Special Interdisciplinary Problem: Knee Dislocation
Troy Caron
H. Claude Sagi
The number of patients who present to the emergency department with a knee dislocation is estimated to be <0.02% of all orthopaedic injuries.1 There are many instances where a dislocated knee has spontaneously reduced before the patient arrives at the treating facility, but this number is unknown. Patients presenting with a multiligamentous knee injury but not a frank dislocation should be treated as having sustained a knee dislocation that spontaneously reduced.
On initial presentation, the patient with a dislocated knee should be treated like any other patient in the trauma setting. Once the patient is stabilized and the primary survey parameters have been addressed, attention should then be directed toward the secondary survey and the status of the extremities. If a knee dislocation is identified or suspected based on position or ligamentous instability, the knee should be reduced and the limb aligned and stabilized as soon as possible. Careful attention to subtle asymmetry in neurologic or vascular examination findings before and following reduction is key.
Only when the knee is reduced and the neurovascular status of the patient is confirmed to be normal can definitive treatment and stabilization for knee instability be considered. Many different combinations of structures in the knee can be damaged with a knee dislocation. These structures include the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), lateral collateral ligament (LCL), posterolateral corner (PLC), menisci, articular cartilage, and bone. Clinical examination, x-rays, and magnetic resonance imaging (MRI) must be obtained for definitive diagnosis of the damaged structures. The treatment options and timing for repair will depend on stability of the patients, what structures have been damaged, and other injuries that the extremity has sustained. The ultimate goal is to restore stability and painfree functional mobility.
CLASSIFICATION
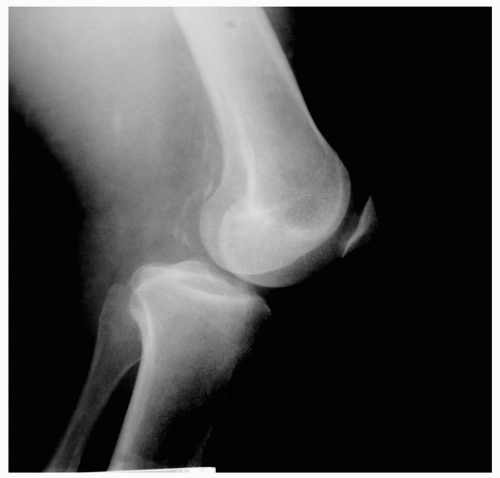
Like all deformity in orthopaedic surgery, dislocations are described by what direction the distal fragment (the tibia) moves in relation to the proximal fragment (the femur). These include anterior, posterior, medial, lateral, and rotatory dislocations.2 Posterior dislocations, the result of a force causing the tibia to be driven anteriorly, are the most common representing more than 70% of the dislocations and likely result from a hyperextension mechanism (see Fig. 1). Studies have shown that when the knee is hyperextended greater than 30 degrees the knee will dislocate.3
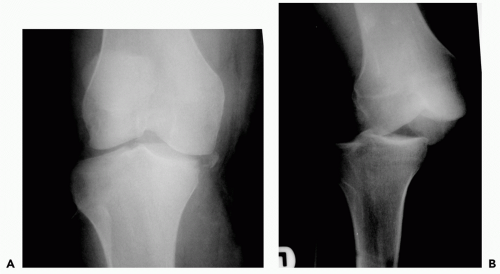
The next most common dislocation is the posterior dislocation (see Fig. 2). Posterior knee dislocations result from a direct force striking the anterior tibia, driving it posteriorly. This occurs most commonly with motor vehicle collisions or sports-related injuries when the knee strikes the dashboard or an oncoming opponent.
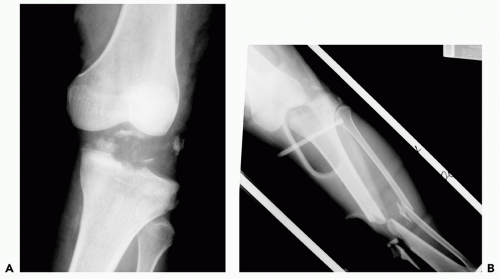
Medial and lateral dislocations (see Fig. 3) are much less common. These occur when a force is directed from
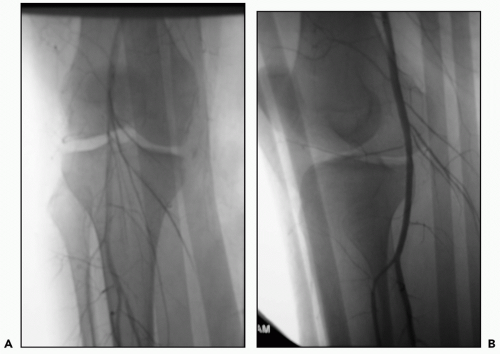
the side causing a varus (toward the midline) or valgus (away from the midline) stress across the knee. Neurologic injury is more likely to occur in lateral knee dislocations as a result of tethering of the peroneal nerve at the fibular head and neck.4 Rotatory dislocations are far less common (see Fig. 4). Rapid twisting or torsion results in rotatory dislocation with or without neurovascular injury. It is almost always accompanied by protrusion of the medial femoral condyle through the medial retinaculum and capsule. With enough twisting, invagination of the MCL into the joint results in incarceration and trapping (buttonholing effect) of the medial femoral condyle and an irreducible knee dislocation.5,6,7,8,9 The invagination of the joint capsule and prominence of the femoral condyle medially produce a dimple in the skin at the joint line which can clinically help distinguish this kind of injury from other dislocations.10
the side causing a varus (toward the midline) or valgus (away from the midline) stress across the knee. Neurologic injury is more likely to occur in lateral knee dislocations as a result of tethering of the peroneal nerve at the fibular head and neck.4 Rotatory dislocations are far less common (see Fig. 4). Rapid twisting or torsion results in rotatory dislocation with or without neurovascular injury. It is almost always accompanied by protrusion of the medial femoral condyle through the medial retinaculum and capsule. With enough twisting, invagination of the MCL into the joint results in incarceration and trapping (buttonholing effect) of the medial femoral condyle and an irreducible knee dislocation.5,6,7,8,9 The invagination of the joint capsule and prominence of the femoral condyle medially produce a dimple in the skin at the joint line which can clinically help distinguish this kind of injury from other dislocations.10
The condition of the static (ligamentous, bony, meniscal, and cartilaginous structures) and the dynamic (muscles) stabilizers determine the stability of the knee. The ligamentous structures include the ACL, PCL, MCL, LCL, and PLC. The PLC is made up of the iliotibial band, popliteus complex, the middle third of the lateral capsular ligament, the fabellofibular ligament, the arcuate ligament, the posterior horn of the lateral meniscus, the lateral coronary ligament, and the posterolateral portion of the joint capsule. In order for the knee to dislocate many of these structures must be disrupted.
Typically, for anterior or posterior dislocations, both ACLs and PCLs are disrupted. However, there are many reports in the literature in which only one of the cruciates is torn.4,11,12,13 The ACL is always disrupted with an anterior dislocation and the PCL with a posterior dislocation. When a valgus stress is applied the MCL will be disrupted. When a varus stress is applied the LCL will be disrupted.
Other more comprehensive classification schemes exist describing the combinations of ligamentous injury rather than the direction of displacement. However, they relate more to the planning of ligamentous reconstruction and are beyond the scope of this chapter.
Fractures of the femoral condyles and tibial plateau need to be recognized because they can significantly influence knee stability in the face of intact ligamentous structures. Injury to articular and/or meniscal cartilage also occurs; however, these injuries have less impact on stability and are more important for the subsequent development of posttraumatic osteoarthritis.
EVALUATION AND ACUTE MANAGEMENT
Once a knee dislocation is identified it should be reduced as soon as possible; however, a quick neurovascular examination should precede the reduction maneuver. The posterior tibial artery and dorsalis pedis artery should be palpated. If the pulses cannot be palpated secondary to vasospasm, hypotension, edema, or soft tissue defects, then Doppler examination should be performed to ensure adequate perfusion to the distal extremity. The sensorimotor status of the deep and superficial peroneal nerves and tibial nerve should be evaluated and documented. Nerve damage occurs with an incidence of 16% to 35% of all knee dislocations.14,15,16,17 The peroneal nerve innervates ankle and toe dorsiflexors,
whereas the tibial nerve innervates ankle and toe plantar flexors.
whereas the tibial nerve innervates ankle and toe plantar flexors.
After the neurovascular status is confirmed and documented, reduction can be performed under conscious sedation if the patient’s status permits. This can be successfully accomplished in most of the patients with gentle longitudinal traction and a force is directed opposite the direction of dislocation by an assistant. In grossly unstable knees, particularly in an unconscious or sedated/relaxed patient, care must be taken to avoid excessive force and overdistraction of the joint and neurovascular structures.
Radiographic evaluation of the knee should be performed to identify the type of dislocation and any fractures about the femur and tibia. However, if a dislocation is identified, neurovascular examination and reduction/immobilization should be performed before any radiographic examination to avoid unnecessary prolonged kinking, traction, or pressure on the neurovascular structures.
The paramount concern in a patient with a knee dislocation is the vascular status of the extremity. Therefore, following reduction the pulses should be palpated for symmetry and an Ankle Brachial Index (ABI) should be performed to rule out occult vascular injury in the case of palpable pulses. An ABI is performed by placing a blood pressure cuff about the calf and using the Doppler to detect the pulse at the ankle or foot. The systolic pressure is recorded when a Doppler-able pulse returns. This is repeated on the ipsilateral upper extremity, and the ratio of the ankle systolic pressure to the brachial systolic pressure is calculated. Normally, the ABI should be > 1, with anything below 0.9 highly suggestive of an occult vascular injury (i.e., an intimal tear or flap).18
If the knee is irreducible and the pulse is absent or asymmetric with an abnormal ABI, then emergent operative reduction should be undertaken followed by repetition of ABI. If the ABI or physical examination suggests a vascular injury despite anatomic reduction, then contrast arteriography is recommended to investigate vascular structures.
The incidence of an associated popliteal artery injury ranges from 7% to 80%.2,19,20,21,22,23 If a vascular injury has not been addressed within the first 6 to 8 hours, the amputation rate has been reported to be as high as 86%.2 Because of the high incidence of associated vascular injury and its catastrophic sequelae, many sources in the past have recommended arteriography for all patients with knee dislocations.21,22,23 However, more recent publications by Stannard and Mills have shown the reliability of both the physical examination and ABI in treating the patient with a knee dislocation. Provided the patient was admitted for close observation and the physical examination or ABI remained within normal limits, no vascular complications were encountered. The complication rate of arteriography ranges from 2% to 3% for allergic reactions, vasculitis, thrombosis, and renal failure; however, in the patient with an abnormal physical examination or ABI this does not outweigh the potential benefits.24,25,26 If any abnormality is noted on arteriography other than vasospasm, vascular consultation is required.
If the pulses are normal and an ABI of >0.9 is found, further evaluation of the ligamentous structures can be attempted using physical examination to assess damage. In the acute setting it can be difficult to perform these tests on an alert patient because of discomfort. The examination is based on stress-testing the stability of the ligamentous structures:
ACL: The Lachman test is done with the patient’s knee held at 20 to 30 degrees of flexion. The patient’s femur is stabilized with one hand while the other hand attempts to translate the tibia anteriorly. The degree of laxity and the firmness of the endpoint are compared to the contralateral knee. This is the most sensitive clinical examination for testing the ACL.27
PCL: The posterior drawer test is used to assess the PCL. This is done by flexing the patient’s knee up to 90 degrees. A posteriorly directed force is then applied to the proximal tibia. The degree of laxity and the endpoint should be assessed and compared to the contralateral side. This is the most sensitive test for the PCL.
MCL: The MCL is assessed with the knee at 30 degrees of flexion with a valgus stress applied to the knee. If the knee is stressed in full extension, the ACL and PCL help to stabilize against a valgus stress and may give a false-negative examination. At 30 degrees of flexion, these ligaments no longer help stabilize against the valgus stress. If the medial joint space opens then the MCL is likely incompetent.
LCL: The LCL is tested at 30 degrees of flexion for the same reason as the MCL. A varus stress is applied to the knee. If the lateral joint space opens then the LCL is likely incompetent.
PLC: The PLC is assessed using the posterior drawer test at both 30 degrees and 90 degrees of flexion. If there is increased laxity at 30 degrees when compared to 90 degrees, a PLC injury should be considered. The dial test is also used to test the PLC. The tibia is externally rotated at 30 degrees of knee flexion and at 90 degrees of flexion. If there is increased rotation at 30 degrees but not 90 degrees then there is an isolated PLC injury. If there is laxity at both 30 degrees and 90 degrees then there is a PLC injury and a PCL tear.28
After the physical examination is completed, the patient should be placed in a long leg splint or a knee immobilizer. Radiographs should be repeated once the knee is immobilized in order to ensure that the knee joint remains reduced in the splint. If the knee joint does not remain reduced in the splint then the patient should be taken to the operating room for application of a spanning external fixator to maintain a concentric reduction and prevent posterior subluxation.
After satisfactory perfusion is assured and the knee joint is reduced and stabilized, MRI should be performed to
assess the extent of soft tissue or ligamentous injury.29,30 MRI has been found to be 85% to 100% accurate in predicting the extent of soft tissue injury.31
assess the extent of soft tissue or ligamentous injury.29,30 MRI has been found to be 85% to 100% accurate in predicting the extent of soft tissue injury.31
The patient should subsequently be admitted for 24-hour observation and frequent (every 2 hours) neurovascular monitoring for compartment syndrome and changes in vascular status.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree