Spica Cast Application for Femur Fractures
William L. Hennrikus
Howard R. Epps
INDICATIONS/CONTRAINDICATIONS
Early spica casting is indicated for the otherwise healthy child from 6 months to 6 years of age with an isolated femoral shaft fracture stemming from a low-energy injury with intact soft tissue, no evidence of compartment syndrome, and a reliable home environment. There has been a trend to place intramedullary (IM) flexible nails in younger children with isolated femoral shaft fractures, and at times, one may consider IM flexible nails in children ≤6 years of age, depending on the family’s wishes and other factors (Heffernan et al.). Femoral fractures in children younger than 6 months of age are best treated with another method, such as a Pavlik harness. In addition, open femoral fractures or fractures associated with multitrauma are not routinely treated with a spica cast; instead, surgical treatment is usually preferred.
Spica cast treatment for the child up to 6 years of age minimizes hospitalization and allows the child to return to the home environment in 1 to 2 days. Attention to detail during cast application and adherence to the indications for the use of spica casting are necessary to achieve a good result. Family teaching about care of the child while in the spica is also key.
PREOPERATIVE PLANNING
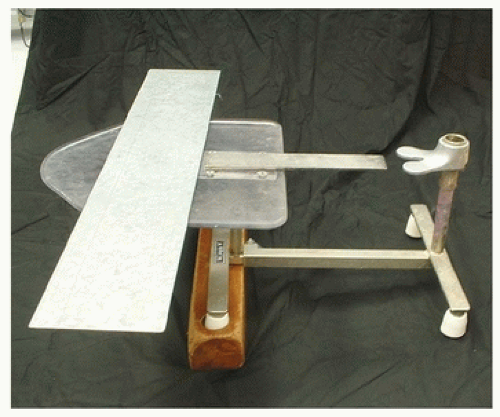
All the necessary materials and assistants needed for application of the cast should be in the room at the start of the procedure. Two assistants are needed to hold the child on the spica table and help apply the spica cast. A radiology technician and fluoroscopic or permanent radiographic imaging are also required. Materials needed include a spica table, an armrest bar (such as a 60 in. × 4 in. × 1/8 in. sheet of stainless steel), and a 2 in. × 2 in. × 3 ft. wood block to elevate the proximal legs of the spica table (Fig. 9-1). The wood elevator tilts the spica 10 degrees so that the patient’s perineum fits snugly onto the perineal post on the spica table. If the procedure is performed in the operating room, a wood elevator is not needed; instead, the operating room table can be tilted 10 degrees for the same effect. A radiolucent spica table is now commercially available (Orthopediatrics, Warsaw, IN) (Fig. 9-2).
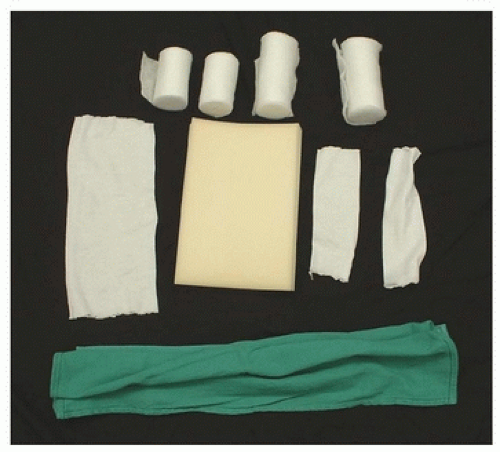
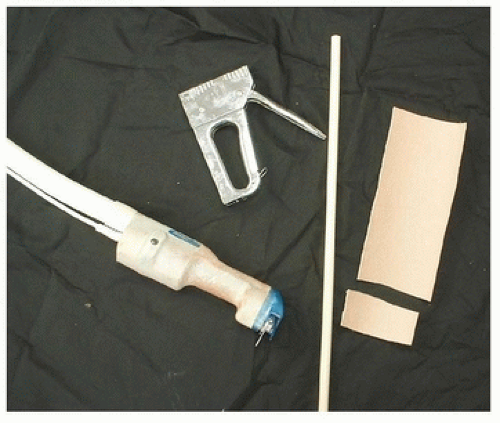
Necessary casting and padding materials include stockinette in multiple sizes (2 in., 3 in., and 4 in.) to cover the legs and abdomen, a folded towel to pad the abdomen, Webril cotton in multiple sizes (2 in., 3 in., and 4 in.), one-quarter self-sticking foam padding to pad bony prominences such as the sacrum and spine, fiberglass in multiple sizes (2 in., 3 in., and 4 in.), fiberglass splints for reinforcing the cast junction between the torso and the leg, towels to provide space for the abdomen, and a bucket of water (Fig. 9-3). Some surgeons use a Gore-Tex cast underliner on the skin as the first layer of the cast, which has the theoretical advantage of being breathable and waterproof; this is not a requirement, however. Materials needed to trim the cast include a cast saw, an industrial-sized staple gun, and moleskin. A one-fourth-inch-diameter wood dowel bar should also be available to connect the legs in the cast for added stability, though this is usually not needed when fiberglass is used (Fig. 9-4). In addition, an instructional handout for the family about spica cast care is very
helpful. Finally, special seat belt straps are required in some states to secure the child in a spica cast during transportation in an automobile.
helpful. Finally, special seat belt straps are required in some states to secure the child in a spica cast during transportation in an automobile.
Application of the spica does not need to be done as an emergency procedure. In general, if the child arrives at the emergency department during normal working hours, the cast can be applied in an immediate fashion. The procedure can be done in the emergency department or procedure room with conscious sedation or in the operating room with general anesthesia. If the child arrives at the emergency department in the evening or on a weekend, the child can be admitted and the injured leg can be placed in Buck skin traction with a small amount of weight (e.g., 5 lb) or just splinted without traction until assistants and an operating room are available. Surgeons should be wary of the possibility of compartment syndrome with tightly wrapped skin traction or ipsilateral leg or foot trauma.
Parents are informed of the risks and benefits of the procedure prior to application of the cast. (See “Complications to Avoid.”) The most important risk to inform the parents of is the potential need to change treatment and remove the spica cast due to unacceptable shortening or angulation. About one in five children placed in an early spica cast will require a change in treatment. This is also the time to set the parents’ expectations that the child may limp for 6 months following a femur fracture; if the child stops limping early, it will just increase the parents’ overall satisfaction with the care. In addition, parents should be informed that overgrowth is not completely predictable. Despite the surgeons’ best efforts, there is a small risk that a child treated with a spica cast for a femoral fracture will have a permanent 2-cm or greater leg length difference and may need an epiphysiodesis at an older age.
SURGICAL PROCEDURE
Spica casts can be applied in the emergency room setting, in the clinic setting, or on the ward under sedation for small children aged 3 years or younger. In general, the spica cast is more easily applied in the operating room under general anesthesia for older or uncooperative children. The traditional one-and-a-half spica cast is applied with the cast extending from the nipple level to the mid- to distal tibia level on the injured side and to the mid- to distal femur level on the uninjured side. The single-leg spica cast extends from the nipple level down to the malleoli of the injured leg. The child is placed supine on the spica table, with the child’s arms secured to the arm board with Webril cotton or held across the child’s chest by an assistant. Securing the arms in this fashion simplifies holding the child. The spica table is tilted 10 degrees downward by placing the wood elevator under the proximal legs of the spica table or by tilting the operating room bed. The one-leg spica cast can simplify care and improve social concerns for simple femur fractures (Epps et al.).
After induction of anesthesia or sedation, stockinette or a Gore-Tex cast liner is applied to all areas to be casted. The patient is then carefully placed onto the spica table. One assistant holds each leg at the ankle and applies gentle traction to the affected side. The goal of positioning the leg is to match the position of the distal fragment to the proximal fragment. For the typical midshaft femoral fracture, the legs are positioned with the hip and knee in mild flexion and with the hip in 20 degrees of abduction and 15 degrees of external rotation, allowing for the effects of the abductor and psoas muscles on the proximal fragment. Proximal one-third fractures should be positioned with more hip flexion. A folded towel at least 2 in. thick is placed on the child’s chest and abdomen beneath the
stockinette to prevent the cast from being too tight and to allow full respiratory excursion while in the cast. If in doubt, make the abdomen padding larger. If the child starts to have decreased oxygen saturation during casting, this is most likely an indication of tight wrapping; removal of the towels is usually curative.
stockinette to prevent the cast from being too tight and to allow full respiratory excursion while in the cast. If in doubt, make the abdomen padding larger. If the child starts to have decreased oxygen saturation during casting, this is most likely an indication of tight wrapping; removal of the towels is usually curative.
Next, three layers of Webril cotton are applied. Extra Webril is applied to bony prominences, such as the fibula head, iliac crest, greater trochanter, and patella. Additional Webril is applied at the top and bottom of the cast so that a soft edge results when the stockinette is folded over. Some surgeons place a self-sticking one-fourth-inch foam pad on the back of the child over the cotton to prevent pressure areas on the sacrum and spine that could result from supine positioning while in the cast.
Just before placing the casting material, AP and lateral imaging may be practiced to make certain the images can be obtained in an expedient fashion while the casting material is hardening, allowing for real-time manipulation of the fracture. Fiberglass rather than plaster is utilized, because fiberglass is lighter, stronger, easier to x-ray through, easier to wedge, and water resistant. Typically, four layers of fiberglass are rolled. The fiberglass is rolled over the Webril, taking care to leave a half-inch area of uncovered Webril at the superior torso and inferior leg area of the cast. The extra Webril in these areas ensures a soft edge when the stockinette is folded over. In addition, fiberglass splints are applied to the groin, buttock, and knee to strengthen the cast and, in most cases, to obviate the need for a connecting bar between the legs. Not using a connecting bar between the legs makes carrying the child on a parent’s hip easier and simplifies peroneal care.
In particular, a splint should be incorporated at the resident’s triangle section of the cast at the inferior lateral buttock area bilaterally. This area typically does not get enough fiberglass coverage from rolling the fiberglass. Splints can be made from a roll of 3-in. fiberglass. Typically, splints are about 6 to 20 in. long and six layers thick.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree