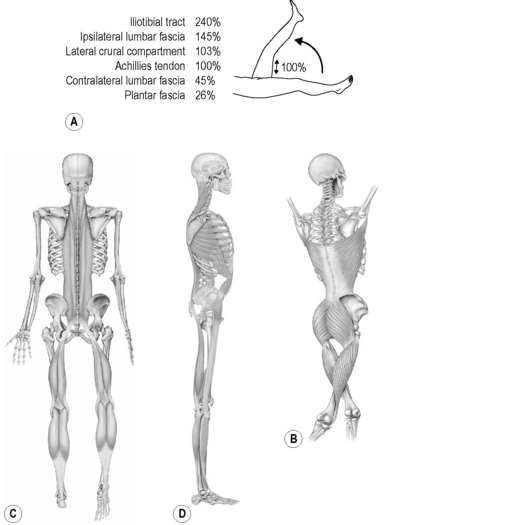
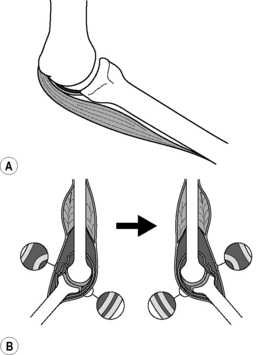
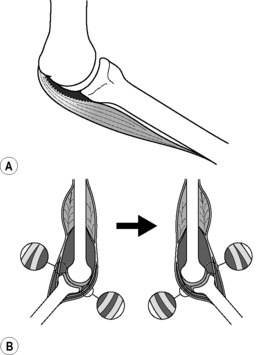
7.20 Stretching and fascia Active or passive soft-tissue stretch is routinely applied in: • manual therapies (massage, myofascial release, active release, muscle energy) • rehabilitative physiotherapy protocols (pre-postsurgical, post-traumatic) • performance enhancement (athletic, dance, active isolated stretching) • self-help methods (yoga, exercise warm-up/cool-down routines) • integrative pattern resolution (osteopathy, structural integration). Additional variables can pertain. Since tension and compression always coexist at 90 degrees to each other, when any given tissue is tensioned in one direction, cells and matrix are also compressed at right angles to the tension (Fuller 1975). Additionally, a linear stretch will be converted in the complexities of fibrous connections to bending, shear, or torsion in surrounding or ‘downline’ tissues (Franklyn-Miller et al. 2009). To be therapeutic, stretching should stay within the physiological range; overstretching can produce injury (Alter 2004). Indeed, many soft-tissue injuries are seen as the sequelae of local tissues being stretched excessively and too rapidly. Despite ubiquitous therapeutic and performance-based stretching, research is still divergent regarding its efficacy (Bovend’Eerdt et al. 2008). Most studies limit themselves to one or two types of stretch techniques, using restricted parameters of intensity and duration (Law et al. 2009). Few have studied the movement-based dynamic stretching that currently prevails in performance training and manual therapy. No consistent guidelines exist for practitioners or movement educators as to optimal measures of intensity, duration, or frequency (da Costa & Vieira 2008). Another factor in the lack of consistency in stretching research is that the organized study of the biomechanical properties of the various topologies and histologies of connective tissues is still in its infancy. Little is definitively known about lengthening and remodeling responses in vivo in anatomically intact tissues, as opposed to single structures isolated for testing in vitro (Standley 2009; Solomonow 2009). Additionally, the broad emphasis on single-unit muscle stretching needs to be reconsidered in terms of new anatomical models linking muscles, fascia, and ligaments in dynamic series, rather than distinct parallel units that can be treated in isolation (Vleeming 2007; van der Wal 2009; Stecco & Stecco 2009). The evidence is quite clear: the use of the word ‘isolated’ in conjunction with the word ‘stretching’ is difficult to justify when a straight leg lift test produces 240% of the strain in the iliotibial tract that it does in the hamstrings (Fig. 7.20.1) (Franklyn-Miller et al. 2009). • mechanical lengthening (and resulting segmental realignment) • direct stimulation of connective tissue cells, notably fibroblasts. All mammals display inflammatory responses to a wide range of trauma or infection from viruses or bacteria, and part of that involuntary response can be neuromyofascial tissue contraction (Grinnel 2009). Humans also respond to stresses at various levels via skeletal and smooth muscle contraction. Long-term problems arise not so much with reflexive or attitudinal hypertonic responses, but rather due to lack of a post-response return to normal states of tone and tissue relaxation, even after the threat, trauma or stress has passed. The subsequent cascade of soft-tissue and skeletal compensations automatically ensues to adapt function to what can become a chronic state of myofascial contraction, increased myofibroblast activity, and fascial tissue contracture (Schleip et al. 2005; Langevin et al. 2009). Many clinicians and researchers propose that chronic ‘below the voluntary’ muscle contraction eventually results in fascial ‘thickening’ (Langevin et al. 2009) or ‘densification’ (Stecco & Stecco 2009) or binding among layers that should slide on each other (Fourie 2009) in various parts of the ECM. These patterns result in chronic eccentric as well as concentric tissue loading, which taken together form body-wide ‘soft tissue holding patterns’ (Myers 2009). The areolar tissue between the skin and the ‘unitard’ of the fascia profundis shows significant viscoelastic properties, allowing for immediate changes in architecture to accommodate changing forces (Myers 2009). This tissue demonstrates many interesting effects in direct cellular signaling, and is easily accessible for, and accommodative of, lengthening in response to an applied uniaxial stretch (Iatrides et al. 2003; Wang et al. 2009). Within and around the muscle, the fasciae can be histologically divided into the endomysium around myofibrils, the perimysium around fiber bundles, and the epimysium around the muscle itself. Distribution of each of these varies widely between muscles (Purslow 2002). The dual needs for force transmission through the ‘myofascial unit’ while accommodating the vascular supply to the muscle cells dictate that both shear and longitudinal strains through the muscle will not be uniform through different phases of contraction and loading. This suggests that most of the ‘release’ felt in myofasciae during manual therapy is due to muscular relaxation rather than actual lengthening of the fascial elements. To the degree that some mechanical lengthening is available in the myofasciae, research suggests the perimysium may be the most easily adaptable of these three layers (Purslow 2002). Tendons themselves show little propensity for changing resting length during the application of manual therapy; indeed, they would be poor choices for creating postural and joint stability if they were subject to such deformation. Ligaments vary in their composition, depending on how elastic they need to be, but ligaments with less elastin have been shown to respond elastically to short-term displacement, and with creep to long-term loading, but there is no evidence to show that ligaments will accept a permanent length change with the forces applied in short-term manual therapy (Solomonow 2009). In dense connective tissue structures such as the iliotibial tract and plantar fascia, it is now evident that the clinician’s feeling of ‘fascial lengthening’ is not coming from actual elongation in the fascial sheet itself, as the forces necessary to lengthen these dense fasciae are far beyond what can be generated therapeutically (Chaudry et al. 2011). A more likely mechanism is that via neurological feedback, muscles in series with the fascia treated are relaxing to produce the feeling of release (Schleip 2003). A ‘map’ of the architecture of the ECM requires knowing where each structure ‘should’ be tied down to surrounding structures, and where it should slide relative to others (Fourie 2009). In addition to mechanical lengthening of tissues, dysfunction (and apparent ‘shortness’) is surmised to come from adjacent fasciae losing serous lubrication between layers, and the establishment of cross-linkages that will not allow movement between those layers. Thus, stretching can be applied not only to ‘length’ problems, but also to ‘stuck layer’ problems. By fixing one layer and requiring stretching movement of the adjacent layer, shear stress is created that allows the restoration of increased relative movement between the adjacent planes of fascia (Schwind 2006). Anatomical research concludes that muscles attach and function with connective tissue, primarily in series rather than the traditionally assumed parallel arrangement (van der Wal 2009) (Fig. 7.20.2). Since each muscle slip attaches to fascial expansions that then attach to periosteum–ligaments–joint capsules, which ultimately attach to bone, a stretch designed to target a supposedly ‘isolated’ muscle can be directed laterally, obliquely, or longitudinally to other nearby structures (Franklyn-Miller et al. 2009). Fig. 7.20.2 • Ligaments, thought to run parallel with overlying muscles (A), can more accurately be viewed as acting in series with nearby muscles (B) (van der Wal 2009). From van der Wal J 2009 The Architecture of the Connective Tissue in the Musculoskeletal System in Fascia Research II: Basic Science and Implications for Conventional and Complementary Health Care, Munich: Elsevier GmbH.
Introduction
Definition
Mixed evidence
Stretching: the evidence for tissue change
Mechanical lengthening
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Stretching and fascia