Francis H. Shen
Spine
Regional Anatomy and Surgical Intervals
Regional Anatomy
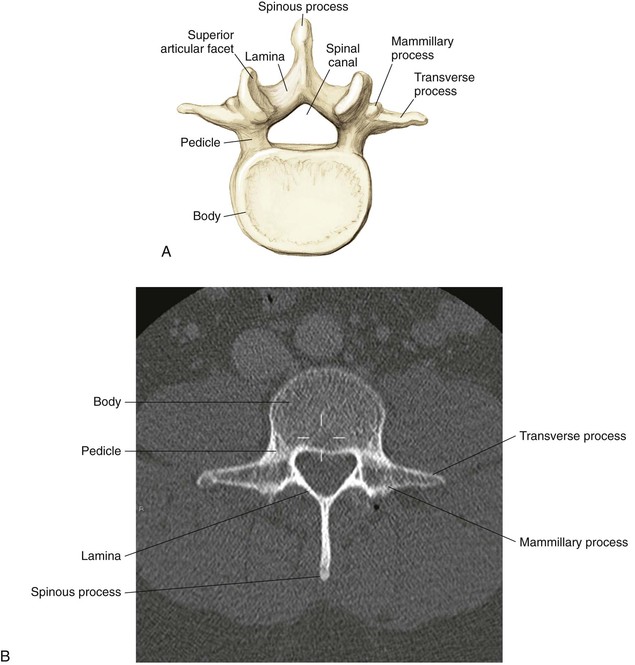
Osteology
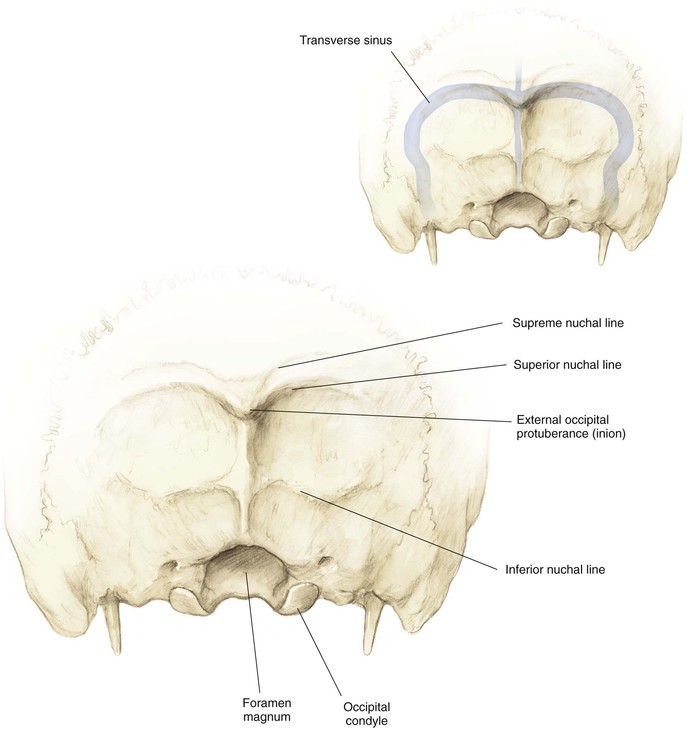
Occiput (Fig. 5-1)
External occipital protuberance (inion)
• Thickest portion of bone (4-18 mm)
Supreme, superior, and inferior nuchal lines
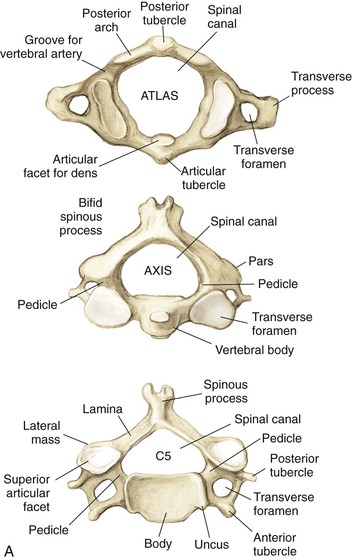
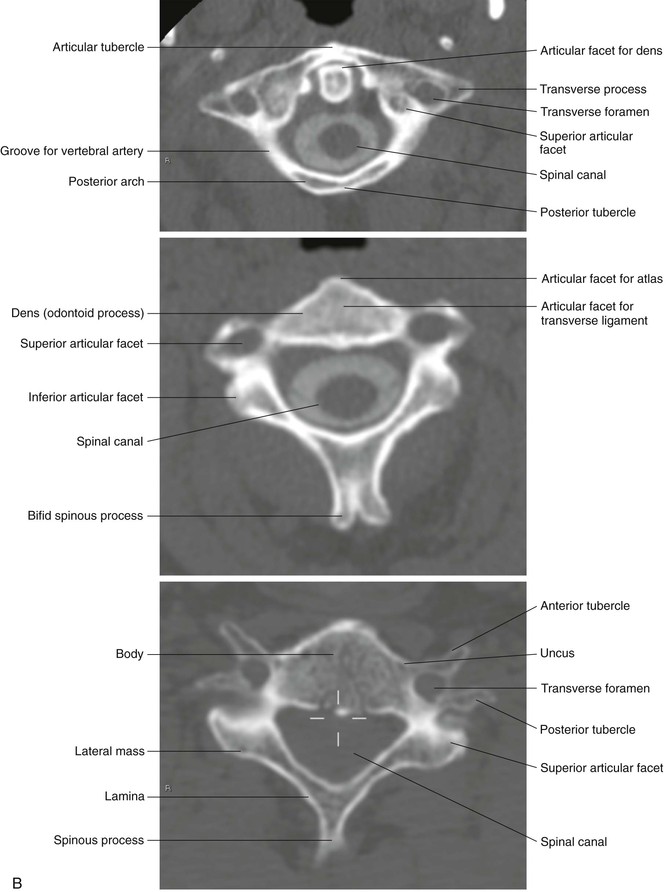
Cervical Vertebrae (Fig. 5-2)
• A ring that lacks a centrum and spinous process
• The groove for the vertebral artery sits posterior and superiorly
• Prominent bifid spinous process
• The superior articular facet lies anterior to the inferior facets
• Spinal canal triangular configuration
• The sagittal diameter varies from 17 to 18 mm (C3-C6) to 15 mm (C7)
• Lateral masses are thinnest at C6 and C7
• Anterior and posterior tubercle
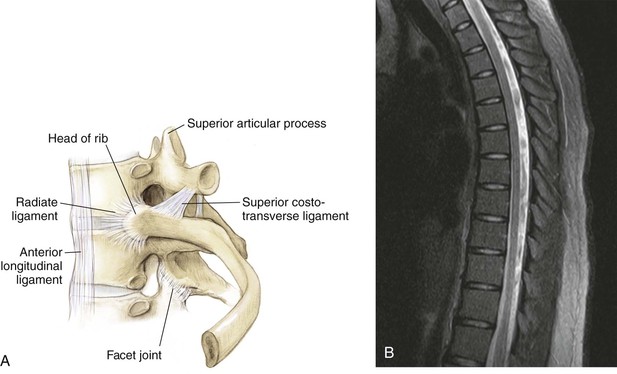
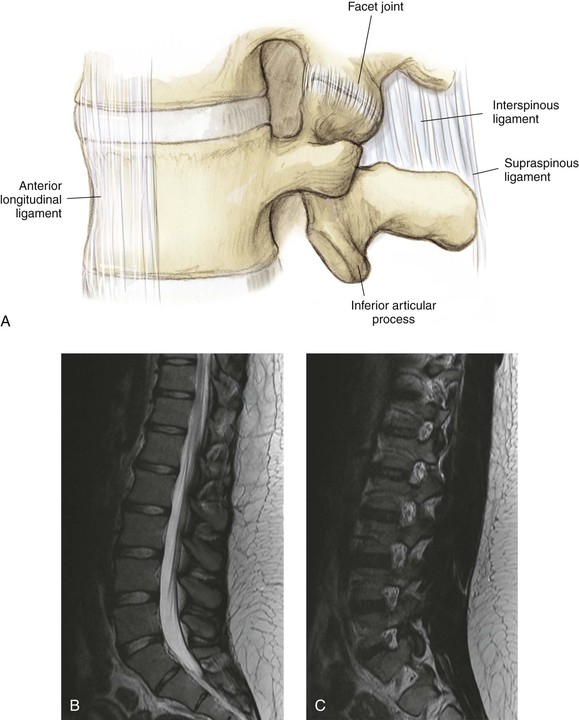
Arthrology
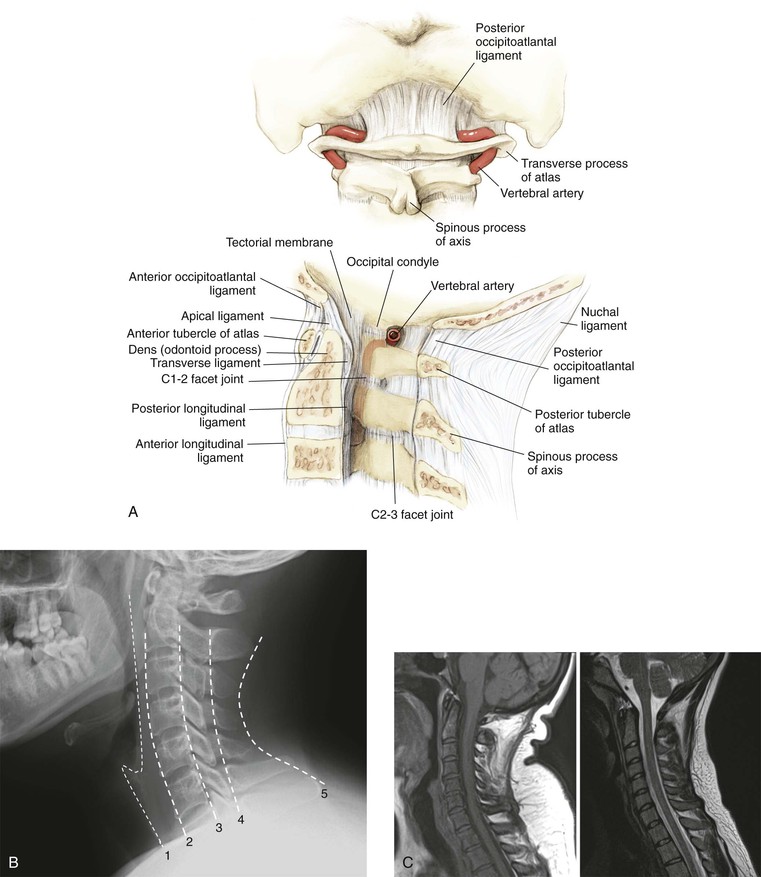
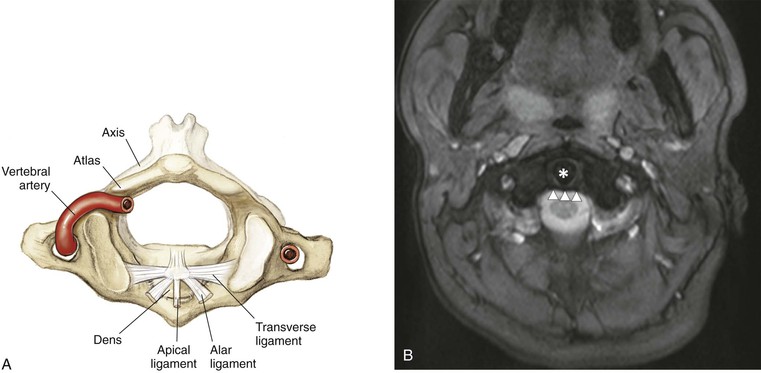
Cervical
• 50% of cervical flexion-extension
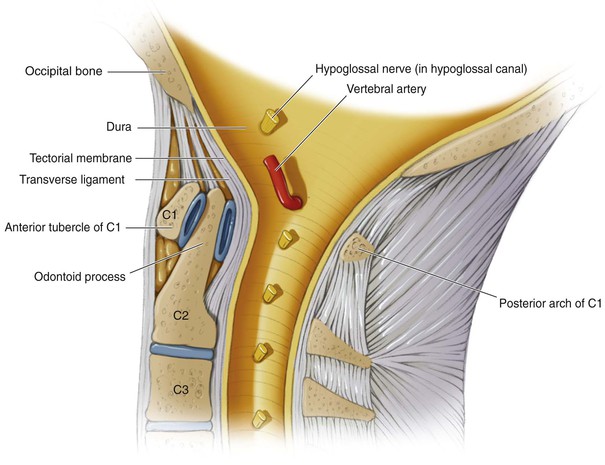
• Tectorial membrane (after the foramen magnum it becomes the posterior longitudinal ligament)
• Anterior longitudinal ligament (continues throughout the mobile spine)
• Posterior occipitoatlantal and anterior occipitoatlantal ligaments
• One apical and two alar ligaments
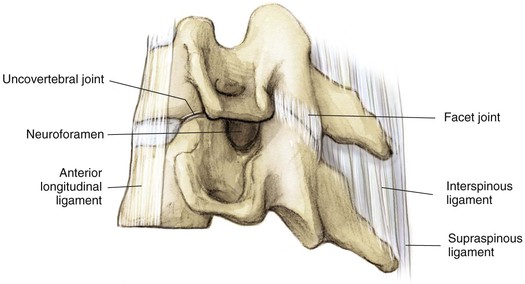
Uncovertebral joint (Fig. 5-7)
• Not a true diarthrodial joint
• Forms the anterior border of the neuroforamen
• Shingled with the superior articular facet anterior to the inferior articular facet
Nervous System
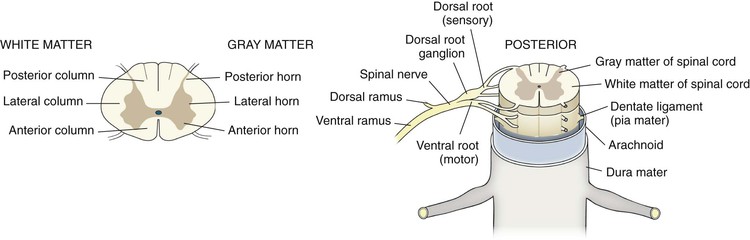
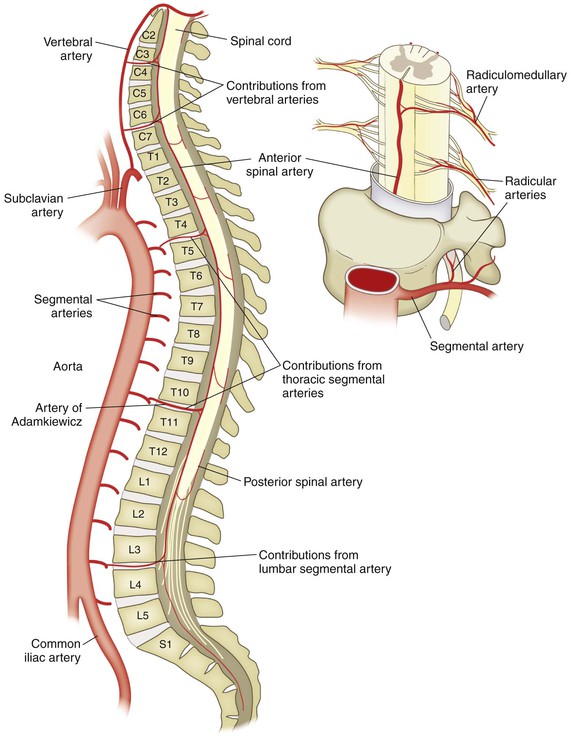
Spinal Cord (Fig. 5-15)
Continuation of the medulla as it exits the foramen magnum
Terminates as the conus medullaris at T12-L1 or L2-L3
Continues caudally as the cauda equina
The spinal cord diameter is largest at the C6 vertebra
Three meninges: dura (outermost covering), arachnoid, and pia mater (innermost covering)
Cerebrospinal fluid is found between the arachnoid and pia mater
White Matter
• Anterior spinothalamic tract
• Carries light/crude touch sensation
• Anterior corticospinal tract
• Delivers voluntary contraction
• Fasciculus cuneatus laterally
• Fasciculus gracilis medially
• Carries deep touch, proprioception, and vibratory sense
• Carries contralateral pain and temperature fibers
• Descending motor lateral corticospinal tract
Nerve Roots
• Formed by the convergence of the dorsal and ventral roots
• Delivers the dorsal primary rami
• Supplies skin and muscle to the neck and back
• Delivers the ventral primary rami
• Supplies the anteromedial trunk and limbs
• Brachial plexus in the cervical spine
• Lumbosacral plexus in the lumbar and sacral spine
Thirty-one paired spinal nerves
Surgical Intervals
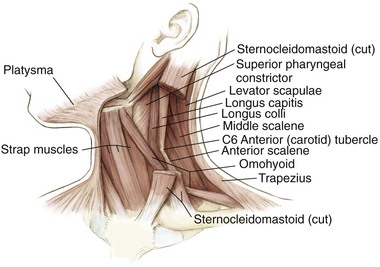
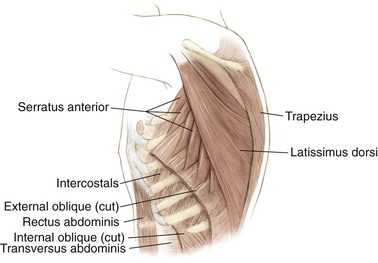
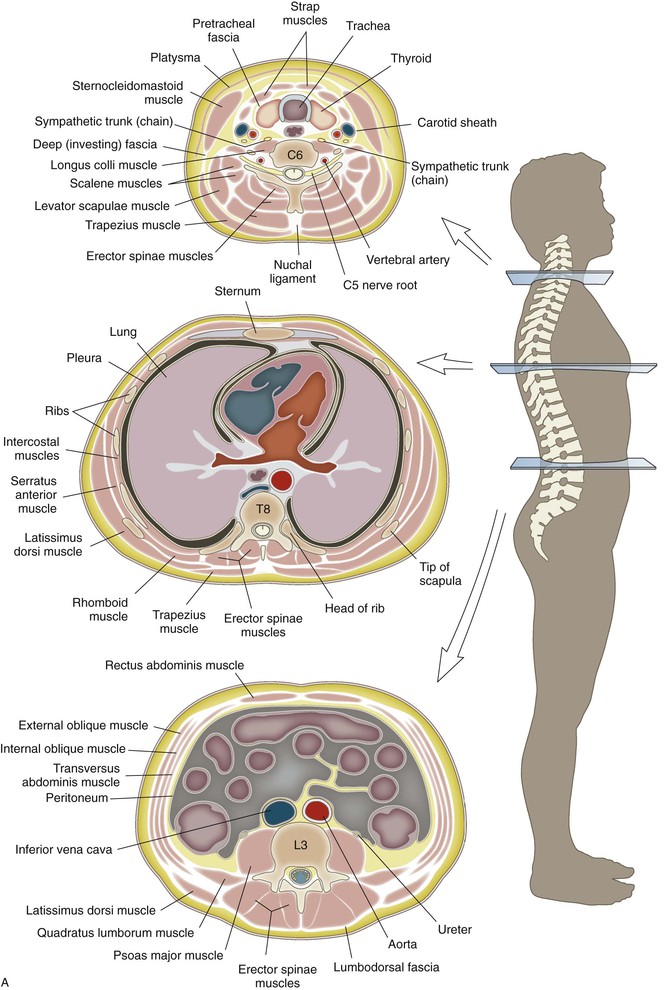
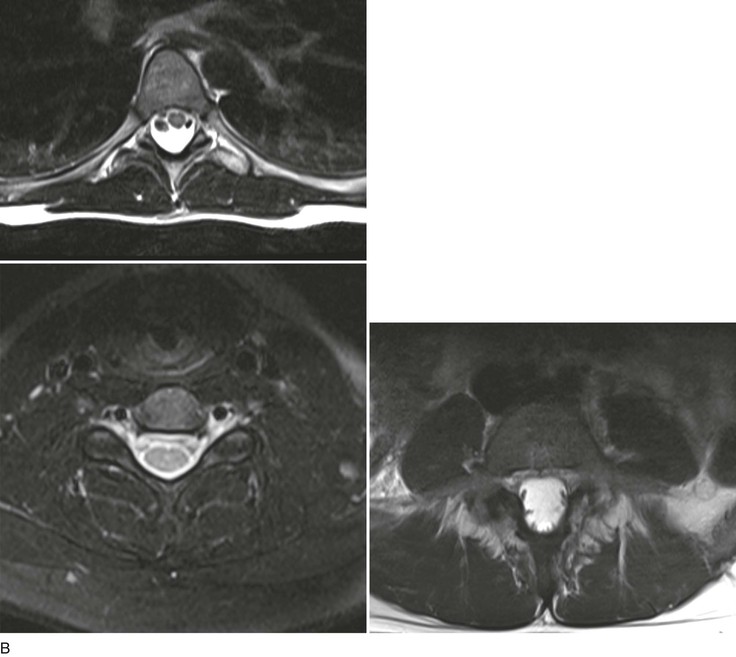
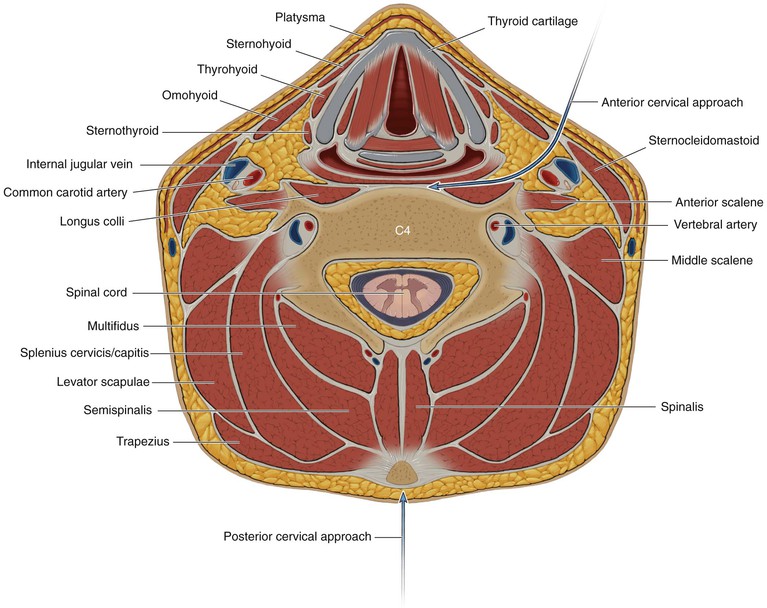
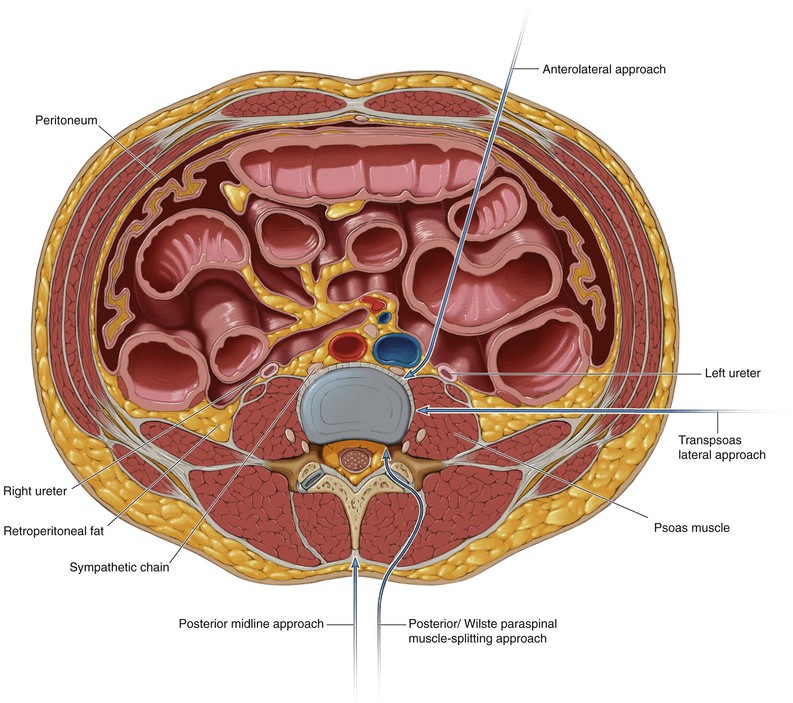
Unlike surgical approaches in the appendicular spine, surgical approaches for the spine traditionally utilize intermuscular planes; approaches for the cervical and lumbar spine are depicted in Figs. 5-16 and 5-17
• The anterior approach to the cervical spine utilizes an intermuscular plane as the safe interval (Fig. 5-16)
• Posterior midline incision (Fig. 5-16)
• Anterolateral approach to the lumbar spine (Fig. 5-17)
• Lateral/transpsoas approach to the lumbar spine (Fig. 5-17)
• Posterior/Wiltse paraspinal muscle-splitting approach to the lumbar spine (Fig. 5-17)
• Posterior midline approach to the lumbar spine (Fig. 5-17)
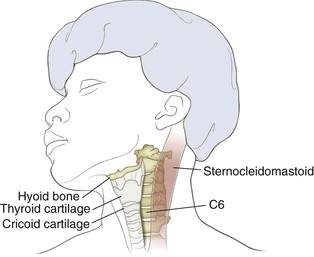
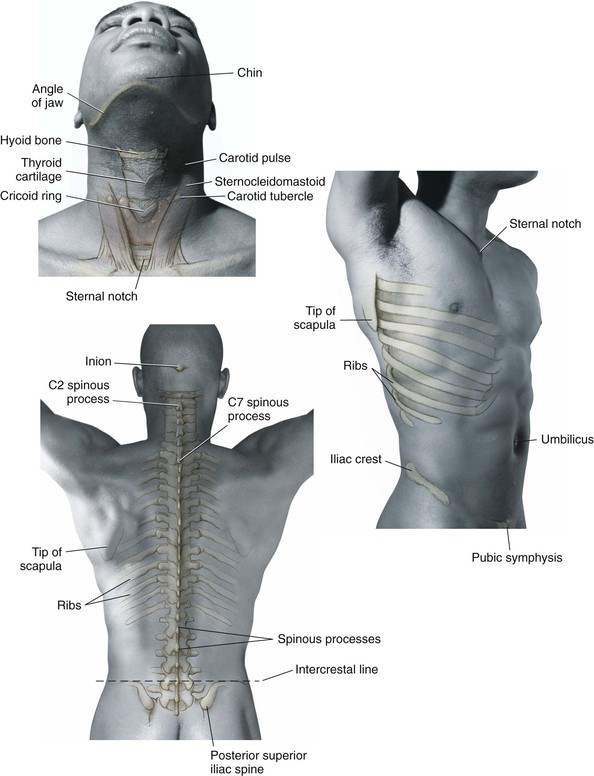
Landmarks (Fig. 5-20)
Cervical Spine
Anterior
Approaches to the Spine
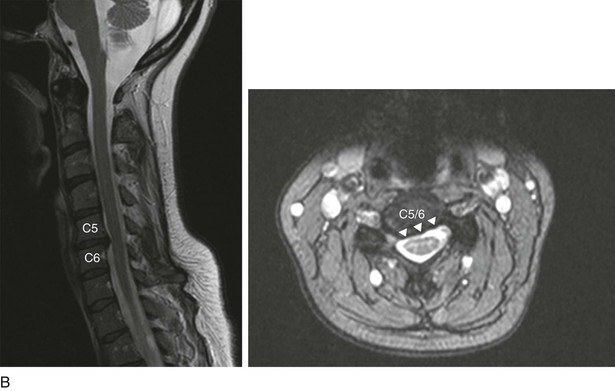
Anterior Approach to the Cervical Spine (Video 5-1)
Indications
Anterior Decompression of the Spinal Canal
Positioning
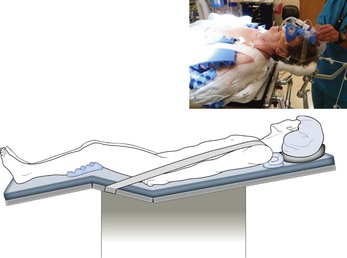
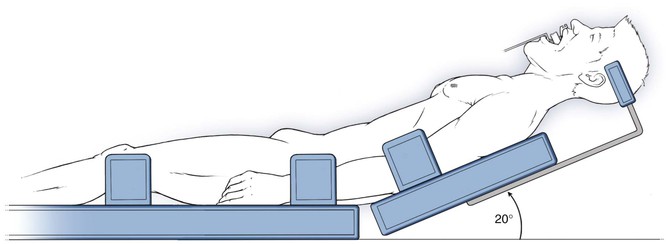
Supine (Fig. 5-21)
• Typically, the head is placed in a neutral alignment
• Extension and contralateral head rotation can help improve surgical exposure if necessary
• Care should be taken to ensure that the degree of extension necessary is possible before intubation
• Gentle taping of the shoulders inferiorly can improve intraoperative radiographs
• Neck extension can be facilitated by placement of a roll between the shoulder blades
• Gardner-Wells or Halter traction can be used if distraction is required
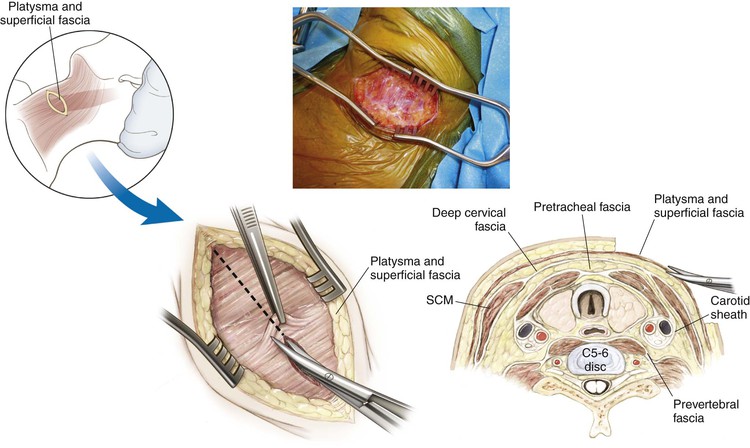
Superficial Dissection
Identify the platysma (Fig. 5-24)
• Divide the fibers of the platysma
• Alternatively, split the muscles of the platysma in line with fibers
• Elevate and mobilize the platysma superiorly and inferiorly as needed
Identify the anterior border of the sternocleidomastoid muscle (Fig. 5-25)
• Divide the fascia immediately anterior to the sternocleidomastoid muscle (deep cervical fascia)
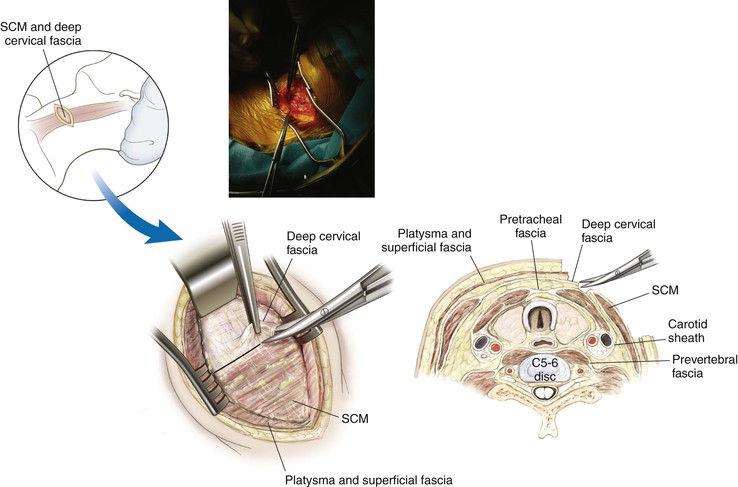
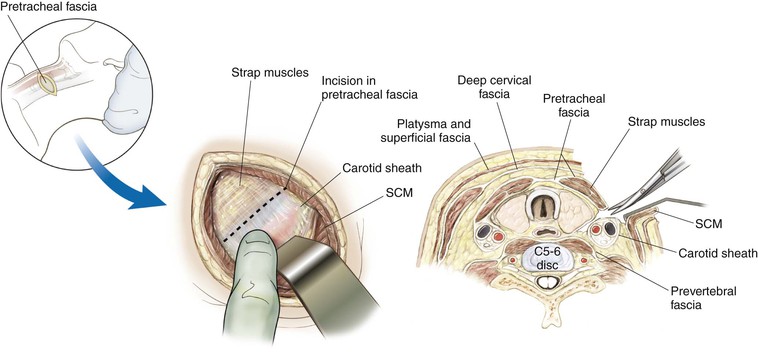
Palpate the pulse of the carotid artery (Fig. 5-26)
• Divide the fascia immediately anterior to the carotid sheath (pretracheal fascia)
Continue with blunt dissection to develop the plane down to the anterior surface of the cervical vertebra (Fig. 5-27)
• Two arteries may be seen crossing the field from the carotid sheath toward the midline structures
• One or both may have to be divided to increase surgical exposure
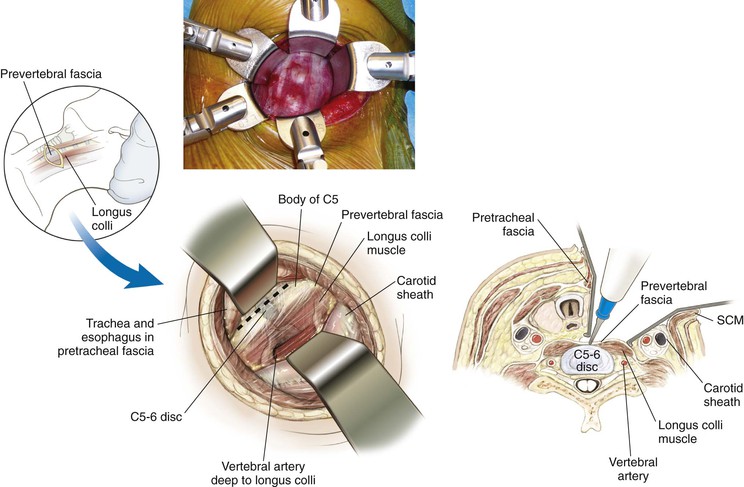
Deep Dissection
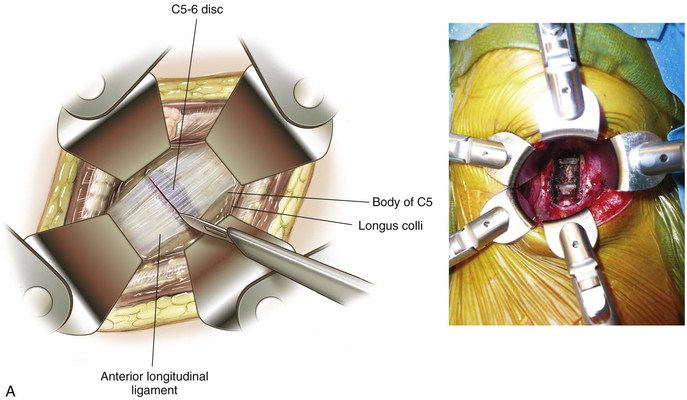
Deep dissection exposes the anterior cervical vertebra (Fig. 5-28)
• The longus colli muscles are now visible on either side
• The prevertebral fascia also can be seen covering the cervical vertebra
• The anterior longitudinal ligament can be seen as a gleaming white structure in the midline
• The sympathetic chain lies on the longus colli lateral to the vertebral bodies
Divide the prevertebral fascia
Detach and elevate the longus colli bilaterally for exposure
Transoral Approach
Indications
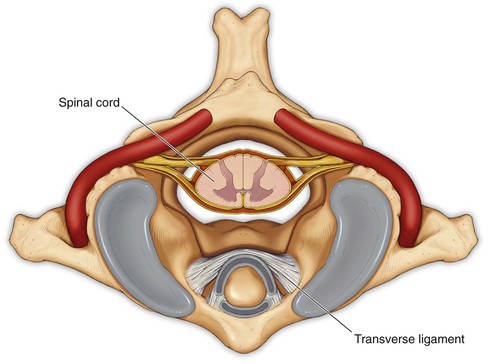
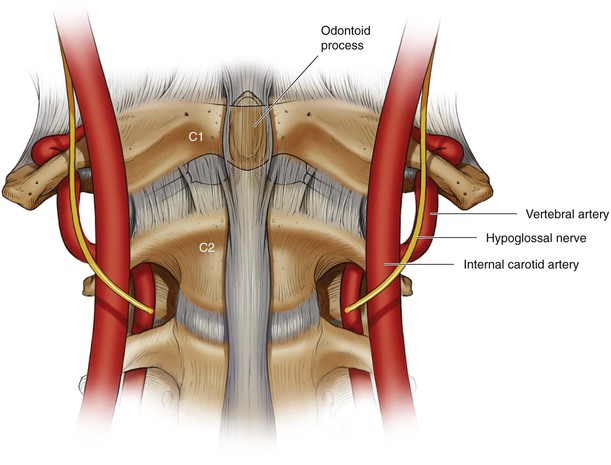
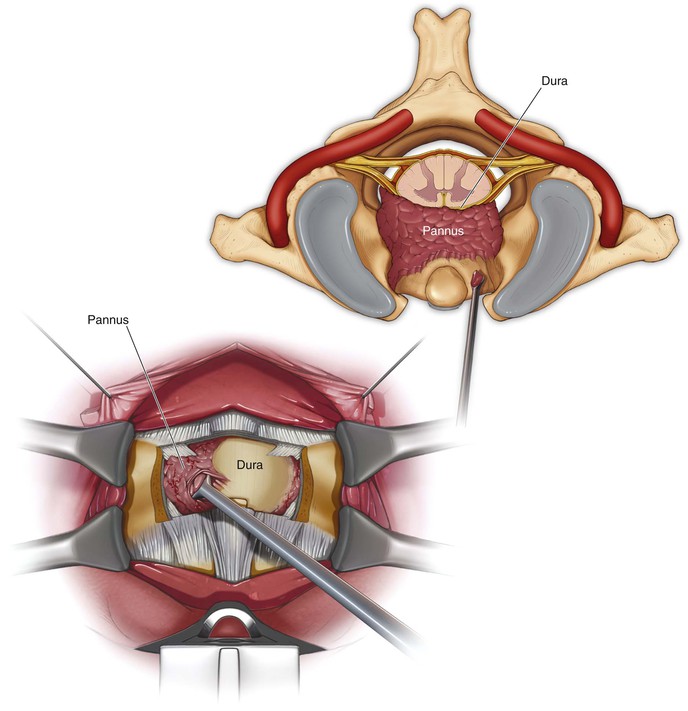
Hazards (Figs. 5-30 and 5-31)
Neural Structures
Vascular
• At risk with lateral exposure greater than 20 mm from midline at the level of C1
• At risk with lateral exposure greater than 10 mm from midline at the level of the C2-C3 disc space
Internal carotid artery (Fig. 5-32)
• Particularly at risk when dissection entails lateral exposure greater than 15 mm from midline
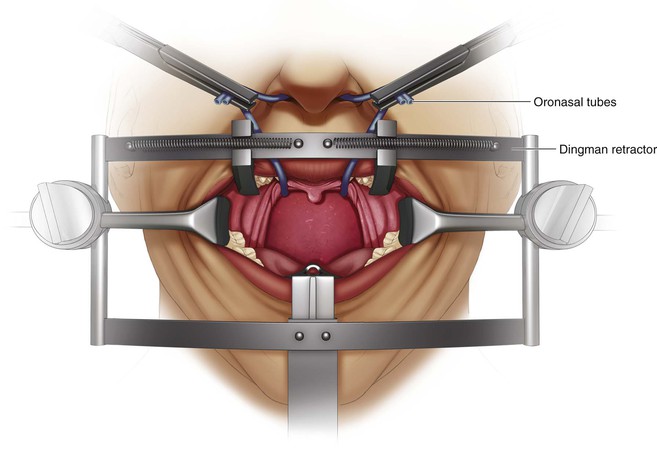
Intraoperative/Preincision Preparation
Pack the upper esophagus and trachea with sterile gauze
• Minimizes the ingestion of blood and other products
• Reduces the risk of aspiration
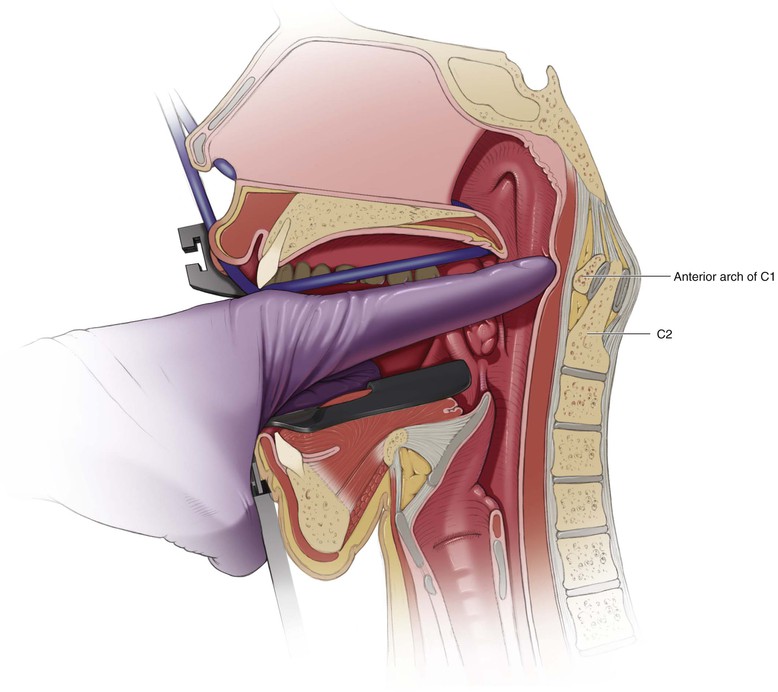
Careful retractor placement improves visualization of the interdental gap (Fig. 5-34)
• Elevate the soft and hard palate
• A tongue blade retractor can be used
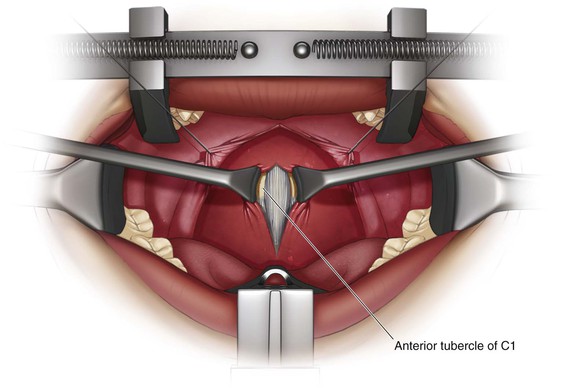
Palpate the anterior tubercle of C1 in midline (Fig. 5-35)
• Confirm the location radiographically
Incision
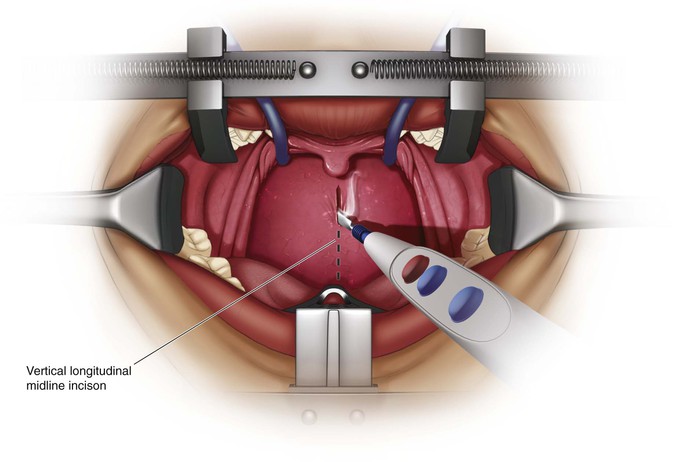
A 1- to 2-cm vertical longitudinal midline incision (Fig. 5-36)
• Just proximal to the anterior C1 tubercle down onto the body of C2 distally
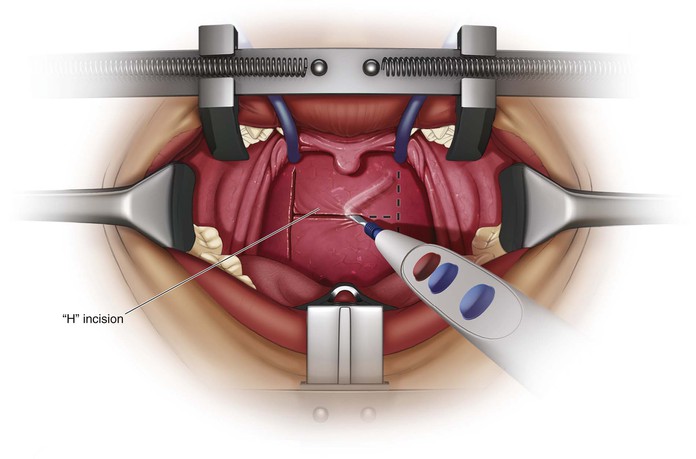
Make an “H” incision (Fig. 5-37)
• Vertical limbs are placed as far lateral as possible
• Injury to the eustachian tubes can occur if the vertical limbs are too lateral
• Allows for two broad-based pharyngeal myomucosal flaps that are elevated superiorly and inferiorly
• The horizontal limb is based on the level of the soft palate
Superficial Dissection
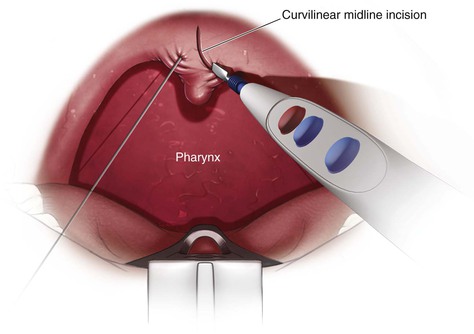
Retract the Soft Palate (Fig. 5-38)
Simple retractor placement may be sufficient
The uvula may be sutured and retracted proximally
Divide the soft palate lateral to the uvula if necessary
Exposure of the Anterior Ring of C1 (Fig. 5-39)
Full-thickness subperiosteal dissection
• Divide the mucosa and pharyngeal musculature as one flap; four layers:
• Superior constrictor muscle of the pharynx
• Anterior longitudinal ligament
• Attached to the anterior tubercle of C1
• May need to be sharply dissected free to maintain subperiosteal exposure
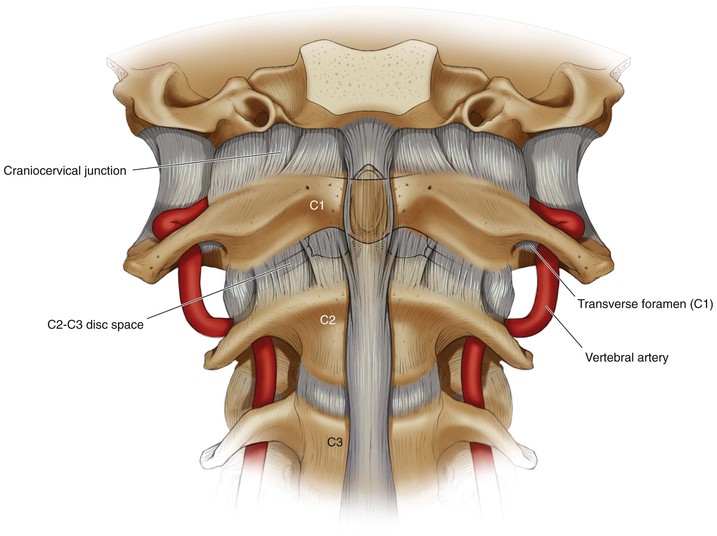
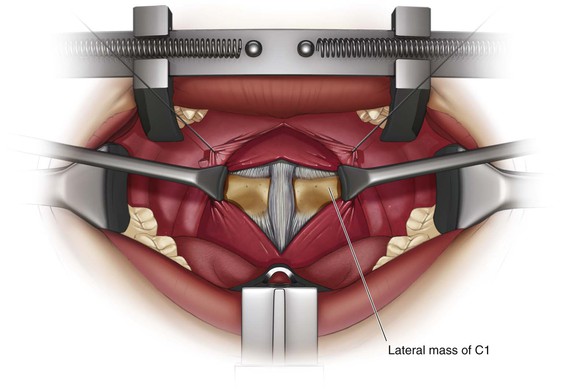
Exposure of the Lateral Mass of C1 (Fig. 5-40)
Elevate the longus colli muscles
Dissection laterally onto the midportion of the lateral mass of C1 bilaterally
• Maintaining midline orientation is imperative
• The anterior tubercle is an important landmark
• The midline can be distorted in patients with atlantoaxial rotatory subluxation
• Atlantoaxial rotatory subluxation can bring the vertebral arteries to the midline
Deep Dissection
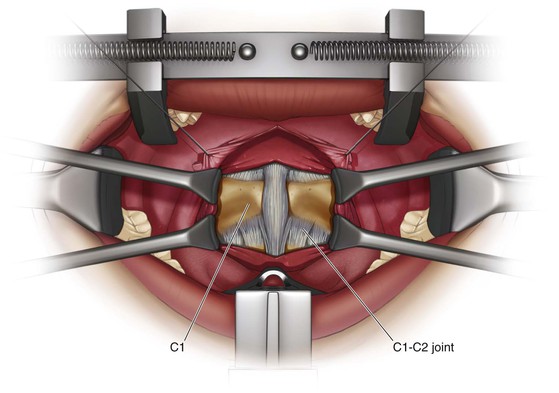
Exposure of C2
Exposure of the odontoid process of C2 (Fig. 5-42)
• Remove the central 1.0 to 1.5 cm of the anterior tubercle of C1
• Perform with a burr, pituitary rongeur, and/or curettes
• Maintaining midline orientation is imperative
• The anterior tubercle is an important landmark
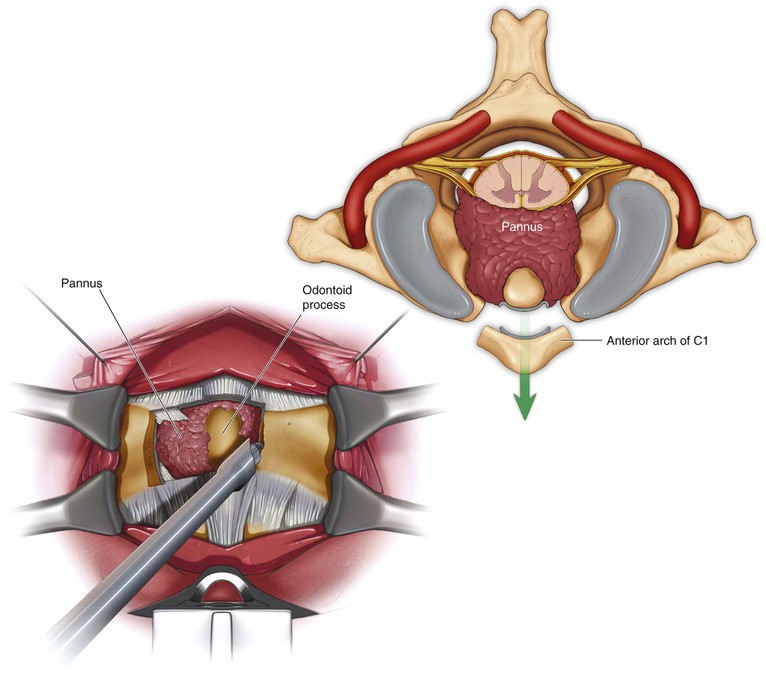
Removal of the Odontoid Process (Fig. 5-43)
• Perform with a burr, pituitary rongeur, and/or curettes
• Resect the odontoid at its base
• Bleeding may arise from the venous plexus just lateral to the base of the odontoid
• The tip of the odontoid process can be gently pulled down into the field from the foramen magnum
• Divide the apical and alar ligaments from the tip of the dens
• Care should be taken when using this technique
• Traumatic avulsion of the apical/alar ligament can result in dural leaks
Closure
Confirm that no CSF leak has occurred
• Use the intraoperative Valsalva maneuver
• Persistent leaks may require a lumbar drain
If possible, reapproximate the longus colli in the midline
Approximate the pharyngeal layer with resorbable suture
If a “H”-type incision was used, close the horizontal limb first, followed by the vertical limb
Approximate the soft palate in layers with absorbable suture
Anterior Transthoracic Approach to the Thoracic Spine (Video 5-2)
Indications
Anterior Spinal Cord Decompression
Positioning
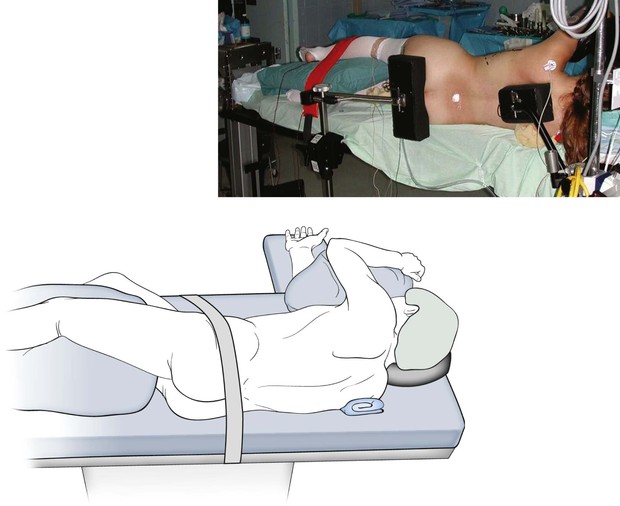
Lateral decubitus position with the side to be approached oriented up (Fig. 5-44)
• For deformity, the convexity of the curve is typically oriented up
• For decompressions, the side with the greatest stenosis to be addressed is typically oriented up
Secure the patient firmly to the operating table
• Stabilize the patient with either beanbags or hip positioners
• Carefully note the orientation of the spine before draping
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree