12. Sports injuries
Dr. Kristjan Oddsson
Introduction
Regular physical activity can improve health in numerous ways. Several scientific studies indicate that it may reduce the risk of developing many diseases. This chapter presents some of the scientifically proven positive effects of physical activity (US Department of Health and Human Services 1996). These include:
• Reduced risk of dying prematurely.
• Reduced risk of dying from heart disease.
• Reduced risk of developing diabetes.
• Reduced risk of developing high blood pressure.
• Reduction in blood pressure in people who already have high blood pressure.
• Reduced risk of developing colon cancer.
• Reduced feelings of depression and anxiety.
• Helps control weight.
• Helps build and maintain healthy bones, muscles, and joints.
• Helps older adults become stronger and better able to move about without falling.
• Promotes psychological wellbeing.
During the 1990s several recommendations were published indicating the importance of physical exercise, with suggested guidelines. These recommended that every US adult should accrue at least 30min of daily moderate physical activity (Pate et al. 1995). This has since evolved so that the current guidance is that healthy adults aged 18–65 need moderately intense aerobic physical activity, or a combination of moderate and intense exercise, for a minimum of 30min a day for five days a week (Haskell et al. 2007).
People aged over 65 are additionally considered to benefit from flexibility and balance exercises to reduce the risk of falling (Nelson et al. 2007). Research has also indicated substantial benefits from strength training for older people (Pollock, 1999 and Kryger, 2007).
Although the existing benefits of exercise are clear (Fig. 12.1), physical activity can also increase the risk of injury. Approximately seven million people a year are treated for injuries acquired from physical activity and/or sports, and 25% of the injured individuals are absent from work or school for at least one day due to the injury (Conn et al. 2003). Injuries are more frequent among younger individuals, and in men twice as often as in women. In the USA, some of the most frequent sports injuries are from contact sports like football, ice hockey, basketball, and soccer. Baseball and softball are sports with less frequent injuries (Hootman et al. 2007). In Europe, soccer and basketball are also among the most injury-frequented sports (Belechri et al. 2001).
It is important for the sports massage therapist to have basic knowledge of the most common sports injuries, their symptoms, and basic treatment protocols. A sports therapist is often asked questions by both coaches and athletes about how to avoid sports injuries and about basic rehabilitation advice.
Basically all tissues and musculoskeletal structures can be affected by sports injuries, i.e. bone, periosteum, joint cartilage, joint capsules, ligaments, menisci, discs, muscles, fasciae, tendons, bursae, blood vessels, and nerves. Properly executed physical exercise will increase the structural size and strength of all affected tissues; however, if the load exceeds the tissues’ ability to adapt, injuries and pain may arise. This is true for both the “weekend warrior,” who starts training at too high an intensity, and the elite athlete, who constantly trains at the upper level of what the body can handle.
During sports activity, the athlete’s body is exposed to extreme stress. For sports with explosive movements, for example certain track and field disciplines (sprints, jump, and throwing events) and team sports (football, soccer, basketball, volleyball), the force between the athlete and surface can reach 1800–2200lb. It is easy, therefore, to understand how different types of injury can arise during such circumstances, especially if the athlete’s body is exposed to loads like this on a regular basis.
Sports injuries generally fall into two major categories: acute injuries and overuse injuries.
Pain and inflammation
Pain is defined by the International Association for the Study of Pain (IASP) as “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (Merskey et al. 1994).
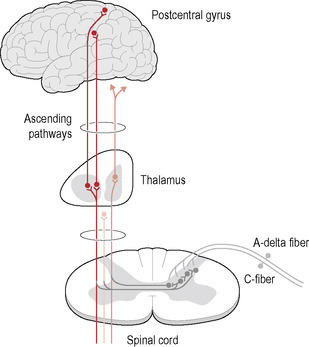
Pain receptors in the form of free nerve endings, i.e. nociceptors, exist in almost all forms of tissue but they are extra prevalent in the skin, periosteum, fasciae, ligaments, and tendon synovial sheaths. The nociceptors can be stimulated by chemicals (for example, potassium ions, histamine, prostaglandins) or by mechanical deformation. When activated, the receptors transmit signals through afferent myelinated Aδ-fibers (approx 30m/s) and even through unmyelinated C-fibers (approx 0.1–1m/s), to the dorsal horn in the spinal cord.
The most important pain pathway is the spinothalamic tract. The nerve impulses reach the postcentral gyrus in the parietal lobe via the thalamus in the brain. There are also more diffuse subcortical areas in the brain where pain sensations are interpreted more emotionally.
Pain anatomy
Figure 12.2 shows how the pain signal travels from the peripheral nociceptors, through Aδ- and C-fiber axons to the nerve roots, then to the spinal cord, from there to the brainstem, to the thalamus, and finally to the cortex, which leads to an awareness of pain.
 |
| Figure 12.2 |
Pain may be classified in the following categories (Woolf 2004):
• Nociceptive pain. Transient pain in response to a noxious stimulus.
• Inflammatory pain. Spontaneous pain and hypersensitivity to pain in response to tissue damage and inflammation.
• Neuropathic pain. Spontaneous pain and hypersensitivity to pain in association with damage to, or a lesion of, the nervous system.
• Functional pain. Hypersensitivity to pain resulting from abnormal central processing of normal input.
Pain is also divided into acute or chronic pain. Pain with a duration of more than three months is medically classified as chronic.
In sports injuries, one of the purposes of the inflammatory pain experience is to promote healing of the injured tissues. The pain reduces movement of and contact with the injured body part to assist the body’s healing efforts. There is generally an organic connection between an injury and the pain sensation. Most soft tissue injuries probably heal within 3–4 months. There are many theories about exactly why pain may be experienced long after the actual injury has healed. One theory is that pain receptors may acquire increased sensitivity during an injury due to chemical metabolites; another is that the brain misinterprets signals from “low-threshold” mechanoreceptors, creating pain sensations instead of positional information.
Microscopically, as tissues are injured, the inflammatory process commences with the release of chemicals from damaged cells. Mast cells release histamine, which promotes vasodilatation of small blood vessels. White blood cells and other phagocytes also participate in the “inflammatory battle.” The injured blood vessels, in conjunction with vasodilatation and increased capillary permeability, create an increased swelling in the area (Nisell et al. 1999).
Macroscopically, inflammation has five common signs:
• pain—dolor
• heat—calor
• redness—rubor
• swelling—tumor
• reduced function—functio laesa.
To reduce pain and inflammation, doctors or other healthcare providers sometimes recommend the patient takes nonsteroid antiinflammatory drugs (NSAIDs), such as aspirin, ibuprofen, ketoprofen, or naproxen sodium. For more severe pain, doctors may prescribe NSAIDs in prescription strengths. It should be noted, however, that the cause of pain and inflammation is never a deficiency of NSAIDs; instead the therapist must seek and treat the real cause of the ailment.
The body’s different tissue types react forcefully to the inflammatory processes; however, tendons seem not to react with inflammation during tissue damage except in the acute stage. Instead, injuries to tendons seem to tend to develop into chronic, sometimes degenerative, conditions, i.e. tendinosis and tendinopathies.
Principles of rehabilitation
Rehabilitation is an integral part of the treatment of both acute injuries and overload traumas. Besides creating freedom from pain, the intention is to restore ROM, strength, endurance, coordination, and function.
The pain experience and degree of tenderness when using the body part should guide the duration and intensity of the training. Movement training should commence with gentle isometric exercises, initially without any external load, and gradually increase in intensity. When normal ROM and strength are achieved, rehabilitation training is gradually transferred to concentric–eccentric training at a higher speed and with smaller loads: the athlete’s own body weight is often enough. Certain injuries, like chronic Achilles tendinitis, have been shown to respond well to heavier eccentric exercises.
Another specific type of strength training is isokinetic training, i.e. training with the same speed throughout the whole movement. This type of rehabilitation training is often used in postsurgical treatment of knee injuries, etc.
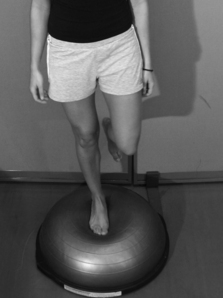
One very important part of rehabilitation training is balance and coordination exercises.
Balance boards
During rehabilitation of ligament and joint injuries, it is important to use different kinds of balance board to place stress on the proprioceptive system (Fig. 12.3). The body’s neuromuscular functions are also affected by tissue damage. A balance board, spring board, rope jumping, etc., help to assist the athlete’s proprioceptive system.
 |
 |
| Figure 12.3 |
Acute injuries
Acute injuries include:
• fractures
• dislocations/luxations
• muscle injuries
• ligament injuries
• acute tendon injuries
• acute bursa injuries.
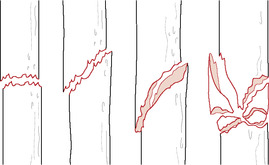
A sports injury can almost always be connected to a specific event, either internal or external violence to the body’s structures, for example muscle strain or contusions, or a sprained ankle in conjunction with training or competitive sports activity. A severe hematoma is commonly present, which leads to further unwanted effects (Fig. 12.4).
 |
| Figure 12.4 |
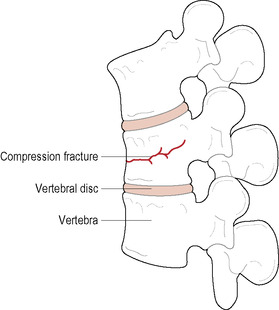
Fractures
Acute fractures are emergencies and should be examined and treated in hospital. Fractures can be simple (closed) or compound (open) (Figs 12.5; 12.6), and are commonly accompanied by soft tissue injuries. Contact sports have a higher incidence of bone fractures, and commonly affected areas are the fingers, clavicle, radius, and tibia.
 |
| Figure 12.5 |
 |
| Figure 12.6 |
The symptoms are pain, swelling, discoloration, and possibly misalignment. After a proper examination and diagnosis, the bone is either reduced or not, depending on the possible misalignment; more complex fractures may require surgical intervention. A cast or splint is often used for 3–12 weeks, depending on the location in the body, to immobilize the affected body part.
Avulsion—a complete tear of a ligament or tendon attachment—is more common among children and adolescents.
Fractures stemming from overload injuries, i.e. stress fractures, are described further in the section “Overuse injuries” below.
Dislocations (luxations)/subluxations
Dislocations are another emergency to be examined, diagnosed, and treated at hospital. They are often caused by external violence, for example a shoulder dislocation created by a fall with extended arms, and sometimes cause fractures in addition. Dislocations may also be caused by internal violence, for example when an arm is hooked and the athlete forces through the movement, thus causing damage.
The most frequent dislocations are of the shoulders and finger joints. More stable joints like the hip, elbow, and ankle require greater forces to dislocate them. Dislocations are commonly associated with soft tissue damage to muscles, ligaments, joint capsules, and occasionally nerves.
Muscle injuries
Muscle injuries can be caused by internal forces, in which case they are called muscle strains. Muscles spanning two or more joints, for example the hamstrings, are more frequently exposed to this type of muscle injury, which is common among track and field athletes in sprinting, jumping, or other events involving explosive muscle contractions. Muscle strains are often located at the musculotendinous junction and are thought to occur in the interplay between high-speed concentric and eccentric muscle contractions.
Muscle strains are classified as:
1. Grade I. Mild strain with damage to less than 5% of the muscle fibers, causing localized pain sensation without substantial strength impairment.
2. Grade II. Moderate strain, a substantially larger injury with notable pain during palpation and/or contraction attempt. A swelling is commonly noted.
3. Grade III. A complete tear of the muscle.
External forces may cause muscle injuries called muscle contusions, for example when one football player collides with another, and a knee crushes the quadriceps muscle toward the underlying femur, or through falling on a hard object. This type of muscle injury can potentially happen in any sport containing moments of contact, such as football, soccer, basketball, or ice hockey.
The symptoms of acute muscle injuries are commonly a sudden stabbing pain accompanied by difficulty contracting the injured muscle. Other symptoms are swelling, possible muscle cramping, and occasionally a palpable gap in the muscle tissue.
The bleeding caused by the injury can be either intermuscular or intramuscular. Intermuscular bleeding is localized between muscles due to a rupture of the muscle fascia. As the blood is spread over a larger area it causes a more visible hematoma, but it has a faster recovery time. An intramuscular hematoma remains within the muscle since the fascia is intact, and has a longer healing period since it is more difficult for the body to absorb the localized edema encapsulated within the muscle. It may additionally cause complications like severe scarring, impaired ROM and/or calcification or ossification of the scar tissue, i.e. myositis ossificans, which may require surgical intervention.
Muscle cramps may be defined as involuntary, often painful, muscle contractions. Their origin is still somewhat unclear, but Parisi et al. (2003) have divided muscle cramp into three categories, based on etiology:
1. paraphysiological cramps
2. idiopathic cramps
3. symptomatic cramps.
Muscle cramps relating to physical activity are categorized as paraphysiological cramps. It is suggested that this type arises from a hydroelectrolytic imbalance caused by hard, long-term, and sometimes repetitive activity leading to hyperexcitability of the terminal nerve branches in the area. Research has additionally indicated low magnesium levels (Klarkeson et al. 1995). Dehydration, glycogen depletion, salt deficiency, previous muscle bleeding, small muscle ruptures, or the athlete’s general health are other possible causes.
The athlete should prevent cramping by adequate basic training, including warm-up routine, and ensuring proper nutrition and fluid, electrolyte, and glycogen deposit uptake (Peterson et al. 2001).
The sports massage therapist can perform cramp release using stretching, cryo-, and physiotherapy, for example strong effleurage and deep friction massage (Brukner et al. 2010). Another popular and effective method involves simultaneous relaxation, approximation, and compression of the cramping muscle combined with alternating isometric contractions of antagonistic muscles (Fig. 12.7). The athlete is asked to contract the antagonistic muscle for 4–5s whilst the approximation/compression is maintained and further increased between every isometric muscle contraction.
 |
| Figure 12.7 |
Ligament injuries
A sprain is a stretch or a tear of a ligament, and commonly occurs in conjunction with acute violence toward the affected joint. Sprains are classified as:
1. Grade I. Mild injury involving microscopic tears and some tenderness.
2. Grade II. Moderate injury with partial ligament rupture, notable swelling, and tenderness.
3. Grade III. Serious injury with a complete tear of the ligament. Generates notable instability and intense pain.
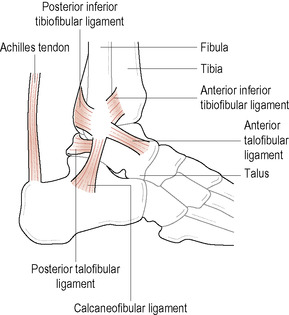
Since the symptoms of ligament sprains in different joints vary, it makes the classifications more difficult to use clinically. The possibilities for healing vary depending on whether the ligament is extracapsular (for example, the calcaneofibular ligament in the ankle), intracapsular (for example, the cruciate ligaments in the knee joint), or capsular (for example, the anterior talofibular ligament in the ankle) (Figs 12.8; 12.9). Intracapsular ligaments do not heal after a complete tear, while a capsular ligament can have better possibilities of doing so (Bahr et al. 2004).
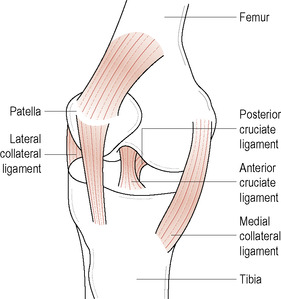 |
| Figure 12.9 Ligaments in the knee jointInjury to the anterior cruciate ligament is common and one of the most controversial and difficult to treat sports injuries |
Ligaments located in the ankle and knee joints are most frequently injured during sports activity. It is estimated that about 20 000 ankle sprains/day occur in the USA. Of these 70% occur in the anterior talofibular ligament. In the knee, there are 200 000 anterior cruciate ligament injuries/year, 100 000 requiring surgical intervention (American Association of Orthopedic Surgeons 2008).
Acute tendon injuries
Almost every acute spontaneous rupture of tendons is preceded by pathological changes in the tendon (Peterson et al. 2001). Tendon injuries are classified similarly to ligament injuries. Ruptures commonly present where the tendon’s blood supply is minimized, for example, for the Achilles tendon, almost 1in above the calcaneus. Many tendons that are exposed to injuries (for example, Achilles tendon, supraspinatus tendon, patellar ligament) may show degenerative changes as early as in the third decade (Maffulli et al. 2005).
Rupture of the calcaneus/Achilles tendon
The calcaneus/Achilles tendon is the strongest tendon in the body. The load during walking is estimated to be 2.5 times the body weight, and running may increase this up to 6–12 times (Komi, 1992 and Merskey, 1994). Men are more frequently exposed than women to complete ruptures of the calcaneus tendon (Fig. 12.10), which has an acute onset with sharp pain and impaired function. Thompson’s test (Simmond’s calf squeeze test) is positive as the foot fails to plantarflex as the calf muscle is squeezed (Brukner et al. 2001; Fig. 12.11).
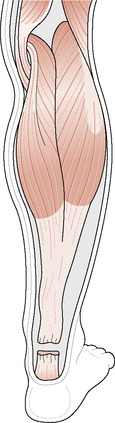 |
| Figure 12.10 |
 |
| Figure 12.11 Thompson’s test for total Achilles ruptureSqueezing the calf muscle will result in a small plantar flexion of the foot. If not, the test is positive |
Treatment of a complete rupture of the calcaneus tendon is either surgical or conservative (for example, cast treatment for 8–10 weeks). Even though the evidence is not yet fully conclusive, it seems that the risk of a new rupture is somewhat larger after conservative treatment. Despite the inherent risks of surgery, it is therefore the preferred treatment for athletes thanks to the possibility of early motion, which is essential for effective rehabilitation (Brukner, 2010 and Peterson, 2001).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree