Squamous Cell Carcinoma and Melanoma of the Hand
Patrick Cole
Yoav Kaufman
Jason Petrungaro
DEFINITION
Squamous cell carcinoma (SCC) and melanoma are malignant transformations of normal epidermal cells in either cutaneous or noncutaneous regions of the body.
Both SCC and melanoma demonstrate the ability to extend locally, involve regional lymph node basins, and metastasize to distant sites. SCC is also prone to locally extending along nerves sheaths.
Early diagnosis, accurate histopathologic evaluation, detailed staging, appropriate surgical, and medical management as well as appropriate follow-up are critical to the management of SCC and melanoma of the hand.
ANATOMY
Intact skin is composed of epidermis and dermis. These act as physiologic barriers to infection and malignant spread. SCC and melanoma develop from different epidermal layers.
SCCs develop from epidermal keratinocytes.
Melanomas derive from dendritic (neural crest) cells within the epidermis. Melanomas are typically pigmented; however, amelanotic melanomas (nonpigmented melanoma) represent 5% of all melanomas.
PATHOGENESIS
The typical SCC lesion is a firm, scaly papule or nodule containing a central ulcer surrounded by an indurated raised border (FIG 1).
Risk factors include the following:
Repetitive damage from sun, heat, and wind
Severe burns and chronic ulcers
Advanced age
Immune compromise (organ transplantation and AIDS)
Major risks for melanoma include the following:
Personal or family history of melanoma
Propensity for sunburn with excessive sun exposure
Immune compromise

FIG 1 • The typical SCC lesion is a firm, scaly papule or nodule containing a central ulcer surrounded by an indurated raised border.
Previous skin cancers
Exposure to coal tar, radiation, or radium
NATURAL HISTORY
SCC is the second most common type, behind basal cell carcinoma (BCC).
The American Cancer Society estimates more than 1 million new diagnoses of cutaneous BCC and SCC are made annually. However, BCC and SCC account for less than 0.1% of patient deaths caused by all cancers.
The American Cancer Society anticipates approximately 60,000 new melanoma cases each year, with an estimated 8110 deaths.
The probability of developing melanoma from birth to death is 2.04 (1 in 49) in males and 1.38 (1 in 73) in females.
Nail matrix SCC or melanoma account for less than 1% of their respective cutaneous malignancies. The histologic features of the epidermis and dermis, including physiologic barriers, are absent in the nail complex. In the nail complex, the matrix is adherent to the underlying phalanx.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients typically present for evaluation after noting the recent appearance of, or changes to, an existing lesion.
Change in size, shape, coloration, the presence of satellite lesions, or ulceration of a lesion should prompt a thorough evaluation and possible biopsy with histopathologic analysis (FIG 2).
Melanoma and SCC can metastasize. Regional lymph node beds (axillary) should be routinely examined in all suspected cases of upper extremity skin cancer.
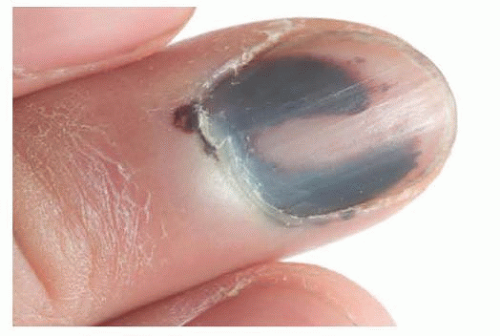
The presence of a Hutchinson sign (extension of brown-black pigment from the nail bed, matrix, or nail plate onto the adjacent cuticle and proximal or lateral nail folds) is consistent with a subungual melanoma (FIG 3). Subungual melanoma should also be suspected when the nail bed contains a new or enlarging pigmented streak wider than 3 mm (FIG 4).
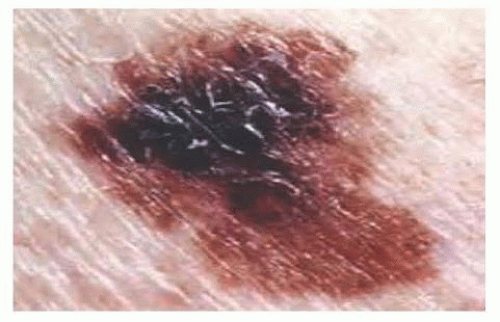
FIG 2 • Change in size, shape, border irregularity, coloration, the presence of satellite lesions, or ulceration should prompt a thorough evaluation and biopsy.
Although there have been reports of amelanotic melanoma of the nail bed, the actual incidence is unknown.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographic evaluation of the hand with plain view x-rays are helpful and may reveal bone involvement (FIG 5).
For both SCC and melanoma, a chest radiograph, complete blood count, and liver panel may be obtained. If these labs reveal abnormality, prompt evaluation by an internist or oncologist is appropriate.
More detailed imaging studies (computed tomography [CT], magnetic resonance imaging [MRI], and positron emission tomography [PET]) may be performed to evaluate specific organ systems (central nervous system, pulmonary, gastrointestinal, and others) if indicated.
The diagnosis of skin cancer requires adequate histopathologic evaluation with a full-thickness (surface to full depth) specimen.
Suspicious pigmented lesions must never be shaved, cauterized, or vaporized for fear of losing the opportunity to accurately identify the lesion depth.
SCC is graded 1 to 4 based on the proportion of differentiating cells present and the frequency of atypical tumor cells.
Melanoma subtypes include the following:
Superficial spreading: most common, 70%
Nodular: 15% to 30%, more aggressive
Lentigo maligna: most common subtype among Asians and African Americans
Acral lentiginous (palmar-plantar and subungual)
Miscellaneous unusual types are as follows:
Mucosal lentiginous (oral and genital)

FIG 4 • Subungual melanoma should also be suspected when the nail bed contains a new or enlarging pigmented streak wider than 3 mm.

FIG 5 • Radiographic evaluation of the hand with plain view x-rays are helpful and may reveal bone involvement.
Desmoplastic
Verrucous
Malignant melanoma staging is determined by histopathologic evaluation of the vertical thickness of the lesion in millimeters (Breslow classification) or the anatomic level of local invasion (Clark classification).
Along with the presence of ulceration, Breslow thickness more accurately predicts melanoma behavior in lesions thicker than 1.5 mm. Estimates of prognosis should be modified by sex and anatomic site in coordination with clinical and histologic evaluation.
The Clark classification ranges from level I (in situ lesions involving only the epidermis) to level V (invasion through the reticular dermis into the subcutaneous tissue).
Micrometastases are diagnosed by elective sentinel lymphadenectomy.
Macrometastases are defined as clinically detectable lymph node metastases confirmed by therapeutic lymphadenectomy or when any lymph node metastasis exhibits gross extracapsular extension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree