6 Spinal Fractures
Overview
 Anatomic Features
Anatomic Features
The spinal column consists of individual bony vertebrae and intervertebral disks that connect each vertebra in the front of the spine. A healthy spine provides strength, is flexible, and allows movement in several planes. Body movement and weight-bearing changes can produce an alteration in the geometry of the spine. The vertebral column is made of 26 separate vertebrae, and can be divided into five sections: cervical, thoracic, lumbar, sacral, and coccygeal. Because the sacrum and coccyx are fused with five sacral vertebrae and four coccygeal vertebrae, respectively, some believe the vertebral column is actually made up of 33 vertebral bones. Each vertebra is composed of a body anteriorly and a neural arch posteriorly. The arch has two supporting pedicles and two arched laminae; it encloses an opening, the vertebral foramen, which helps to form the vertebral canal in which the spinal cord is housed. Seven processes arise from the vertebral arch: the central spinous process, two transverse processes, two superior facets, and two inferior facets. Three-quarters of the length of the vertebral column is from the vertebral bodies, and one-quarter is from the thickness of the intervertebral disks.
Two important concepts have emerged during the study of the spine’s anatomic features. They are the two-column concept and three-column concept. In 1968, Kelly and Whitesides proposed a two-column concept that aided the assessment of angular deformation (Plate 6.1). The two columns, specifically the anterior and posterior column, are defined as involving the vertebral bodies and neural arches, respectively, and are delineated by the posterior longitudinal ligament. The anterior column is composed of the anterior longitudinal ligament, posterior longitudinal ligament, and vertebral body. The posterior column, otherwise known as the hollow column, is composed of the vertebral canal and the posterior ligamentous complex. Kelly and Whitesides highlighted the importance of the posterior ligamentous complex in the assessment of spine stability. However, the two-column concept is limited in assessing posterior nerve root injury in spine fractures, and has been gradually replaced by the three-column concept.
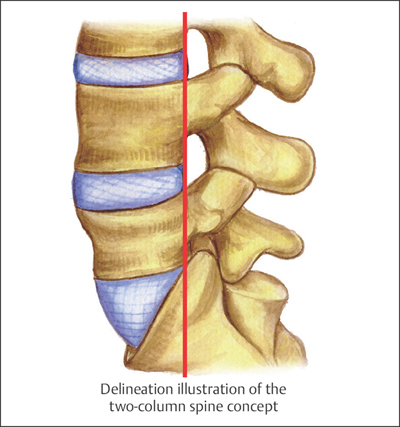
Plate 6.1
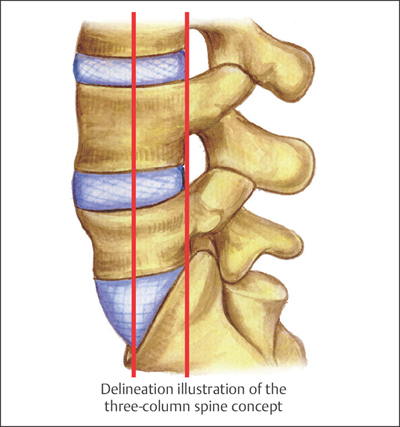
Plate 6.2
The three-column concept was introduced by Denis in 1983, and is able to reach better agreement with clinical observations regarding spine stability than the two-column concept (Plate 6.2). It divides the spine into three columns: the anterior, middle, and posterior columns. Using this scheme, the anterior column is composed of the anterior half of the vertebral body and the intervertebral disk, and the anterior longitudinal ligament; the middle column includes the posterior part of vertebral body and the disk, and the posterior longitudinal ligament; the posterior column includes the pedicles, the facet joints, and the supraspinous ligaments. In 1983, McAfee proposed that the demarcation lies between the anterior and middle columns at the junction of the anterior two-thirds and posterior one-third of the vertebral body, instead of the midpoint of the vertebral body as proposed by Denis. With McAfee’s scheme, fractures involving the middle column are unstable fractures. This concept is able to provide a better and more accurate assessment of spinal stability and neurologic injury.
 AO Classification and Coding System for Spine Fractures
AO Classification and Coding System for Spine Fractures
Based on AO classification, the spinal column is coded as the number “5.” Cervical, thoracic, lumbar, and sacral fractures are assigned as numbers “51,” “52,” “53,” and “54,” respectively. Pelvic fractures always involve sacrococcygeal fractures; therefore, we put sacral and coccygeal fractures into the pelvic section during our statistical analysis.
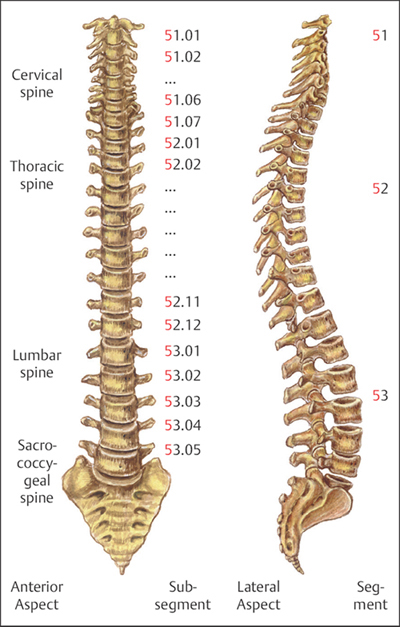
Plate 6.3
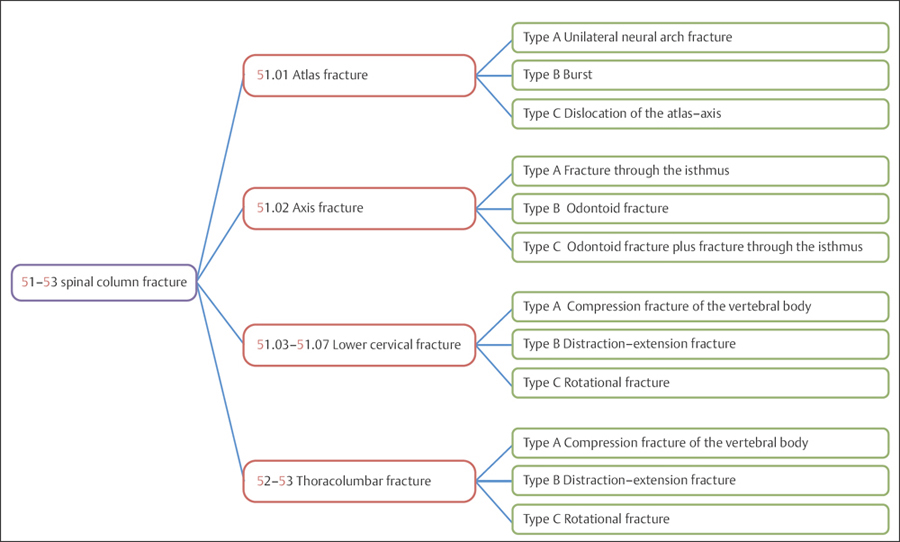
Plate 6.4
Because the atlas (51.01) and axis (51.02) have different anatomic features and unique functions from other cervical vertebrae, they require different methods of assessment regarding the stability and neurologic injury resulting from fractures. As such, AO classification places vertebral column fractures into four sections: atlas, axis, lower cervical, and thoracolumbar fractures. The atlas and axis constitute the upper cervical spine.
For AO classification of spine fractures, the number “5” is assigned for the spine; “51” for the cervical spine, 51.01–51.07 for vertebrae C1–C7, respectively (Plate 6.3); “52” for the thoracic spine, 52.01–52.12 for vertebrae T1–T12, respectively; “53” for the lumbar spine, 53.01–53.05 for L1–L5, respectively (Plate 6.4).
 Clinical Epidemiologic Features of Fractures of the Spinal Column
Clinical Epidemiologic Features of Fractures of the Spinal Column
A total of 4175 patients with 4720 spinal column fractures were treated at our trauma center over a 5-year period from 2003 to 2007. All cases were reviewed and statistically studied; the fractures accounted for 6.93% of all patients with fractures and 7.23% of all types of fractures, respectively. Among these 4175 patients, there were 44 children and 4131 adults.
Epidemiologic features of fractures of the spinal column are as follows:
• more males than females
• the high-risk age group is 41–50 years—the same age group for both males and females
• thoracolumbar fractures occur more frequently than cervical or sacrococcygeal fractures.
 Spinal Column Fractures by Sex
Spinal Column Fractures by Sex
Table 6.1 Sex distribution of 4175 patients with spinal column fractures
| Sex | Number of patients | Percentage |
| Male | 2263 | 54.20 |
| Female | 1912 | 45.80 |
| Total | 4175 | 100.00 |
Fig. 6.1 Sex distribution of 4175 patients with spinal column fractures.
 Spinal Column Fractures by Age Group
Spinal Column Fractures by Age Group
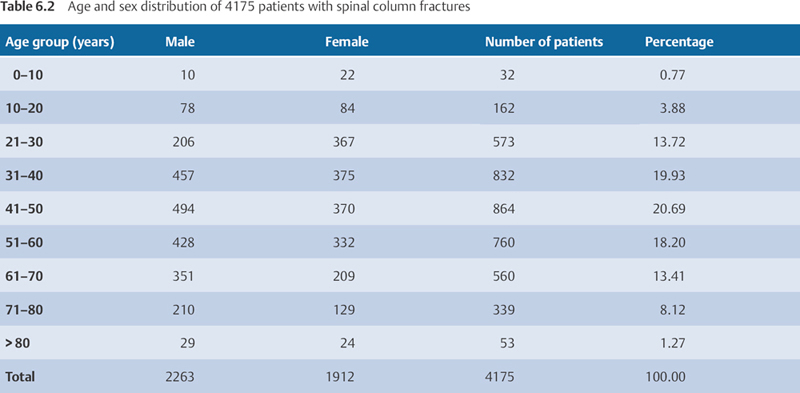
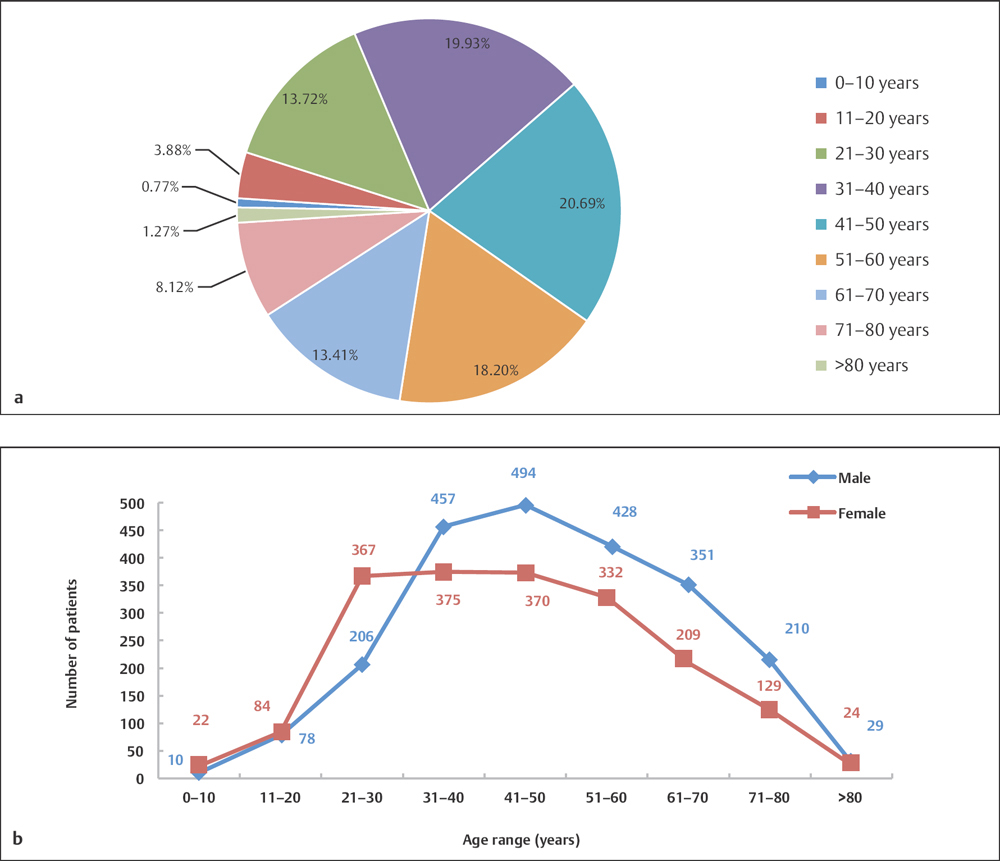
Fig. 6.2 a, b
a Age distribution of 4175 patients with spinal column fractures.
b Age and sex distribution of 4175 patients with spinal column fractures.
 Spinal Column Fractures by Segment
Spinal Column Fractures by Segment
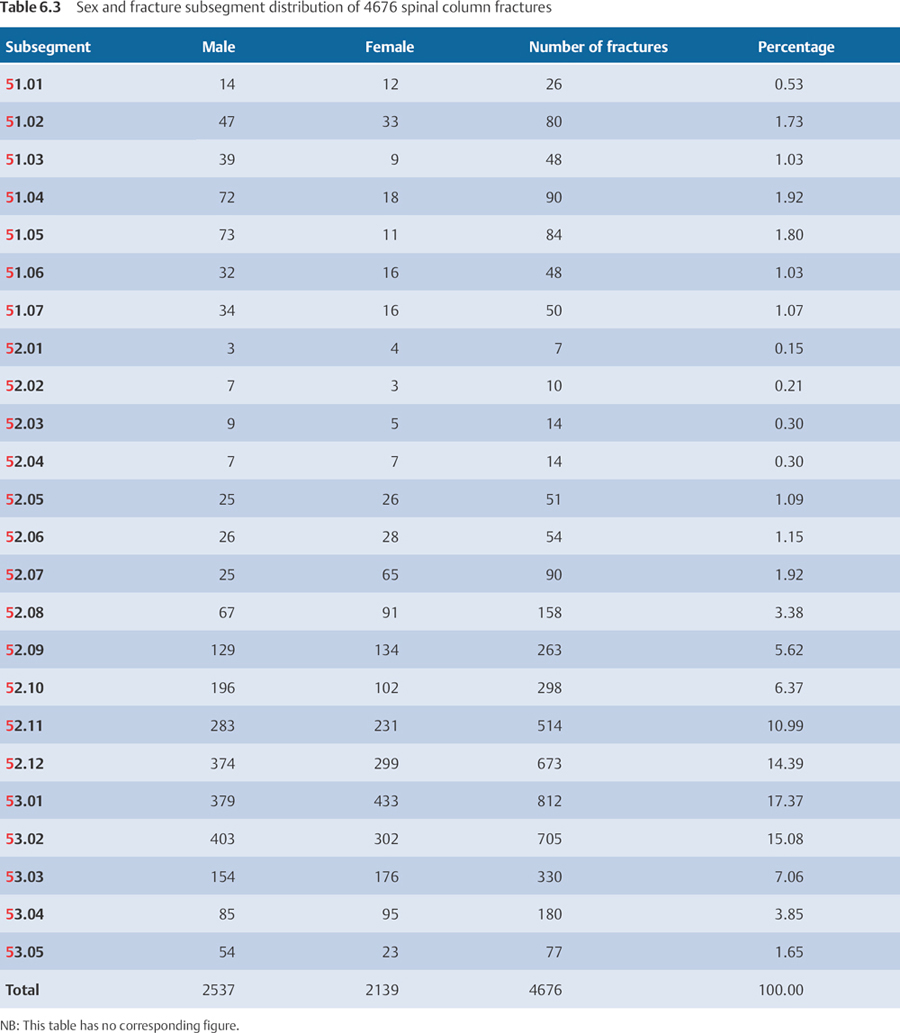
Cervical Fractures (Segment 51)
 Anatomic Features
Anatomic Features
The first two vertebral bodies in the cervical spine are called the atlas and the axis. They are very special with respect to their unique anatomic features and functions; therefore, assessment of injuries to the atlas and axis are very different from injuries to other vertebrae. AO classification has special descriptions for fractures of the atlas and axis (Plate 6.5).
The atlas, a ring-shaped bone, is remarkable for having no “body.” It consists of anterior and posterior arches, and two lateral masses, from which two transverse processes project laterally and downward. Its superior articular facets articulate with the occipital condyles of the skull, and it forms the atlantoaxial joint with the dens of the axis. The two transverse processes of the atlas serve as attachment sites for muscles and ligaments, which assist in rotating the head. The foramen transversarium pierces the transverse processes of the atlas, and gives passage to the vertebral artery and vein. The anterior and posterior arch is thin, especially at their junction with the lateral mass, which is particularly susceptible to injury and, if damaged, may lead to fracture and dislocation.
The dens of the axis was originally part of the atlas, but became separated from the atlas during development; therefore, malformations commonly occur, such as absence of the dens of axis, hypoplasia or agenesis of the dens, occipital–atlas fusion, and atlas–axis fusion. These malformations may result in poor stability of the craniocervical region and compression of the spinal cord. The root of the dens is very thin, making it especially prone to injury. The resultant fracture and dislocation of the root would lead to a high risk of paraplegia or even death (Plate 6.5).
There are important ligaments between the atlas and axis, connecting two or more bones, condrites, or other soft tissues. The atlantoaxial ligament complex provides stability to the atlantoaxial joint though its great range of motion, and prevents hyperflexion or hyperextension of the joint (Plate 6.6). The upper cervical ligament is important in stabilizing the upper cervical spine and preventing neurologic injury. Loss of stability of the ligament can result in subluxation of C1–C2, and lead to lethal neurologic injuries.
Each vertebra in the lower cervical spine (C3–C7) consists of a vertebral body, a vertebral arch, which is formed by a pair of pedicles, and a pair of laminae (Plate 6.7). Each vertebra also has seven processes, four articular, two transverse, and one spinous. By comparison, cervical vertebrae are smaller than thoracolumbar vertebrae. The lateral aspect of each vertebral body has a superior projection (uncinate process) that forms Luschka’s joints (uncovertebral joints) with a projection downward from the inferior surface of the vertebral body above. The transverse process is short and broad, with a wide groove for the existing spinal nerve on its upper surface. It gives attachment to several muscles. The bony protuberances at the end of the transverse processes are called the anterior and posterior tubercles, accordingly. The articular facets are inclined ~ 45° from the horizontal plane. A characteristic feature of vertebrae C2 to C6 is a projection known as the bifid spinous process, whereas C7 has a prominent nonbifid spinous process that can be felt at the base of the neck.
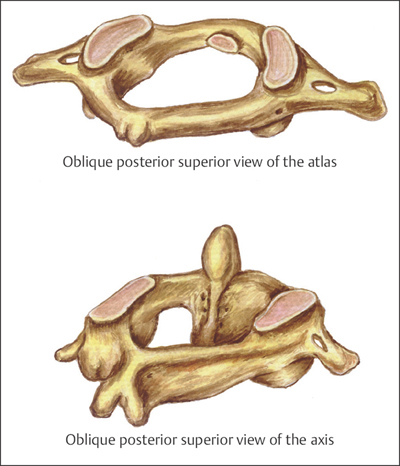
Plate 6.5
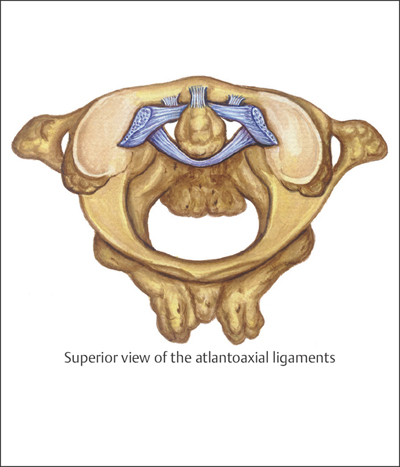
Plate 6.6
 AO Classification of Cervical Spine Fractures
AO Classification of Cervical Spine Fractures
Based on AO classification, 51.01 (atlas) fractures can be divided into three types: A: unilateral neural arch fractures; B: burst fractures; and C: dislocation of the atlas–axis. 51.02 (axis) fractures can also be grouped into three types: A: fractures through the isthmus, including neural arch (ring) fractures or hangman’s fractures; B: odontoid fractures; and C: fractures through the isthmus plus an odontoid fracture. AO classification for segment 51.03–51.07 (lower cervical spine) has three categories: A: compression fractures of the vertebral body; B: distraction injuries of the anterior and posterior elements; and C: rotational injuries with translation affecting the anterior and posterior elements (Plate 6.8).
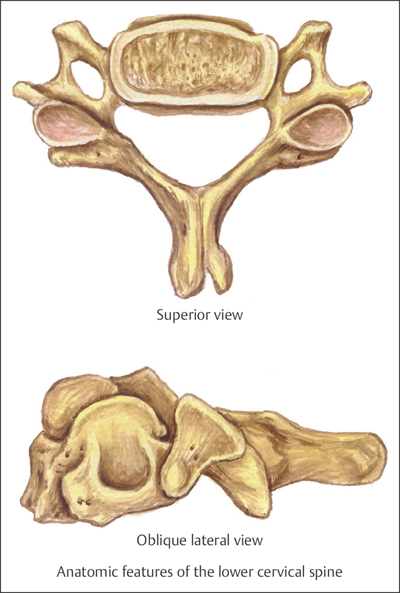
Plate 6.7
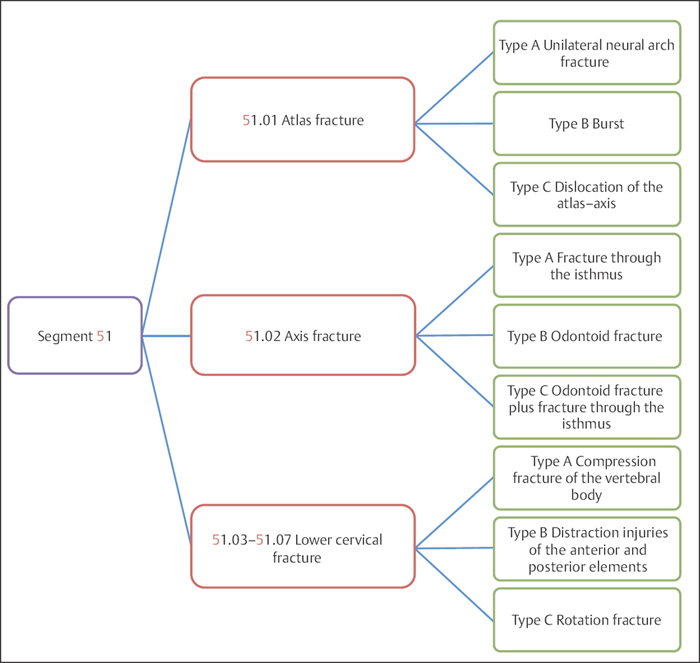
Plate 6.8
 Clinical Epidemiologic Features of Fractures of the Upper Cervical Spine (Segment 51.01–51.02)
Clinical Epidemiologic Features of Fractures of the Upper Cervical Spine (Segment 51.01–51.02)
A total of 106 adult fractures of the upper cervical column were treated at our trauma center over a 5-year period from 2003 to 2007. All were reviewed and statistically studied; the fractures accounted for 2.27% of all spinal column fractures in adults. Their epidemiologic features are as follows:
• more males than females
• the highest-risk age group is 41–50 years
• the most common type of fracture among segment 51.01 (atlas) fractures is type A
• the most common type of fracture among segment 51.02 (axis) fractures is type B.
 Fractures of Segment 51.01–51.02 by Sex
Fractures of Segment 51.01–51.02 by Sex
Table 6.4 Sex distribution of 106 upper cervical spine fractures
| Sex | Number of fractures |









