalar motion is rarely exact given the subtalar joint’s couple with the ankle.
PATHOGENESIS
Not much literature is dedicated to osteochondral lesions of the subtalar joint.
Snowboarders, with their hindfoot held in place with stiff boots during a fall, in addition to lateral talar process fractures, may experience injury to the middle facet of the subtalar joint.
The sustentaculum tali and middle facet are impacted.1
Sinus tarsi syndrome is clinically described as lateral pain over the sinus tarsi.
Although the etiology of sinus tarsi syndrome is unknown, several theories exist3:
Scarring and fibrosis of interosseous or cervical ligament
Subtalar synovitis
Sinus fat pad alterations and scarring
PATIENT HISTORY AND PHYSICAL FINDINGS
Commensurate with the patient’s complaint of hindfoot soreness, stiffness, and, occasionally, a sense of instability, particularly while walking on uneven surfaces, physical examination of the hindfoot demonstrates pain and limited motion.
By stabilizing the ankle, typically with thumb support on the medial talar neck, some sense of subtalar inversion/eversion compared to the contralateral hindfoot should identify pain and restriction of motion.
The patient often describes diffuse hindfoot pain, medially, laterally, and posteriorly.
Sinus tarsi tenderness is a consistent finding suggestive of anterior subtalar pathology, often due to interosseous ligament sprain or lateral process avulsion injury.
Pain with forced eversion may suggest lateral subtalar gutter impingement and is generally the most sensitive area on examination of a patient with subtalar pathology.
Pain with forced plantarflexion is not definitive for the ankle or subtalar joint but may be due to posterior subtalar impingement.
Due to the coupled ankle and subtalar mechanism, subtalar and ankle instability are often difficult to distinguish from ankle instability. Moreover, reliable and reproducible stress maneuvers that isolate subtalar motion have not been developed.
Although invasive, perhaps the best test to isolate subtalar pathology is local anesthetic subtalar injection via the sinus tarsi.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs
May not reveal diagnosis
Anteroposterior (AP), lateral, and oblique weight-bearing views of the foot
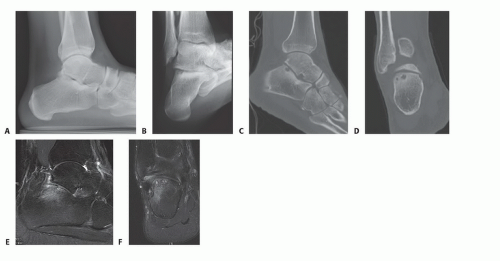
Broden view: posterior facet (FIG 1B)
The foot is placed in neutral flexion, and the leg is internally rotated 30 to 40 degrees. The x-ray beam is centered over the lateral malleolus, and four x-rays are made with the tube angled 40-, 30-, 20-, and 10-degree cephalic tilt. The 10-degree view shows the posterior portion of the posterior facet and the 40-degree view shows the anterior portion.
Lateral oblique: posterior facet
Foot is dorsiflexed, everted, and externally rotated to 60 degrees.
Beam is centered 2 cm below medial malleolus with 10-degree cephalic tilt.
Computed tomography
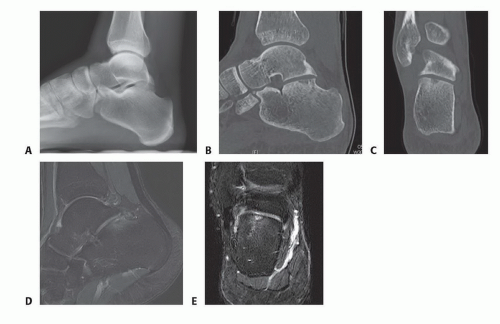
Cystic component of osteochondral lesions of the subtalar joint (FIGS 1C,D and 2C,D)
Subchondral sclerosis, cystic changes consistent with arthritis
Magnetic resonance imaging
Cartilage or osteochondral defects (FIGS 1E,F and 2E,F)
Edema associated with osteochondral lesions
Sinus tarsi pad fat changes
Interosseous or cervical ligament tears
Stress reactions
Fibrosis within subtalar joint
Cartilaginous coalitions
DIFFERENTIAL DIAGNOSIS
Lateral ankle instability
Peroneal tendon pathology
Fractures of:
Lateral talar process
Anterior beak of the calcaneus
Stieda process
Navicular
Calcaneus
Osteochondral lesions of the inferior surface of talus or posterior facet of calcaneus
Edema associated with osteochondral lesions
Subtalar arthritis
Stress reactions
Fibrosis within subtalar joint
Cartilage coalitions
NONOPERATIVE MANAGEMENT
Functional rehabilitation includes range of motion for the ankle and hindfoot, concentric and eccentric muscle strengthening, endurance training with particular attention to the peroneal musculature, and proprioceptive exercises.
Anesthetic (with or without corticosteroid) injection into the sinus tarsi
UCBL orthosis to limit inversion/eversion
Nonsteroidal anti-inflammatory agent
SURGICAL MANAGEMENT
Indications
Sinus tarsi syndrome with identifiable pathology
Chondral and osteochondral lesions
Chronic synovitis
Adhesions, arthrofibrosis
Loose bodies
Mild arthritis
Impingement (os trigonum)
Contraindications
Local soft tissue/bone infection
Severe arthritis/deformity
Poor vascular status
Edema
Chronic regional pain syndrome
Preoperative Planning
Imaging studies must be reviewed so that the location of the lesion is identified.
Plain films must be reviewed for degenerative changes, malalignment, and fractures.
Physical examination, combined with preoperative imaging, typically directs if lateral or posterior subtalar arthroscopy is favored to access the specific subtalar pathology.
In general, lateral subtalar arthroscopy is favored for sinus tarsi and anterior pathology, including the anterior one-half of the subtalar joint.
Posterior arthroscopy is favored for posterior hindfoot impingement and pathology isolated to the posterior half of the subtalar joint.
Lateral subtalar and lateral gutter pathology may be better accessed with the lateral subtalar arthroscopy.
Medial subtalar pathology is difficult to access from either lateral or posterior portals.
TECHNIQUES
▪ Lateral Arthroscopy for Anterior and Lateral Subtalar Pathology
Background
A 25-year-old man with a 6-month history of hindfoot pain after inversion ankle/hindfoot injury, failing nonoperative measures.
Physical examination and imaging studies (see FIG 1) suggested lateral gutter impingement, sinus tarsi pathology, and lateral osteochondral lesion of the posterior calcaneal facet.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree