CHAPTER 14 Subscapularis and Rotator Interval Repair
Failure of subscapularis repair occurs in 2% of patients after shoulder arthroplasty for primary osteoarthritis.1 Prognostic factors for the development of symptoms after subscapularis failure are unclear. Many patients will be asymptomatic after failure of subscapularis repair, with subscapularis weakness detected only on postoperative examination. However, symptoms of weakness or anterior instability (or both) will develop in some patients. Additionally, even in patients who are asymptomatic, concern exists over subscapularis failure’s causing eccentric anterior loading and subsequent loosening of the glenoid component. For these reasons every effort should be made to perform a secure subscapularis repair. We prefer a repair that incorporates both transosseous and transtendinous components. In addition to subscapularis repair, we also routinely close the rotator interval to further decrease the risk for postoperative glenohumeral instability.
TECHNIQUE FOR REPAIR OF THE SUBSCAPULARIS AND ROTATOR INTERVAL
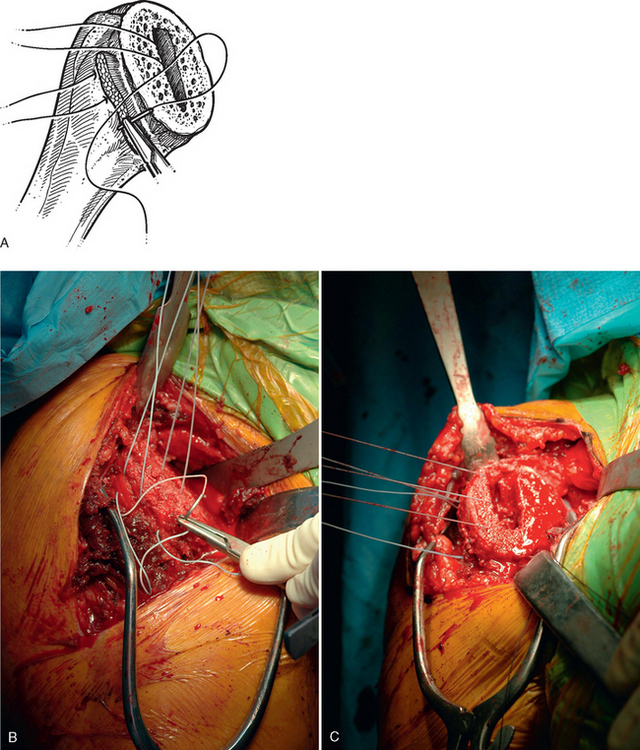
After completing soft tissue balancing, final preparations are made for implantation of the humeral component and subsequent subscapularis repair. Three no. 2 nonabsorbable braided sutures are placed through the lesser tuberosity and the humeral stump of the subscapularis tendon, as detailed in Chapter 11, to be used for reattachment of the subscapularis (Fig. 14-1). These sutures are placed just before insertion of the final humeral implant. The final humeral implant is then impacted into place and its stability checked (Chapters 11 and 13).
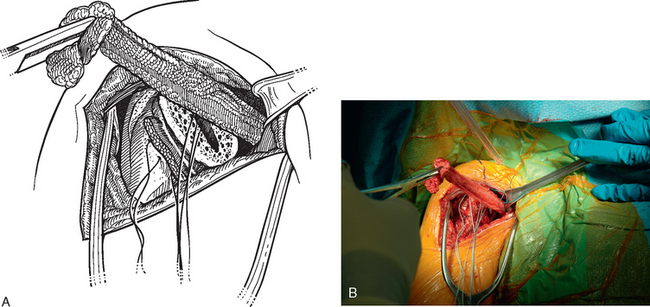
The small anterior glenoid rim retractor is removed and replaced with a narrow Richardson retractor, which is used to retract the conjoined tendon medially. The previously placed sponge is visualized and removed from the subscapularis fossa with a Kocher clamp (Fig. 14-2). Removal of this sponge reveals the stay sutures placed in the subscapularis tendon during the surgical approach. The Kocher clamp is placed on these stay sutures to obtain control of the subscapularis (Fig. 14-3). The limb of the superior suture exiting the medullary canal is passed from deep to superficial through the superior portion of the subscapularis tendon not more than 1 cm medial to its terminus. The same limb is then passed through the humeral stump of the subscapularis and back through the superior portion of the subscapularis tendon, as before (Fig. 14-4). This suture is tied with a square surgeon’s knot using five throws. The subscapularis stay sutures are removed, and the suture passing and tying procedure is repeated for the middle suture and then the inferior suture. This technique yields a transosseous and transtendinous repair (Fig. 14-5). No effort is made to imbricate the subscapularis or to medialize its insertion; the repair should be as anatomic as possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree