Staged Digital Flexor Tendon Reconstruction
Sebastian C. Peers
Kevin J. Malone
DEFINITION
Staged flexor tendon reconstruction is required in the settings of delayed diagnosis of a flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) disruption or failed previous attempt at primary repair within zone II of the digital tendon sheath.
During the first stage of the reconstruction process, a silicone rod is placed within the flexor tendon sheath. The role of this implant is to help reestablish a frictionless inner lining of the sheath that will accommodate the placement of a tendon graft in the second stage.
ANATOMY
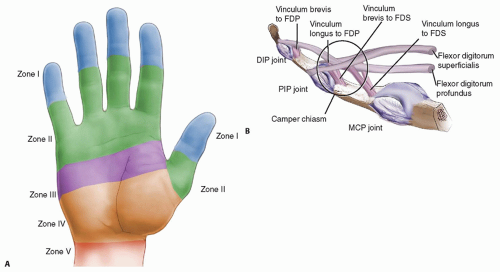
Flexor tendons can be divided into five zones (FIG 1A).
Bunnell originally described the region between the A1 pulley and the FDS insertion, zone II, as “no man’s land” because the initial results after attempted primary tendon repair were so poor he felt that no one should attempt this procedure.
In the limited confines of zone II, the two flexor tendons function together and rely on the digital sheath and its frictionless synovial interface for gliding and proper function.
Another complicating anatomic characteristic of zone II is the chiasm of Camper. Here, FDP passes through the slips of FDS, creating another potential region for adhesions (FIG 1B).
PATHOGENESIS
Zone II has the highest probability of developing adhesions and the poorest prognosis after repair.
Violation of the sheath, the lining, or the blood supply to the tendons by trauma or infection may lead to dense scar and adhesion formation and can compromise the results after either a primary repair or an attempt at single-stage reconstruction with a tendon graft.1
NATURAL HISTORY
Flexor tendon injuries that are not reconstructed can progress to a stiff and sometimes painful digit.
If both tendons are not functional, no active proximal interphalangeal (PIP) or distal interphalangeal (DIP) motion will be possible, but if only the FDP tendon is disrupted, active PIP flexion will be present.
If a digit with incompetent flexor tendons is subjected to repeated extension stress, as in pinch, the volar supporting structures will become lax over time, leading to hyperextension and an unstable joint.
PATIENT HISTORY AND PHYSICAL FINDINGS
The examiner should elicit information about the initial injury, such as when it occurred and if there were associated injuries (fractures, laceration of digital nerves or vessels).
The examiner should determine when the patient first noticed a decrease in the function of the digit (if flexor tendon repair has already been attempted).
Staged flexor tendon reconstruction is contraindicated in the setting of an active infection, and for that reason, an infection history must be sought.
If an infection is identified, it should be treated aggressively with antibiotics and débridement to minimize the destruction of the flexor tendon sheath from the inflammatory process.
Tests for tendon function include the following:
Finger cascade: Loss of the normal cascade suggests disruption or loss of function of the flexor tendons.
FDP examination: Loss of active DIP flexion suggests disruption or loss of FDP function.
FDS examination: Loss of active PIP flexion suggests disruption or loss of FDS function.
Tenodesis effect: Loss of the tenodesis effect suggests disruption of the flexor tendons.
It is also important to assess the vascular supply and the digital sensation to determine if there is a concomitant injury to the digital neurovascular structures.
Both active and passive range of motion must be recorded for the metacarpophalangeal (MP), PIP, and DIP joints.
If contractures are present, as evidenced by decreased passive joint motion, intensive therapy should be initiated before proceeding with staged flexor tendon reconstruction.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs should be obtained to rule out fractures or other associated injuries to the hand and digits.
Ultrasound or magnetic resonance imaging (MRI) can be used to help localize the site of tendon rupture and position of the proximal stump if not clear by clinical examination.
DIFFERENTIAL DIAGNOSIS
Fracture or dislocation of digits
Proximal compression of anterior interosseous nerve, median nerve, or ulnar nerve
Cervical radiculopathy
Upper motor neuron lesion
NONOPERATIVE MANAGEMENT
There is no acceptable nonoperative management for combined FDS and FDP tendon lacerations. Alternatives to staged flexor tendon reconstruction include arthrodesis and amputation.
Isolated chronic disruption of the FDP tendon with an intact FDS tendon is best treated nonoperatively. Attempts at reconstruction of the FDP tendon risk function of the FDS tendon.
Buddy taping or trapping of the injured finger by an adjacent figure during finger flexion may allow concealment of the functional deficit between stage 1 and stage 2 or in the patient who is not a candidate for staged tendon reconstruction.
SURGICAL MANAGEMENT
Indications for two-stage flexor tendon reconstruction include the following:
Loss of FDP and FDS
Protective sensation
Nearly full passive range of motion
Good-quality skin in the region of zone II
A cooperative patient willing to participate fully in rehabilitation
The patient will need to have access to a good hand therapist before and after each of the stages of this complex reconstructive process.
Preoperative Planning
For the second stage of the procedure, a tendon must be harvested to use for the reconstruction. Often, a palmaris longus graft is used. If the patient does not have a palmaris longus, then a long toe extensor or plantaris tendon can be used. In this situation, the lower extremity must also be prepared out into the surgical field.
As an alternative to a traditional free tendon graft, the proximal end of the lacerated FDS may be used as graft. Paneva-Holevich7 first described this technique in 1965. It has since been refined and is described as the modified Paneva-Holevich technique6 in this chapter. If this technique is selected, the proximal tendon stumps of FDS and FDP are sutured together in the shape of a “loop” during the first stage.
Positioning
For both stages of the procedure, the patient is placed supine on the operating table with the arm abducted on a hand table. A nonsterile tourniquet is placed around the upper arm for hemostasis.
Approach
Stage 1: A volar Brunner incision is made over the flexor tendon sheath and extended proximally into the palm. A second incision is made in the distal forearm to ensure placement of the rod within the carpal tunnel.
Stage 2: A limited Brunner incision is made at the level of the distal junction of the repair. A separate incision is made at the level of the proximal junction of the repair. This can be the same incision in the distal forearm as in stage 1 if the tendon graft is long enough. Alternatively, the proximal junction will be in the palm with shorter tendon grafts. A third incision or set of incisions will be made for the tendon harvest. If the modified Paneva-Holevich technique is used, a third incision at the musculotendinous junction of the FDS tendon is used.
TECHNIQUES
▪ Stage 1
A volar Brunner incision is made over the course of the flexor tendons.
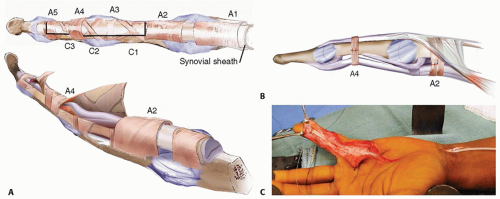
The flexor tendon sheath is incised, taking care to preserve the A2 and A4 pulleys. L-shaped flaps can be made within the flexor sheath to aid in access to the flexor tendons and protect the A2 and A4 pulleys (TECH FIG 1A).
The scarred tendon is excised, leaving a portion of the distal stump of the FDP intact at its insertion.
This is useful in securing the tendon rod in stage 1 and the tendon graft in stage 2.
If a digital nerve laceration is identified, it should be repaired at this stage.
Release any adhesions within the sheath.
Release any flexion contractures of the joints by releasing the volar plate and accessory collateral ligaments.
Be sure to preserve the proper collateral ligaments.
If the A2 or A4 pulleys are absent or have been excised with the scar release, they need to be reconstructed. A tendon graft can be used to reconstruct the pulleys (TECH FIG 1B).
The tendon should be passed between the proximal phalanx and the extensor tendon for A2 reconstruction.
For A4 reconstruction, the tendon can be passed dorsal to the extensor tendon.
A silicone Hunter rod is inserted into the sheath. Distally, it is secured to the remnant of the FDP tendon with nonabsorbing suture.
If there is not enough of the tendon remnant, it can be secured to surrounding tissue at the base of the distal phalanx.
Some Hunter rods can be secured using a screw placed in the distal phalanx.
Proximally, the silicone rod is passed through the carpal tunnel and allowed to glide free with the flexor tendons in the distal forearm (TECH FIG 1C).
All skin incisions are closed with 4-0 nylon after ensuring hemostasis.
The patient is then placed into a dorsal blocking splint holding the fingers into an intrinsic plus posture.
Rehabilitation is started early after surgery, often within 1 week, to ensure that the patient regains full passive range of motion. The scar tissue must be soft and supple before the patient is scheduled for the second stage of tendon reconstruction. On average, this takes 3 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree