Chapter 33 Sports Injuries of the Elbow
Background/aetiology
Injury and reconstruction of the UCL enjoys great notoriety in the world of sports. Injury to the UCL was first described in javelin throwers in 1946.1 Perhaps due to incomplete understanding of the injury and its effect primarily on throwing athletes, little was written about the subject for the next 40 years. Interest in this injury was renewed with the first description of reconstruction of the UCL by Jobe et al in 1986.2 This was spurred in no small part by the widely publicized success of Dr Jobe’s reconstruction on major league baseball pitcher Tommy John in 1974. Known since as the ‘Tommy John surgery’, a great deal of research has furthered the understanding of UCL anatomy, the way it is injured, and the optimal treatment and rehabilitation.
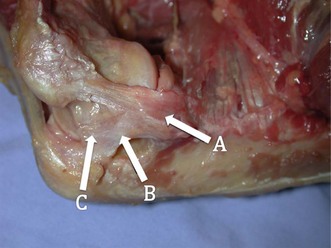
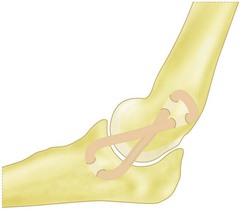
Understanding the injury and treatment of UCL tears in overhead throwers begins with an understanding of the anatomy of the medial side of the elbow. The UCL is consistently made up of an anterior and posterior bundle, with a variable transverse bundle (Fig. 33.1). Within the UCL complex, the primary restraint to valgus stress is the anterior bundle, which originates on the inferior-most aspect of the medial epicondyle of the humerus and inserts on the sublimus tubercle of the ulna. The anterior bundle is further divided into an anterior band, which is tighter in extension, and a posterior band, which is tighter in flexion. An anatomical study by Callaway et al confirmed this characterization of the bands as ‘reciprocal’ in their roles of stabilization through the flexion-extension arc.3 The authors found that the anterior band was the primary stabilizer at 30°, 60° and 90°, while the anterior and posterior band were co-primary stabilizers at 120°. The posterior bundle lends little to the valgus stability as long as the anterior bundle remains intact, except at 30° of flexion, where it is a secondary stabilizer.
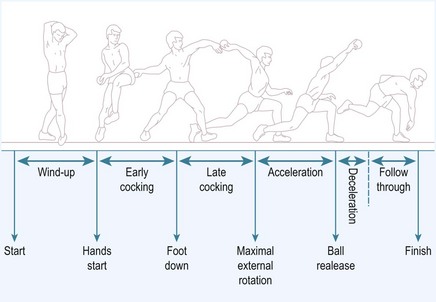
Injury to the UCL occurs as either a single traumatic event or from cumulative injury and repetitive loads experienced by the elbow during athletic activities. With overhead throwing, the UCL is most at risk during the late cocking and early acceleration phases of pitching, with the upper extremity achieving a peak angular velocity in the range of 2300–5000°/sec3 (Fig. 33.2). This finding is supported clinically by the fact that severe pain during the throwing motion occurs most commonly during the acceleration phase.4 Further, biomechanical studies have demonstrated the ultimate load to failure of the native anterior band of the UCL in resisting valgus torque to be 34 Nm,5 while the estimated demand on the UCL during pitching has been demonstrated to be 35 Nm.6 With estimated demand so near to the load to failure, it is not surprising that overhead athletes, especially baseball pitchers, are prone to an injury of this ligament.
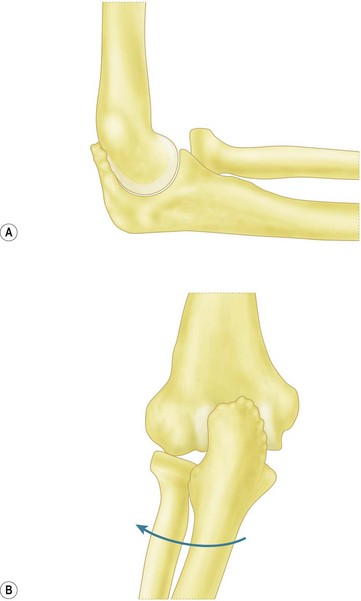
Repetitive throwing can also lead to a spectrum of pathology involving the UCL, ranging from attenuation to partial or complete tears. As UCL insufficiency progresses, coincident pathology can also develop, including radiocapitellar arthritis, ulnar neuropathy, and valgus extension overload syndrome (VEOLS). VEOLS results from the valgus force on the elbow during the early acceleration phase of throwing and from the compression of the posteromedial olecranon against the olecranon fossa as the elbow is extended in the ‘follow through’ phase. Patients present with posteromedial elbow pain along the border of the olecranon.7 These elevated loads on the elbow may lead to the formation of osteophytes at the posterior and posteromedial tip of the olecranon with associated cartilage wear and loose bodies (Fig. 33.3).
Similar symptomatology and pathology can also develop in young pitchers. In one series, 28% of adolescent pitchers experienced elbow pain over a course of 2 years.8 However, unlike adults, the presence of physeal plates in the youth elbow leads to a different pattern of injury.9 Whereas valgus torque may lead to injury to the UCL in adults, similar stresses lead to medial epicondylar apophysitis or avulsion fractures in children and adolescents.10 Sabick et al studied the valgus torque on the elbow in adolescent baseball pitchers based upon video data.9 Controlling for height and weight and taking only kinematic variables, they found maximum shoulder external rotation to be the most significant variable in the generation of elbow valgus torque. Thus, a pitching style that eliminates exaggerated shoulder external rotation may help to prevent elbow injury.
Other authors have suggested guidelines to help diminish the risk to young pitchers such as limiting pitch counts per game and per season.8 At greater than 75 pitches per game, the odds of elbow pain increases by 50%. Pitch counts of greater than 600 per year also correlated with increased risk of elbow pain. In addition, proper instruction in mechanics and avoidance of pitching while fatigued are important. Specific pitch types, such as the slider and curveball, and a sidearm delivery have also been reported to increase the risk of elbow pain.4 Thus, it is important for coaches and leagues to adhere to pitch count guidelines based upon the athlete’s age, instruct in proper mechanics from a young age, and monitor their players’ development of these specific pitches (Table 33.1).
Table 33.1 Little league baseball pitch count rules
| League age (years) | Pitchers per day |
|---|---|
| 13–16 | 95 |
| 11–12 | 85 |
| 9–10 | 75 |
| Under 8 | 50 |
| Pitch count | Days of rest |
|---|---|
| 61 pitches per day or more | 4 |
| 41–60 pitches | 3 |
| 21–40 pitches | 2 |
| 1–20 pitches | 0 |
Presentation, investigation and treatment options
Injuries to the UCL in the overhead athlete may present with acute or insidious symptoms during throwing. Athletes may recount a history of acute medial-sided elbow pain during a pitch together with a popping sensation. More commonly, pitchers describe a gradual onset of pain, accompanied by loss of velocity or ball control.11 Pain is usually greatest during the late cocking and early acceleration phases of the throwing cycle. In addition, patients with valgus extension overload syndrome may experience posteromedial pain during deceleration due to osteophyte impingement. Occasionally, patients may also describe a sensation of instability or ‘opening’ in the elbow while throwing.12 Finally it is important to question the athlete about ulnar nerve symptoms during competition or at rest.
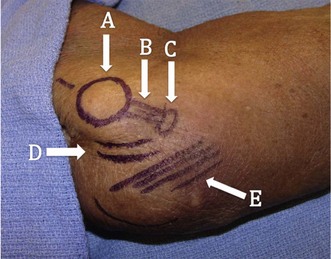
Physical examination of these patients begins with a basic evaluation of the joint. Patients will often exhibit tenderness to palpation over the UCL most often at the distal insertion site at the sublime tubercle12 (Fig. 33.4). Additionally, patients may display tenderness over posterior or posteromedial osteophytes and pain with forced extension of the elbow. In the setting of arthritis, loose bodies, or osteophytes, range of motion may be reduced.7 A complete neurovascular examination should be performed with special attention paid to ulnar nerve. This should include both an examination for a Tinel’s sign and inspection for subluxation of the nerve over the medial epicondyle during flexion and extension. The presence of both or either of these findings will guide intraoperative decisions regarding handling of the nerve.
Various specific physical examination manoeuvres have been described to assess valgus instability. Positioning the elbow in 20–30° of flexion unlocks the olecranon from the fossa, decreasing osseous stability and more accurately testing the anterior band of the UCL. By applying a valgus stress while palpating the ligament and comparing to the contralateral side, the examiner may be able to detect instability.12 Additionally, a valgus stress can be applied by placing the patient’s shoulder at 90° of abduction and maximal external rotation locks the shoulder. By pulling on the thumb in this position, a valgus load is applied to the elbow.
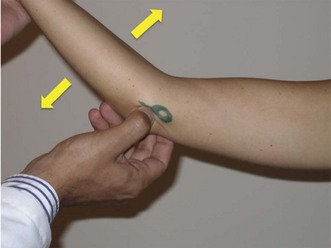
The milking manoeuvre (Fig. 33.5A) is a provocative test designed to preferentially stress the posterior portion of the anterior bundle of the UCL. The test involves the patient grasping the thumb of the affected arm while the affected elbow is supported with the other forearm.13 With traction applied to the thumb, the elbow is forced into valgus. Additionally, the examiner can palpate the ligament during this manoeuvre. Safran et al have described a modification of this milking maneuver.14 Once again, the patient stabilizes the affected elbow in supination and 90° of flexion, but the examiner pulls the affected thumb. Elicitation of pain is a positive finding (Fig. 33.5B).

(B) Modified milking manoeuvre. The patient supports the affected elbow while the examiner pulls on the patient’s thumb to create a valgus force.
(Reprinted with permission from Meyers A, Palmer B, Baratz ME. Ulnar collateral ligament reconstruction. Hand Clin 2008; 24(1):53–67.)
O’Driscoll et al have described the ‘moving valgus stress test’ and reported a 100% sensitivity and 75% specificity.15 To perform this test, the patient is positioned upright with the shoulder abducted to 90°. A modest valgus torque is placed on the forearm until the shoulder reaches its maximum external rotation. Starting with the elbow in maximal flexion, the elbow is rapidly extended to 30° while maintaining a constant valgus force. Two components comprise a positive result. First, the test must elicit pain similar to that during the act of throwing. Secondly, the maximal pain must occur between the position of late cocking (120°) and early acceleration (30°) of elbow flexion (Fig. 33.6).
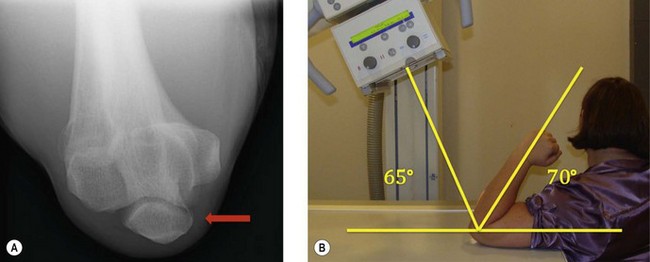
Imaging studies are also an important aid in the diagnosis of UCL tears. Plain radiographs of the affected elbow should be obtained to determine any radiocapitellar pathology, loose bodies, or calcification within the ulnar collateral ligament. Oblique radiographs as well as an axial view of the olecranon may help to identify posteromedial osteophytes7 (Fig. 33.7). Previously stress radiographs were also undertaken and found to be of some additional diagnostic value. However, these have now largely fallen from favour due to a high incidence of false positives and a lack of reproducibility. Ellenbecker et al compared the findings of stress radiographs between dominant and non-dominant elbows in 40 asymptomatic high-level baseball players.16 The authors found a significantly greater difference in joint space opening between the stressed and unstressed states in the dominant elbow, showing a natural tendency to increased laxity. In addition, Azar et al found positive results with stress radiographs in only 46% of athletes whose clinical findings led to operative treatment for a UCL injury.17
Magnetic resonance imaging with and without arthrography is a powerful diagnostic tool for evaluating the UCL. Calcification seen within the substance of the UCL on MRI has been associated with chronic partial or complete rupture of the ligament.18 Timmerman et al compared the findings of MRI without arthrography to intraoperative findings in 25 baseball players with a history and examination suggestive of UCL tears.19 The authors reported a 57% sensitivity and 100% specificity. Specifically, MRI without arthrography was sensitive in detecting full thickness tears, but only detected partial tears in 14% of cases. The addition of arthrography to MRI improved the sensitivity of the test to 86% in one series.20 The addition of contrast allows for improved visualization of the undersurface of the UCL, allowing better identification of partial tears. In addition, contrast allows visualization of the UCL recesses, which are potential spaces between the ligament and the epicondyle proximally and the ulna distally. The distal insertion of the ligament should be visualized within 1 mm of the articular margin of the coronoid process. Extension of contrast beyond these recesses is indicative of a tear UCL. Thus, whilst injection of contrast adds to morbidity and patient discomfort, it is now the study of choice for most clinicians. However, it is important to recognize that a negative study does not preclude a tear.20
Additional studies include CT arthrogram. Timmerman et al reported a sensitivity of 86% and specificity of 91% in a population of baseball players.19 In addition, the authors described a radiographic ‘ T-sign’ which represents an undersurface tear of the UCL. The undersurface tear of the ligament allows dye to leak around the detached insertion but remains ultimately contained within the superficial layer of the ligament and capsule (Fig. 33.8).

(B) CT arthrogram ‘T-sign’. Positive finding of dye extravasation along the proximal ulna beyond the insertion of the ligament (arrow).
Once the diagnosis is established, treatment must be individualized to the patient based upon their level of impairment, functional demands, desire to continue in their sport, and willingness to undergo the lengthy process of surgery and rehabilitation. Dysfunction from UCL tears usually occurs only in overhead athletes when throwing or performing equivalent activities such as spiking a volleyball. Thus, patients who are able to avoid these activities in their sport can usually be treated without surgery.21,33
Non-operative management generally includes rest from throwing for 2–4 weeks with the application of physical therapy modalities such as phonophoresis, iontophoresis, or electrical stimulation.12 Patients progress to a programme promoting elbow range of motion, flexor-pronator strengthening, and a progressive throwing programme at approximately 3 months.12,42 One study has reported success with nighttime splinting and progressive physical therapy in 42% of throwing athletes.21 Patients who fail a thorough attempt at non-operative treatment and wish to return to their sport are candidates for surgical treatment.
Contraindications to surgical management include patients with asymptomatic tears of the UCL.33 Given the sensitivity of magnetic resonance imaging (MRI) with arthrogram, pathology of the UCL may be detected that is not clinically relevant. Although, the natural history of asymptomatic partial tears has not been established, surgery is not indicated in such patients. In addition, certain athletes may be able to modify their activities to lessen valgus load on the elbow, making surgery unnecessary. A relative contraindication to ligament reconstruction is concomitant ulnohumeral or radiocapitellar arthritis.23 With reconstruction, such patients may experience worsened joint pain.
Surgical techniques and rehabilitation
Various modifications and refinements of UCL reconstruction have been made since Dr Jobe’s first description of the procedure in 1986.2 However, the goal of the procedure remains the same: to stabilize the elbow against the extreme valgus forces encountered during the late cocking and early acceleration phases of the throwing cycle.
Although, not performed on a routine basis, arthroscopy is an important tool in treating patients with UCL rupture. Field et al has described an arthroscopic valgus instability test of the elbow.22 Viewed from the anterolateral portal, a valgus stress is applied to the elbow, which is flexed between 60° and 75° with the forearm in pronation. A positive result corresponds with a visible opening in the ulnohumeral articulation of 1 mm or more.
In addition to diagnosis of instability, arthroscopy can be important in diagnosing and treating concomitant intra-articular pathology. In one report, routine arthroscopy was performed prior to reconstruction of the UCL. The authors removed osteophytes from either the posteromedial olecranon or the coronoid process in 29% of cases, performed microfracture on cartilaginous defects in 9%, and removed loose bodies in 7%.11 While some surgeons may prefer to forgo routine arthroscopy due to challenges in positioning and additional time added to the procedure, it may augment treatment of patients with valgus extension overload syndrome (VEOLS), especially those with intra-articular symptoms.
It is our practice to perform arthroscopic resection of posteromedial osteophytes in patients with posteromedial pain from VEOLS. Failure to identify and treat this related problem leads to continued pain from impingement of these osteophytes against the articular wall of the olecranon fossa and possible need for reoperation.7 However, there continues to be some concern that olecranon resection may lead to a loss of ulnohumeral constraint and as a consequence increasing strain on the UCL. Andrews et al found that 25% of professional athletes who underwent debridement of posteromedial osteophytes developed valgus instability requiring UCL reconstruction.25 Reports vary on the amount of olecranon that can be safely resected, ranging from 3 to 8 mm.24,26
After any intra-articular pathologies are addressed, attention can be turned to reconstruction of the UCL. If the surgeon has elected to position the patient in a lateral decubitus position for elbow arthroscopy, the patient is then turned to a supine position with the arm abducted and supported on a table. A tourniquet should be used to control bleeding. A longitudinal 6 cm curvilinear skin incision is made centred over the medial epicondyle. Care must be taken to protect branches of the medial antebrachial cutaneous nerve as they cross the distal aspect of the incision. In his original description of the procedure, Dr Jobe described detachment of the flexor-pronator mass.2 However, in an effort to limit damage to this structure, which is important in throwers, most authors now utilize a muscle-splitting approach to expose the UCL.11,17,27–30 Thompson et al described this approach as a splitting of the fascia over the muscle fibres beginning at the anterior portion of the anterior band of the UCL.30 An intramuscular interval is developed bluntly between the two heads of the flexor carpi ulnaris (FCU). With anterior retraction of the humeral head of the FCU and careful posterior retraction of the ulnar nerve, the remnant of the UCL, distal surface of the medial epicondyle, and the medial cortex of the ulna, including the sublime tubercle, are exposed (Fig. 33.9). An additional benefit of the muscle-splitting technique is that it obviates transposition of the ulnar nerve. Obviously the surgeon must be aware of the course of the nerve and be careful to protect it from compression or direct damage during the procedure; however, the choice of transposition can be made by the surgeon based upon surgeon preference and preoperative symptoms. Current reports reflect differing opinions on transposition, as some authors routinely transpose the ulnar nerve, while others only do so in the setting of preoperative ulnar nerve complaints.11,17,25–29 When performed, most authors prefer subcutaneous transposition of the nerve via fascial slings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree