The relationship of sleep to post-exercise recovery (PER) and athletic performance is a topic of great interest because of the growing body of scientific evidence confirming a link between critical sleep factors, cognitive processes, and metabolic function. Sleep restriction (sleep deprivation), sleep disturbance (poor sleep quality), and circadian rhythm disturbance (jet lag) are the key sleep factors that affect the overall restorative quality of the sleep state. This article discusses these theoretic concepts, presents relevant clinical cases, and reviews pilot data exploring the prevalence of sleep disturbance in two groups of high-performance athletes.
The relationship between sleep and post-exercise recovery (PER) and performance in elite athletes has become a topic of great interest because of the growing body of scientific evidence confirming a link between critical sleep factors, cognitive processes, and metabolic function. Although a complete understanding of the function of sleep in humans remains unknown and contested on many fronts, certain indisputable facts remain: sleep restriction (sleep deprivation) is linked causally to cognitive impairment; there is interindividual variability in the response to sleep deprivation with respect to the degree of cognitive impairment; and critical metabolic, immunologic and restorative physiologic processes are negatively affected by sleep restriction, sleep disturbance, and forced desynchrony of the human circadian sleep/wake phase.
Sleep has been identified by elite athletes, coaches, and trainers as an important aspect of the PER process, and is thought to be critical for optimal performance, even though there is little scientific evidence supporting this observation. The first comprehensive review of sleep and sport concluded that
- 1)
Little is known about the relationship between sleep to PER and performance in elite athletes.
- 2)
Current interventions are based largely on clinical experience and evidence derived from research in other fields, far removed from elite athletics.
- 3)
More sophisticated research methodology is required.
Previous research in the fields of aviation, transportation, and the military has established that sleep is an active physiologic state, during which critical metabolic, immunologic, and cognitive/memory processes occur. Sleep-deprivation studies have demonstrated a significant effect on glucose metabolism, appetite, and fat deposition. Cognitive performance (psychomotor vigilance) has been shown to be directly affected by sleep deprivation, with a distinct interindividual variability in the response to various doses of sleep deprivation. The impact of sleep disturbance on learning and neural plasticity has also been established. The positive or mitigating effect of recovery sleep (strategic napping) has been established as well in sleep-deprivation studies.
Current research performed to explore the relationship between sleep and PER and performance in athletes has been of questionable value because of the multiple variables affecting sleep in athletes, the limitations of the research methodology, and the small sample sizes. To establish an effective research plan, the first step is to identify the key sleep factors of interest (primary outcomes) and to identify valid, reliable measures for subjective capture of these data. With these tools, the relationship of sleep to PER and performance can be explored in a structured fashion. Sleep length (total sleep requirement: hours/night), sleep quality (sleep disturbance or fragmentation), and sleep phase (circadian timing of sleep) are the key factors affecting the overall recuperative outcome of the sleep state. Valid, reliable, subjective and objective measures of these factors can be used to explore the relationship of sleep to PER and performance in athletes. This article describes the theoretic concepts, discusses the results of pilot study data and proposes future research directions.
Theoretical concepts
Sleep Requirement (Total Sleep Time)
There is great interest and debate over the optimum amount of sleep (sleep length) required for humans to recuperate and function normally. Van Dongen and colleagues have shown a dose-response relationship between hours of sleep deprivation and decline in cognitive function using the psychomotor vigilance task. Although a research subject’s performance was relatively stable over the course of the experiment, there were significant differences among subjects in their responses to the negative effects of sleep deprivation. In other words, different subjects respond differently to the same amount of sleep deprivation. Walker and Stickgold have summarized the relationship of sleep to consolidation of skill memory and performance enhancement, concluding that sleep restriction poses a risk to sleep-dependent memory consolidation and neural plasticity. Thus a causal relationship exists among sleep, memory, and performance. These results substantiate the importance of adequate sleep (amount and quality) for athletes to ensure optimal performance when cognitive tasks and psychomotor vigilance is required. Human sleep deprivation studies support the assumption that sleep restriction (sleep debt) has a negative effect on neuroendocrine and immune function. Critical metabolic and immune processes are known to occur during specific stages of sleep. Therefore, a critical relationship exists between physiologic recovery during the sleep state and an athlete’s ability to train at maximum capacity with optimal results. Overtraining syndrome or chronic training fatigue is a common phenomenon that negatively affects athletes, and is believed to be predominantly the result of immunologic, neuroendocrinological, and musculoskeltal factors. Therefore, determination of an athlete’s total sleep need and ongoing sleep debt is likely a critical factor affecting PER, performance and susceptibility to overtraining syndrome.
Sleep Quality (Sleep Disturance)
Nonrestorative sleep is the descriptor used to account for the fact that some people get enough sleep (achieve their total sleep need) on a nightly basis, but the quality of the sleep is inadequate. Sleep quality is disturbed by sleep fragmentation as a result of recurrent arousal throughout the sleep period, without full awakening, or light sleep as a result of a hyperaroused state, with recurrent awakening throughout the sleep period. Brief arousal and full awakening during the sleep period are associated with a sympathoadrenal response that negatively impacts sleep quality. Athletes who suffer with nonrestorative sleep may be tired from training as well as from not achieving the full restorative benefit of their sleep. Therefore, determining the athlete’s sleep quality is another sleep factor that could be a critical determinant of PER, performance, and prevention of overtraining.
Timing of Sleep (Circadian Phase)
The circadian timing of sleep directly affects sleep length and sleep quality. The circadian phase is both genetically and environmentally determined in humans. Each athlete has a preferred sleep schedule that suits his or her circadian phase; however, training, school, and work commitments can have a substantial impact on the athlete’s ability to match the circadian phase to the sleep schedule. If the circadian preference and sleep schedule are not matched and are out of phase, this will affect the amount and quality of the sleep. For example, night owls who prefer to go to bed later and sleep in (1 am –9 am ) and who then have to wake up at 5 am to train at 6 am will curtail their sleep by 2 to 4 hours per night, missing critical periods of rapid eye movement (REM) sleep and slow wave sleep.
The clinical significance of sleep, recovery, and performance
Case 1
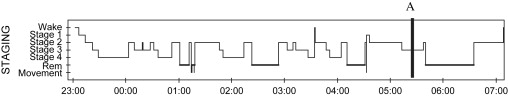
A 19-year-old male university swimmer presented with a 3-year history of increasing fatigue and inability to tolerate standard training volume and intensity, following a prolonged viral illness. The sleep history was significant for a lifetime of light nonrestorative sleep and intermittent violent myoclonic jerking in sleep. Teammates would not share a room with him because of his habit of banging the wall throughout the night. His mother reported an occasion when the athlete was sleeping in the passenger seat of a car and he struck her while she was driving. The provisional diagnosis was periodic limb movement disorder and nonrestorative sleep. The hypnogram of sleep ( Fig. 1 ) revealed an absolutely normal night of sleep with appropriate sleep staging. The sleep electroencephalograph (EEG) revealed a pattern, referred to as alpha-delta intrusion, consistent with that seen in patients who describe “nonrestorative sleep.” The synchronized digital video revealed normal myoclonic jerking in sleep. The key clinical factor in this case is the fact that this athlete is being chronically sleep restricted by 1 to 2 hours per day when morning training begins at 6 am . The chronic sleep restriction deprives the athlete of a long period of REM sleep in the morning. The combination of chronic sleep restriction and REM sleep deprivation contributes to ongoing fatigue; impaired memory, cognition, and learning; and finally impaired immunologic function. This could account for the prolonged recovery from the viral insult.
Case 2
A 17-year-old female ice hockey goalie presented with initial insomnia and situational anxiety. She was diagnosed with a delayed sleep phase, with a preferred sleep schedule of 1 am to 9 am . Attempts at going to sleep earlier than 11 pm resulted in a 2-hour sleep onset latency, causing anxiety over not being able to fall asleep. This was inadequately treated with a sedative/hypnotic (7.5 mg of zopiclone nightly at bedtime). She was waking early for training at 6 am and having trouble with her training regimen. Once the delayed sleep phase was treated with a seasonal affective disorder (SAD) light, which advances the sleep phase by adjusting melatonin secretion, she was able to adjust her training schedule. She was then able to fall asleep earlier and wake spontaneously at 7 to 8 am . She began going to the gym later, at 9 am, and experienced major positive benefits in her training, including weight gain, improved strength, and better performance. The sedative medication was no longer needed once the sleep phase was advanced. Delayed sleep phase syndrome is a circadian rhythm disorder that is best treated with chronotherapy (SAD light and/or melatonin) and not a sedative/hypnotic. This case illustrates the importance of a comprehensive sleep assessment for determination of the cause of initial insomnia. Additionally, adjustment of the sleep phase improved the training regimen and response.
Case 3
A 20-year-old female university swimmer who had a 6-year history of chronic daytime fatigue and recurrent upper respiratory tract infections followed by a bout of mononucleosis was referred for a sleep assessment. The sleep history revealed a preference for a delayed sleep phase, predisposition to initial insomnia, and according to the parents, loud, disruptive snoring. She was referred for ongoing fatigue and possible sleep disorder. The medical workup for fatigue was negative. She was being treated for depression with 20 mg of citalopram every morning, and her mood was stable. Sleep history was unremarkable except for the snoring. A sleep apnea screening study was performed, and she had evidence of high upper airway resistance associated with the snoring. This is a well-described phenomenon that is known to cause recurrent arousals throughout the night, similar to sleep apnea, as a result of partial closure of the airway, increased resistance to airflow, and increased respiratory effort. A therapeutic trial of an autotitrating positive airway pressure (autoPAP) device was done for 2 weeks, followed by 2 weeks off therapy. The patient noted a substantial improvement in her daytime fatigue with therapy. This case points to the importance of careful exploration of the sleep history in order to determine if any primary sleep disorders could be disturbing the quality of the sleep on a chronic basis.
These clinical cases exemplify the importance of determining the athlete’s total sleep requirement, the presence of sleep disturbance/fragmentation, and the athlete’s preferred circadian sleep phase. Evaluating these sleep factors may explain an athlete’s ongoing problems with nonrestorative sleep and chronic training fatigue. More importantly, optimizing these sleep factors for the athlete may have a substantial impact on training, PER, and performance.
The clinical significance of sleep, recovery, and performance
Case 1
A 19-year-old male university swimmer presented with a 3-year history of increasing fatigue and inability to tolerate standard training volume and intensity, following a prolonged viral illness. The sleep history was significant for a lifetime of light nonrestorative sleep and intermittent violent myoclonic jerking in sleep. Teammates would not share a room with him because of his habit of banging the wall throughout the night. His mother reported an occasion when the athlete was sleeping in the passenger seat of a car and he struck her while she was driving. The provisional diagnosis was periodic limb movement disorder and nonrestorative sleep. The hypnogram of sleep ( Fig. 1 ) revealed an absolutely normal night of sleep with appropriate sleep staging. The sleep electroencephalograph (EEG) revealed a pattern, referred to as alpha-delta intrusion, consistent with that seen in patients who describe “nonrestorative sleep.” The synchronized digital video revealed normal myoclonic jerking in sleep. The key clinical factor in this case is the fact that this athlete is being chronically sleep restricted by 1 to 2 hours per day when morning training begins at 6 am . The chronic sleep restriction deprives the athlete of a long period of REM sleep in the morning. The combination of chronic sleep restriction and REM sleep deprivation contributes to ongoing fatigue; impaired memory, cognition, and learning; and finally impaired immunologic function. This could account for the prolonged recovery from the viral insult.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






