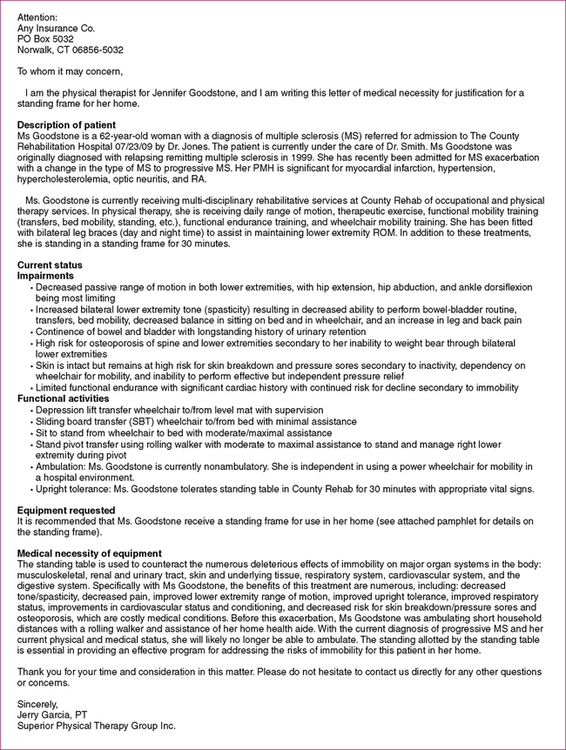
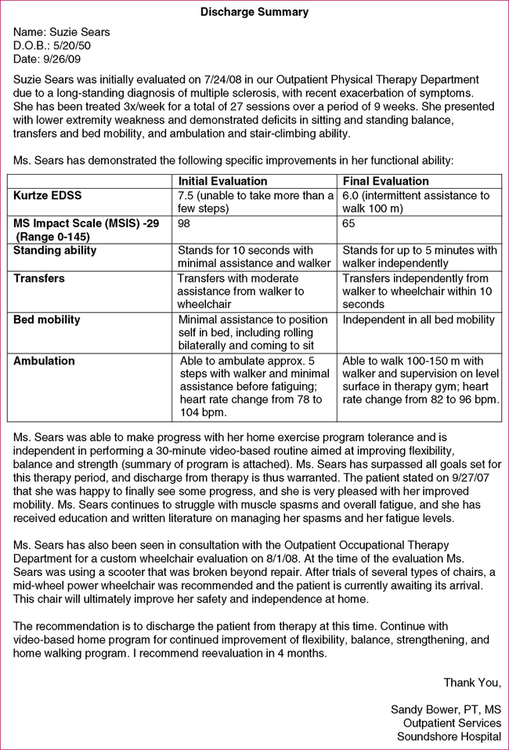
After reading this chapter, the reader will be able to: 1. List the key components of a discharge summary. 2. List the essential features of letters to third-party payers to justify need for equipment or equipment purchases. 3. Identify the key features of letters seeking to appeal denials or requesting continuation of services. 4. Discuss the considerations for providing written patient education materials. The following are essential components of a discharge summary: • Patient description. This should include a description of the patient’s diagnosis and background information and can also include description of current plan of care. • Summary of physical therapy intervention. It should be stated for what length of time and how many sessions the patient received physical therapy services. A brief summary of the interventions that were provided can be provided. • Current status. Summarize the patient’s current status. This can include any impairments but should focus on the patient’s functional abilities and any participation restrictions as appropriate. • Goals. It should be indicated whether the goals were achieved, partially achieved, or not achieved. If goals were not achieved or partially achieved, a brief explanation or justification is warranted. • Recommendations. The PT should list any recommendations for the patient at this point. This plan should include home-based instructions and follow-up or reevaluation instructions. If the patient has moved to another facility (e.g., discharged from acute care to a skilled nursing facility), then any recommendations for continued therapy or other services should be provided. Figure 13-1 is an example of a discharge summary written in an outpatient hospital setting. The following list provides the essential components of a letter of medical necessity: • Patient description. This should include a description of the patient’s diagnosis and background information and can also include a description of the current plan of care. • Current status. Summarize the patient’s current status. This can include any impairments but should focus on the patient’s level of participation and performance of activities as appropriate. • Equipment description. Describe the requested equipment in detail (provide picture or other information if possible). If special components or additions above and beyond standard equipment are required, each item should be separately and explicitly justified. • Medical necessity of equipment. This is the most important component of the letter. The focus here should be on medical necessity. It should include the medical need for the equipment, specify benefits to the patient, and describe the patient’s ability to use the equipment. It is important, whenever possible, to include evidence from the literature to support the need for the equipment. In addition, the inability of any alternatives (particularly cheaper ones) to meet the patient’s medical needs should be discussed if appropriate. Cost benefits can be explained in detail as well. For example, as seen in Figure 13-2, the use of a stander can help prevent skin breakdown and prevent osteoporosis, which are costly medical conditions.
Specialized Documentation
DISCHARGE SUMMARIES
LETTERS TO THIRD-PARTY PAYERS TO JUSTIFY SERVICES OR EQUIPMENT
EQUIPMENT PURCHASES
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Specialized Documentation
Only gold members can continue reading. Log In or Register to continue