Subtalar Arthroscopy: Perspective 1
Carol Frey
DEFINITION
The subtalar joint is a complex and functionally important joint of the lower extremity. It plays a major role in inversion and eversion of the foot.
Subtalar arthroscopy can be applied as a diagnostic and therapeutic instrument.
Subtalar arthroscopy includes arthroscopy of the sinus tarsi and posterior and anterior subtalar joints.
ANATOMY
For arthroscopic purposes, the subtalar joint is divided into anterior (talocalcaneonavicular) and posterior (talocalcaneal) articulations (FIG 1).
The anterior and posterior articulations are separated by the tarsal canal, which has a large lateral opening called the sinus tarsi. The tarsal canal is filled with a thick interosseous ligament. Because of this ligament, there is usually no connection between the anterior and posterior joint complex.
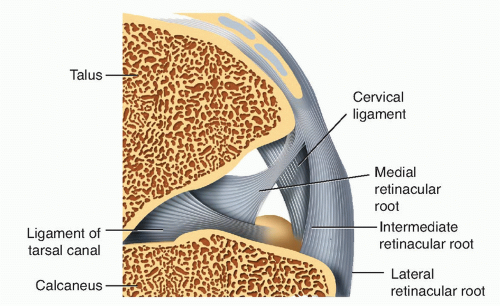
Within the tarsal canal and sinus tarsi are found the interosseous talocalcaneal ligament, the medial and intermediate roots of the inferior extensor retinaculum, the cervical ligament, fatty tissue, and blood vessels.5,6,8,12

FIG 1 • A,B. The subtalar joint is divided into the anterior (talocalcaneonavicular) and posterior joints (talocalcaneal).
The lateral ligamentous support of the subtalar joint consists of the lateral talocalcaneal ligament, the posterior talocalcaneal ligament, the lateral root of the inferior extensor retinaculum, and the calcaneofibular ligament (FIG 2).
The anterior subtalar joint is generally thought to be inaccessible to arthroscopic visualization because of the thick interosseous ligament that fills the tarsal canal and the ligaments that insert on the floor of the sinus tarsi.2,3,4,18 However, when there is a tear of the ligaments or they are débrided, the anterior joint can be visualized.
The posterior subtalar joint has a synovial lining. This joint has a posterior capsular pouch with small lateral, medial, and anterior recesses.
PATHOGENESIS
One of the most common indications for subtalar arthroscopy is chronic pain in the sinus tarsi, historically referred to as sinus tarsi syndrome.2
Sinus tarsi syndrome has been described as persistent pain in the tarsal sinus secondary to trauma (80% of the cases reported).2
There are no specific objective findings in this condition.
The exact etiology is not clearly defined, but scarring and degenerative changes to the soft tissue structure of the sinus tarsi are thought to be the most common cause of pain in this region.
Therefore, sinus tarsi syndrome is an inaccurate term that should be replaced with a specific diagnosis, as it can include many other pathologies, such as interosseous ligament tears, arthrofibrosis, and joint degeneration.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with subtalar joint pathology often present with lateral ankle pain that is aggravated by standing and walking activities, particularly on uneven terrain.
Walking on uneven terrain can result in a feeling of instability.
Motion of the subtalar joint is not simple inversion and eversion.8,12 However, motion is best tested by holding the left heel in the right hand and vice versa, then using the opposite hand to hold the forefoot and move the foot from inversion to eversion. This motion should be smooth and painless.
Inversion and eversion are coming primarily from the talocalcaneal (subtalar) joint. Exact measurements are difficult using standard techniques. Restricted motion may be seen with acute ankle sprain, arthritis, posterior tibial tendon dysfunction, tarsal coalition, fracture, chondral injury, adhesions, synovitis, and inflammatory conditions.
There may be swelling or stiffness in the joint.
Subtalar stiffness and pain indicate pathology in and around the subtalar joint but are not specific to one diagnosis.
Clinical examination reveals pain on the lateral aspect of the hindfoot aggravated by firm pressure over the lateral opening of the sinus tarsi.
Relief of symptoms with injection of local anesthetic directly into the sinus tarsi confirms the diagnosis of pain or dysfunction in the sinus tarsi.
Pathology of the interosseous ligaments of the subtalar joint usually is associated with focal pain over the lateral entrance to the sinus tarsi. Patients often have slight restriction and discomfort with passive subtalar motion.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Differential injections may be required to confirm pathology in the subtalar joint.
Anteroposterior (AP), lateral, and modified AP views of the foot are necessary to identify the subtalar joint.
The lateral and posterior processes are better seen on hindfoot oblique views.
The oblique 45-degree foot films show the anterior portion of the subtalar joint.
Broden view shows the posterior facet of the subtalar joint. This view is obtained by rotating the foot medially 45 degrees with dorsiflexion. The x-ray beam is pointed at the lateral malleolus and angled 10 degrees cephalad. Different views are obtained by changing the angle of the x-ray beam from 10 to 40 degrees.
Computed tomographic (CT) scans in the coronal plane are best for visualizing the talar body or posterior and lateral processes of the talus. CT can be used to show intraarticular pathology.
CT scans in the transverse or sagittal planes are best to visualize the talar neck and dome.
Magnetic resonance imaging (MRI) may detect chronic inflammation or fibrosis within the subtalar joint. Ligament injury, bone contusions, osteochondral lesions, chondral injury, impingement, synovitis, and fibrous or cartilaginous coalitions can be well demonstrated on MRI.
The preoperative imaging studies predict subtalar cartilage damage less accurately than does arthroscopy.
DIFFERENTIAL DIAGNOSIS
Chronic lateral ankle pain
Chronic ankle instability
Peroneal tendon pathology
Posterior tibial tendon dysfunction
Superficial peroneal nerve pathology
Fracture of the anterior process of the calcaneus
Fracture of the lateral process of the talus
Fracture of the posterior process of the talus
Navicular fracture
Calcaneal cuboid arthrosis/subluxation
Calcaneus fracture
Coalition
Posterior ankle impingement
NONOPERATIVE MANAGEMENT
Injection of anesthetic agent or corticosteroid
Foot orthosis, including a UCBL
Anti-inflammatory medication
Ankle brace with a hindfoot lock
Peroneal tendon strengthening
SURGICAL MANAGEMENT
Indications for subtalar arthroscopy include chondromalacia, subtalar impingement lesions, osteophytes, lysis of adhesions with posttraumatic arthrofibrosis, synovectomy, and the removal of loose bodies.1,2,4,7,11
Other therapeutic indications include instability, débridement and treatment of osteochondral lesions, retrograde drilling of cystic lesions, evaluation of coalition, removal of a symptomatic os trigonum, evaluation and excision of
fractures of the anterior process of the calcaneus and lateral process of the talus, and subtalar fusion.9,10,15,16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree