Interest in scuba (self-contained underwater breathing apparatus) diving increased in the 1970s, and undersea diving continues to be a popular sport early in the 21st century, with approximately 3 million certified divers in the United States. The Divers Alert Network (DAN), an institution created in 1981 by the Commerce Department, National Oceanic and Atmospheric Administration, has collected diving injury data for US and Canadian divers since 1987 that can be studied to suggest the epidemiologic characteristics of diving. This article examines neurologic injuries resulting from scuba diving.
Interest in scuba (self-contained underwater breathing apparatus) diving increased in the 1970s, and undersea diving continues to be a popular sport early in the 21st century, with approximately 3 million certified divers in the United States. The Divers Alert Network (DAN), an institution created in 1981 by the Commerce Department, National Oceanic and Atmospheric Administration, has collected diving injury data for US and Canadian divers since 1987 that can be studied to suggest the epidemiologic characteristics of diving.
The 2006 annual DAN Diving Report on Diving Injuries and Diving Fatalities is based on data collected during 2004. This diving report presents information on Project Dive Exploration (PDE), which is a prospective observational study of recreational diving yearly data since 1995. PDE divers are volunteers from the general recreational diving population, but they are not necessarily representative of this population. Most PDE divers are 30 to 50 years of age; 22% are over the age of 50, and 4% are under 20 years of age. Thirty percent of the divers are female. Sixty-six percent of the female divers hold open water, advanced open water, or specialty certification, verses 46% of the males.
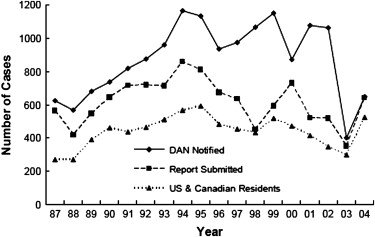
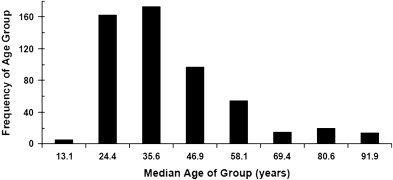
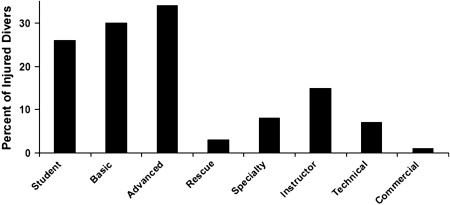
The annual number of injury cases reported has increased from 1987 to 2004, with about 600 cases in 1987 and 1100 cases in 2002 ( Fig. 1 ). The dramatic dip noted in 2003 represents decreased data collection because of the Health Insurance Portability and Accountability Act (HIPAA). The mean age of divers in the DAN injury population was 39 years ( Fig. 2 ). Interestingly, divers with advanced certification had the highest percentage of injuries, but this may be due to unknown diving frequency and may differ between the varying certification categories ( Fig. 3 ).
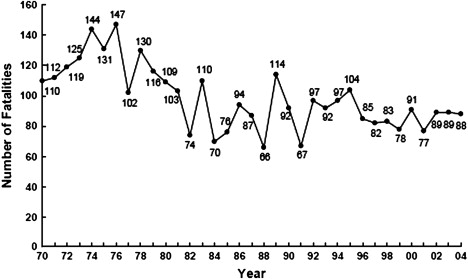
The annual record of US and Canadian diving fatalities, began in 1971 by John McAniff of the University of Rhode Island, was transitioned to DAN in 1989. The number of fatalities reported from 1970 to 2004 ranges from 80 to 120 annually, with a stable number of fatalities ( Fig. 4 ). The general diving population seems to be aging, as a larger percentage of divers have been diving for more than a decade since certification. This aging of the diving population may account for the increase in the mean age of diving fatalities from 1989 to 2002. The mean age of divers experiencing injuries also increased from 33 to 39 years during this time.
Medical history (limited) was available in 40% of the fatality cases, and the most frequently reported medical conditions were heart disease and high blood pressure. Most of the fatalities in the DAN Report had open water or advanced certification, and 25% had been certified 10 years or greater, whereas 45% had 1 year or less. This report does not specify the dive frequency among the fatalities. The most common cause of death in the judgment of the DAN pathologist reviewing each case was drowning, whereas the next most common causes were an acute heart condition or an arterial gas embolism. The cause of death was not determined in 10% of the cases, either because the body was not found or the cause was not identified by the local medical examiner.
Decompression sickness
Decompression sickness occurs when inert gas comes out of solution, forming bubbles following the reduction of surrounding pressure (decompression). This commonly occurs with breathing compressed air while diving. As the diver descends and is exposed to elevated environmental pressure, increased amounts of inert gas dissolve in the tissues. This is in accordance with Henry’s law, which states that the amount of gas dissolved in a fluid is directly proportional to the partial pressure of that gas. The amount of inert gas dissolved depends on the depth and the duration of the dive. If the diver ascends too quickly, the inert gas taken up during the dive exceeds solubility at the reduced pressure, and leads to bubble formation in tissues and in venous blood. The extent of bubble formation depends on the depth and duration of the dive and the rate of the ascent.
The likelihood of decompression sickness is related to the extent of bubble formation. A few bubbles coming out of solution may cause only minor symptoms; however, a large bubble load may result in multisystem failure and death. There are two general types of decompression sickness, Type I and Type II. Small gas loads typically cause Type I decompression sickness, which is characterized by pain in the joints and limbs and itching in the skin (niggles). Decompression sickness Type II is serious, and is characterized by neurologic problems such as weakness or paralysis, limb paresthesias, disturbance of vision, bowel and bladder dysfunction, and vertigo. Most often, the target organ is the spinal cord, usually the thoracic level. The thoracic level is probably targeted because of the vascular anatomy of the spinal cord. The paravertebral veins (Batson’s plexus) allows for bubbles to collect because of stagnant flow resulting in venous infarction in the spinal cord. Cerebral involvement occurs in 30% of the cases of Type II decompression sickness. Divers who have cerebral involvement may complain of confusion, lethargy, mental cloudiness, difficulty with concentration, visual disturbances and dysphagia. Symptoms typically begin within an hour of surfacing, but may be delayed for several hours. An earlier symptom onset may indicate a greater bubble load and a worse prognosis.
The diagnosis of decompression illness is based on the clinical examination, including the neurologic examination, and the dive history. Laboratory and imaging studies sometimes add to the diagnosis. In 2004 Freiberger identified important diagnostic factors using simulated diving injury cases. The top five diagnostic factors in order of importance were: (1) a neurologic symptom as the primary presenting symptom, (2) onset time to symptoms, (3) joint pain as a presenting symptom, (4) any relief after recompression treatment, and (5) maximum depth of the last dive. Age, gender, or physical characteristics were not statistically important.
Decompression sickness: case one
A 32-year-old sport diver with several years experience was in the fifth day of a diving vacation trip to the South Pacific. On each of the previous days, he had made two or three dives, and at least one dive each day had exceeded 100 feet. He was using a decompression computer and was quite sure that he had stayed within the parameters required by the computer throughout his trip. On the fifth day, he made one dive to 150 feet and three dives to 90 feet, each separated by surface intervals that met the requirements of his computer. About 5 minutes after surfacing from his third 90-foot dive, as he was sitting on the bench, he had an aching, pressurelike pain around his flanks and into his groin. The right side was somewhat worse than the left, but as the pain became more intense, both sides were equally affected. A few minutes later, he got to his feet and was unable to walk without assistance. His companions and the boat captain helped him to the bench, where he lay down and was treated with oxygen. Symptoms did not improve. Arrangements were made to evacuate him to a recompression chamber on an island several hundred miles distant. The flight was delayed by darkness. When he arrived at the chamber the next day, about 10 hours after onset, he had moderate weakness in both thighs and virtually no strength in his left foot and lower leg, with his right foot less affected. He had altered sensation and patchy loss of sensation from the umbilicus downward, although he could feel pressure in his feet. He was unable to void without pressing on his abdomen. On urinary catheterization, he had 1500 mL residual urine. Reflexes were hyperactive.
He was treated according to US Navy Table 6. He made some improvement during the first 2 hours and treatment was extended to a full 10 hours. At the conclusion of treatment, his quadriceps and thigh strength had largely returned; his left foot was still nearly flaccid, but his right was only slightly weak. Sensation was improved, and pain resolved. The indwelling catheter was removed on the second day, and he was able to void with a Crede maneuver.
He was retreated on Table 5 (shorter oxygen table) for each of the following 3 days. He made no further improvement after the first treatment.
A week after completion of treatment, he returned to the United States by commercial aircraft. There was no change in his symptoms. In the ensuing year, he reported slow improvement in his mobility and in bladder control. One year after the event, he had persistent spastic paraparesis. He was able to ambulate without a cane or crutches, but with moderate discernable weakness and bilateral hyperreflexia. Sensation about the perineum was decreased and was nearly normal in the feet.
This case typifies serious decompression sickness with delayed treatment and with partial response. Although this patient was diving “within the rules,” he had accumulated a large gas load.
Decompression sickness: case one
A 32-year-old sport diver with several years experience was in the fifth day of a diving vacation trip to the South Pacific. On each of the previous days, he had made two or three dives, and at least one dive each day had exceeded 100 feet. He was using a decompression computer and was quite sure that he had stayed within the parameters required by the computer throughout his trip. On the fifth day, he made one dive to 150 feet and three dives to 90 feet, each separated by surface intervals that met the requirements of his computer. About 5 minutes after surfacing from his third 90-foot dive, as he was sitting on the bench, he had an aching, pressurelike pain around his flanks and into his groin. The right side was somewhat worse than the left, but as the pain became more intense, both sides were equally affected. A few minutes later, he got to his feet and was unable to walk without assistance. His companions and the boat captain helped him to the bench, where he lay down and was treated with oxygen. Symptoms did not improve. Arrangements were made to evacuate him to a recompression chamber on an island several hundred miles distant. The flight was delayed by darkness. When he arrived at the chamber the next day, about 10 hours after onset, he had moderate weakness in both thighs and virtually no strength in his left foot and lower leg, with his right foot less affected. He had altered sensation and patchy loss of sensation from the umbilicus downward, although he could feel pressure in his feet. He was unable to void without pressing on his abdomen. On urinary catheterization, he had 1500 mL residual urine. Reflexes were hyperactive.
He was treated according to US Navy Table 6. He made some improvement during the first 2 hours and treatment was extended to a full 10 hours. At the conclusion of treatment, his quadriceps and thigh strength had largely returned; his left foot was still nearly flaccid, but his right was only slightly weak. Sensation was improved, and pain resolved. The indwelling catheter was removed on the second day, and he was able to void with a Crede maneuver.
He was retreated on Table 5 (shorter oxygen table) for each of the following 3 days. He made no further improvement after the first treatment.
A week after completion of treatment, he returned to the United States by commercial aircraft. There was no change in his symptoms. In the ensuing year, he reported slow improvement in his mobility and in bladder control. One year after the event, he had persistent spastic paraparesis. He was able to ambulate without a cane or crutches, but with moderate discernable weakness and bilateral hyperreflexia. Sensation about the perineum was decreased and was nearly normal in the feet.
This case typifies serious decompression sickness with delayed treatment and with partial response. Although this patient was diving “within the rules,” he had accumulated a large gas load.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






