Athletic competition has long been a known source of spinal injuries. Approximately 8.7% of all new cases of spinal cord injuries in the United States are related to sports activities. The sports activities that have the highest risk of catastrophic spinal injuries are football, ice hockey, wrestling, diving, skiing, snowboarding, rugby, and cheerleading. Axial compression forces to the top of the head can lead to cervical fracture and quadriplegia in any sport. It is critical for any medical personnel responsible for athletes in team sports to have a plan for stabilization and transfer of an athlete who sustains a cervical spine injury.
Athletic competition has been an established cause of spinal injuries for centuries. Approximately 8.7% of all new cases of spinal cord injuries in the United States are related to sports. Athletic injuries are third only to motor vehicle accidents and violence as the most common cause of spinal cord injury in people aged 30 years or younger. A 3-year nationwide survey of all sports in Japan revealed a spinal injury incidence of 1.95 per million per year, with a mean age at injury of 28.5 years, and with 88% occurring in males. Catastrophic spinal cord injuries are much more likely to result from a cervical spinal injury than thoracic or lumbar trauma. Historically, sports at greatest risk for catastrophic spinal injuries have been football, ice hockey, wrestling, diving, skiing, snowboarding, rugby, cheerleading, and baseball.
The most common spine injuries in athletics can be carefully managed with nonoperative treatment. More serious spinal injuries, however, may lead to death, permanent disability, and extreme morbidity. The most common mechanism for injury leading to quadriplegia is an axial compressive force applied to the top of the head while the neck is slightly flexed, leading to loss of the protective cervical lordosis and alignment of the cervical vertebra. Information on catastrophic injuries in sports has been recorded by the National Center for Catastrophic Sports Injury Research (NCCSIR), the National Spinal Cord Injury Statistical Center, the United States Consumer Product Safety Commission (CPSC), and other organizations ( Table 1 ). The NCCSIR defines a catastrophic sports injury as any severe spinal, spinal cord, or cerebral injury incurred during participation in any school- or college-sponsored sport. These injuries are further subclassified into direct and indirect, and serious, nonfatal, and fatal for epidemiologic purposes.
| American Association of Cheerleading Coaches and Advisors (AACCA) | www.aacca.org |
| Consumer Product Safety Commission (CPSC) | www.cpsc.gov |
| The National Collegiate Athletic Association (NCAA) | www.ncaa.org |
| National Catastrophic Center Sports Injury Research (NCCSIR) | www.unc.edu/dept/nccsi/ |
| National Spinal Cord Injury Statistical Center (NCDDR) | www.ncddr.org |
| National Center of Injury Prevention and Control (NCIPC), Centers for Disease Control and Prevention (CDC) | www.cdc.gov/ncipc |
| National Federation of State High School Associations (NFHS) | www.nfhs.org |
| National Operating Committee on Standards for Athletic Equipment (NOCSAE) | www.nocsae.org |
| National Spinal Cord Injury Statistics Center (NSCISC) | www.spinalcord.uab.edu |
| USA Baseball | www.usabaseball.com |
In this article, the authors discuss common spinal injuries in the athletic population, typical mechanisms of injury, sport-specific catastrophic injuries and potential preventive measures in these at-risk sports.
Common spine injuries
Common athletic injuries to the spine include strains, muscle spasms, compression fractures, avulsion fractures, and disc herniations, with strains being the most common. Strains can be caused by any low-grade force to the spine, including the sudden extension-flexion mechanism associated with whiplash injuries. These athletes typically present with paravertebral muscle spasm, limited range of motion, and a normal neurologic examination. The loss of normal cervical lordosis or thoracic kyphosis may be seen on plain radiographs. Treatment involves conservative management with relative rest, anti-inflammatories (NSAIDs), muscle relaxants, and physical therapy.
Although compression fractures can occur anywhere along the course of the vertebral column, cervical spine compression fractures typically occur at the lower levels of C4 to C7. Radiologic evaluation with anterior-posterior, lateral, and flexion-extension radiographs are helpful in excluding serious injuries. Occasionally, when radiolographic negative evaluations are negative, CT or MRI may be necessary to further characterize an injury when the clinician has a high suspicion for cervical injury. Isolated compression fractures with less than 25% anterior compression can be conservatively managed with a cervical orthosis. Compression fractures with greater than 50% anterior compression are frequently associated with posterior ligamentous disruption, are usually unstable, and may require surgical fixation. A CT scan is helpful in evaluating fractures of the posterior vertebra and the vertebral elements that, if injured, may compromise spinal stability.
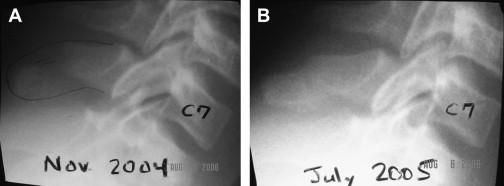
Cervical spinous process avulsion injuries, known as clay shoveler’s fractures, usually occur in football players and power lifters at the C7 level ( Fig. 1 ). The most widely accepted theory for the mechanism of injury in clay shoveler’s fracture is a forceful flexion of the cervical spine, or forceful contraction of the trapezius and rhomboid muscles. These avulsion fractures are quite stable and can usually be treated with cervical orthosis and other symptomatic measures such as pain medications and ice.
Return-to-play decisions for these fractures are usually straight forward. Patients who have a stable, healed compression or spinous process avulsion fracture, full, painless range of motion, and no neurologic deficits may return to contact sports participation.
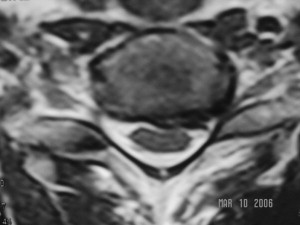
Disc herniation may occur in many sports ( Fig. 2 ). Typical symptoms and physical examination findings include pain, restricted range of motion, radicular symptoms, and sensory and motor deficits. A thorough neurologic examination can localize the level of the herniation, but an MRI will confirm the diagnosis and further characterize the extent of disc herniation. Athletes who have a herniated disc frequently respond to conservative, nonoperative modalities such as relative rest, NSAIDS, steroid dose pack, physical therapy, or epidural steroid injections. Only after these conservative measures fail, or if the athlete has a progressive neurologic deficit, is surgical decompression indicated. An anterior cervical discectomy with instrumented fusion is the surgical standard of care for most cervical disc herniations. Far lateral cervical disc herniations usually require a minimally invasive posterior foraminotomy to decompress the nerve root. Rarely, athletes may develop transient quadriplegia or long-tract findings from large central disc herniations. In these cases, urgent surgical management with anterior cervical discectomy and interbody vertebral fusion is recommended.
Catastrophic cervical spine injuries
Catastrophic cervical spine injuries include unstable fractures or dislocations, cervical cord neuropraxia (CCN or transient quadriplegia), and intervertebral disc herniations. The most frequent causes of catastrophic cervical spine injury, unstable fractures and dislocations, often result in permanent neurologic sequalae and usually occur in the lower cervical spine. In the lower cervical spine, the spinal cord occupies close to 75% of the canal’s cross-sectional area as compared with less than half at the level of the atlas.
Cervical injuries resulting in quadriplegia typically occur following application of an axial force to the top of the head while the neck is slightly flexed. The neutrally positioned neck has a protective lordotic curve, and most of the energy is dissipated by the paravertebral muscles and the intervertebral discs during an impact. When the neck is forward flexed about 30°, the cervical spine straightens, allowing the forces to be transmitted to the aligned cervical column. Once maximum compressive forces are reached, the spine fails. This occurs in either a flexion (flexion teardrop) or pure compression (burst fracture) mode with a resultant fracture, dislocation, or subluxation. This injury sequence may cause vertebral fragments or the intervertebral disc to retropulse into the spinal canal causing spinal cord damage.
CCN is an acute, usually transient neurologic injury, associated with sensory changes and possible weakness or paralysis in at least two extremities. Despite these findings, the cervical spine bony elements are usually uninjured and the patient is pain-free at the time of injury, with full range of motion. CCN is classified based on the neurologic deficit, duration of neurologic symptoms, and the pattern of injury. Injury grading is based on the duration of symptoms: Grade I, less than 15 minutes; Grade II, 15 minutes to 24 hours; and Grade III, longer than 24 hours. The pattern of injury is classified as quadriplegia, upper only, lower only, or hemiplegia. A prevalence of seven per 10,000 football participants has been previously estimated. Symptoms typically resolve within 10 to 15 minutes. Cervical stenosis is theorized to be the primary predisposing factor to CCN. Previously, the postulated mechanism of injury was either a hyperflexion or hyperextension of the neck causing a pincer-type spinal cord compression injury; however, new data have revealed that no one position particularly predisposes to CCN, and that various mechanisms, including axial forces, can be causative.
An episode of CCN is not an absolute contraindication to return to contact sports. It is unlikely that athletes who have had previous CCN injuries are at increased risk for permanent quadriplegia with further contact activities. Rather, poor technique using the top of the head for tackling is the primary risk factor for quadriplegia. Currently, there are no reports of any previously CCN-injured athlete sustaining a quadriplegic event after returning to contact sports; however, because the number of athletes returning to play after a CCN injury is low, no definitive conclusions can be made. Although complete resolution of symptoms is the rule with CCN, mild permanent neurologic deficits have been rarely reported.
Athletes who sustain a CCN injury need to be counseled on the known and potential risks of injury with return to contact sports. Specifically, there is a 50% overall risk of a recurrent CCN episode with return to football, which varies individually based on the canal diameter size—the smaller the canal diameter, the greater the risk of recurrence. Athletes who have any ligamentous instability, neurologic symptoms lasting longer than 36 hours, recurrent episodes, or MRI evidence of cord defect, cord edema, or minimal functional reserve should be excluded from return to contact sports.
Catastrophic cervical spine injuries
Catastrophic cervical spine injuries include unstable fractures or dislocations, cervical cord neuropraxia (CCN or transient quadriplegia), and intervertebral disc herniations. The most frequent causes of catastrophic cervical spine injury, unstable fractures and dislocations, often result in permanent neurologic sequalae and usually occur in the lower cervical spine. In the lower cervical spine, the spinal cord occupies close to 75% of the canal’s cross-sectional area as compared with less than half at the level of the atlas.
Cervical injuries resulting in quadriplegia typically occur following application of an axial force to the top of the head while the neck is slightly flexed. The neutrally positioned neck has a protective lordotic curve, and most of the energy is dissipated by the paravertebral muscles and the intervertebral discs during an impact. When the neck is forward flexed about 30°, the cervical spine straightens, allowing the forces to be transmitted to the aligned cervical column. Once maximum compressive forces are reached, the spine fails. This occurs in either a flexion (flexion teardrop) or pure compression (burst fracture) mode with a resultant fracture, dislocation, or subluxation. This injury sequence may cause vertebral fragments or the intervertebral disc to retropulse into the spinal canal causing spinal cord damage.
CCN is an acute, usually transient neurologic injury, associated with sensory changes and possible weakness or paralysis in at least two extremities. Despite these findings, the cervical spine bony elements are usually uninjured and the patient is pain-free at the time of injury, with full range of motion. CCN is classified based on the neurologic deficit, duration of neurologic symptoms, and the pattern of injury. Injury grading is based on the duration of symptoms: Grade I, less than 15 minutes; Grade II, 15 minutes to 24 hours; and Grade III, longer than 24 hours. The pattern of injury is classified as quadriplegia, upper only, lower only, or hemiplegia. A prevalence of seven per 10,000 football participants has been previously estimated. Symptoms typically resolve within 10 to 15 minutes. Cervical stenosis is theorized to be the primary predisposing factor to CCN. Previously, the postulated mechanism of injury was either a hyperflexion or hyperextension of the neck causing a pincer-type spinal cord compression injury; however, new data have revealed that no one position particularly predisposes to CCN, and that various mechanisms, including axial forces, can be causative.
An episode of CCN is not an absolute contraindication to return to contact sports. It is unlikely that athletes who have had previous CCN injuries are at increased risk for permanent quadriplegia with further contact activities. Rather, poor technique using the top of the head for tackling is the primary risk factor for quadriplegia. Currently, there are no reports of any previously CCN-injured athlete sustaining a quadriplegic event after returning to contact sports; however, because the number of athletes returning to play after a CCN injury is low, no definitive conclusions can be made. Although complete resolution of symptoms is the rule with CCN, mild permanent neurologic deficits have been rarely reported.
Athletes who sustain a CCN injury need to be counseled on the known and potential risks of injury with return to contact sports. Specifically, there is a 50% overall risk of a recurrent CCN episode with return to football, which varies individually based on the canal diameter size—the smaller the canal diameter, the greater the risk of recurrence. Athletes who have any ligamentous instability, neurologic symptoms lasting longer than 36 hours, recurrent episodes, or MRI evidence of cord defect, cord edema, or minimal functional reserve should be excluded from return to contact sports.
Screening
Currently only athletes who have a previous history of CCN should undergo screening for spinal cord stenosis. Radiation risk and cost make screening all athletes prohibitive. During the pre-participation physical examination (PPEs) providers should screen all athletes for any previous history of neck injury because this may obviate further questioning and screening. The Pavlov-Torg ratio for assessing cervical spinal stenosis involves measuring the cervical canal diameter and dividing it by the anteroposterior width of the vertebral body. A ratio of less than 0.8 potentially indicates significant cervical stenosis; however, this is a poor screening tool, because many football players have normal canal dimensions but large vertebral bodies, artificially decreasing this ratio below 0.8. A functional spinal stenosis may be a more accurate way of looking for athletes at risk of CCN. This is seen when there is a loss of the normal amount of cerebrospinal fluid around the spinal cord on MRI or CT myelography.
Sport-specific considerations for catastrophic spine injuries
Football
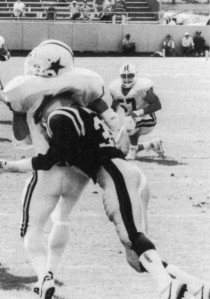
Because of large participation numbers and a high incidence of catastrophic injuries, football is associated with the highest number of severe cervical injuries per year for any high school or collegiate sport. Though head-related fatalities declined in the early 1970s as a result of better protective helmets, the number of cervical quadriplegia cases increased, likely because tacklers began hitting opponents using the crown of the head because of decreased fear of head injury. Torg and colleagues were instrumental in reducing the rate of quadriplegia as a result of cervical injury once they demonstrated that spearing, or tackling another player using the top of the head, was the major cause of permanent cervical quadriplegia ( Fig. 3 ). Spear tackling injuries typically occur to defensive players, especially defensive backs, as they attempt to tackle an offensive player. Special team players are especially susceptible because the speed at the time of collision is extremely high. After intentional spearing was banned in 1976, the rate of catastrophic cervical injuries dropped 80% from 1976 to 1987. This decline continued, and the incidence of quadriplegic injuries at the high school and college levels remained stable in the 1990s and early 2000s at 0.52 per 100,000 participants per year. In a recent review of over 500,000 high school football injuries of the 2005–2006 season, 4.1% of all injuries involved the neck or cervical spine, further defining this at-risk population.