Soft Tissue Problems Following Total Hip Arthroplasty
Ormonde M. Mahoney
Case Report
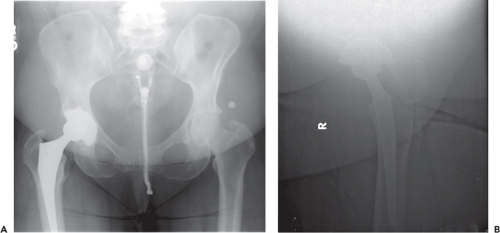
TE is a 64-year-old female who underwent right total hip replacement 3 years earlier. Over the past 6 months the patient has suffered from progressive pain in the ipsilateral groin with active hip flexion; making it difficult to get in and out of the car or to climb stairs. The patient denies any other constitutional problems, fevers or recent infections, and antecedent trauma. Physical examination reveals that the patient walks without a notable limp. There is no tenderness over the trochanter, but the patient complains of discomfort with pressure placed over the anterior hip. Passive hip motion is unrestricted compared to the contralateral hip, however, the patient complains of pain with any attempt at active hip flexion in the supine or seated positions. Radiographs pictured here reveal a well-fixed cementless total hip arthroplasty in satisfactory position (Fig. 85.1A and B).
Persistent pain after total hip replacement is not as rare as we would like to believe. In fact, in a Danish population-based study, Nikolajsen et al. (1) noted clinically significant postarthroplasty pain in 12% of total hip patients. Many of these dissatisfied patients may have soft tissue problems like the patient described in this text. The presenting complaints and findings depicted here represent one variant of a constellation of potential soft tissue problems that can be encountered after successful total hip replacement. The evaluation of these problems begins first with the elimination of more potentially serious problems like loosening or infection and referred pain from spine pathology. A thorough history directed at establishing the onset, location, character, timing, and associated symptoms or complaints is essential. A vague history of antecedent trauma should not be considered adequate to rule out infection since patients will often draw associations between the onset of pain and a preceding event
like a slight miss-step. Recent bladder infections or dental problems, with or without periods of feverishness or sweats, should raise suspicions of more serious problems. Constant, progressive pain represents infection until proven otherwise and the examiner should have a low threshold for arthrocentesis in these patients. Other causes of progressive pain like metallosis and corrosion-related synovitis must also be considered. Plain radiographs are usually quite effective at identifying loosening.
like a slight miss-step. Recent bladder infections or dental problems, with or without periods of feverishness or sweats, should raise suspicions of more serious problems. Constant, progressive pain represents infection until proven otherwise and the examiner should have a low threshold for arthrocentesis in these patients. Other causes of progressive pain like metallosis and corrosion-related synovitis must also be considered. Plain radiographs are usually quite effective at identifying loosening.
Soft tissue problems around hip prostheses are almost always associated with specific activities or movements. The importance of observation of gait, evaluation of motion range, and deep tissue palpation cannot be underestimated in these cases.
Trochanteric Bursitis
Pain centered over the greater trochanteric bursa is probably the most common soft tissue complication seen after total hip arthroplasty, with incidences reported in 4% to 17% of patients (2). Historically, this phenomenon was thought to be secondary to an inflammatory process involving the bursa itself, but this etiology has recently been questioned and the presence of abductor tendinopathy seen in magnetic resonance studies of many cases may be a more plausible explanation (3,4,5). Multiple technical factors have been implicated as contributors to the occurrence of the problem. It appears to be more common when a lateral approach is used, but this observation remains controversial (6). Most authors do agree that the biggest contributors are limb lengthening and increases in offset of a centimeter or more (2,6). The problem is more common in females and usually manifests itself between 8 and 24 weeks post surgery. Most patients initially complain of pain at night when they roll over onto the operated hip, but as the symptoms progress, they experience pain on weight bearing and an associated limp. This presentation of initial pain in bed that progresses to more diffuse lateral hip and thigh pain on weight bearing can be helpful in eliminating other more serious causes of painful total hip replacements.
Treatment is primarily conservative, consisting of several weeks of nonsteroidal anti-inflammatory and physical therapy. In cases where pain is substantial and in cases where therapy is not effective corticosteroid injections are recommended. This treatment is often effective with success rates reported in the 40% to 80% range (6). In the majority of patients only one injection is required. In a review of 24 articles on the management of trochanteric bursitis, Lustenburger et al. (7) reported two studies describing the use of low-energy shock wave therapy as an additional treatment option with results at least equivalent to other nonoperative methods. Surgical treatment should be considered only after failure of multiple injections and physical therapy. The most common options are centered on open release of the iliotibial band and the fascia lata, removal or debridement of the trochanteric bursa along with smoothing any notable bony prominences, or in severe cases a trochanteric reduction osteotomy (8). Recently, a number of authors have documented success using endoscopic bursectomy (9,10,11).
Abductor Muscle Tears
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree