Chapter 16 Soft Tissue Manipulation in Complementary/Alternative Medicine
Modern health care practice has begun to embrace the concept of complementary/alternative medicine (CAM) as an important approach for treating illness and promoting health and wellness. Other terms that encompass similar ideas are holistic medicine and integrative medicine. Since the 1980s, there has been a growing acceptance of the efficacy of CAM as an alternative to orthodox medical practice. Many of the treatment concepts that fall into the category of CAM have their origins in traditional Eastern medicine. Systems of care such as acupuncture and acupressure are good examples. In contrast, some more modern concepts also fit into this category. These techniques include myofascial release and rolfing structural integration. This chapter briefly considers several treatment concepts that are good examples of both ancient and modern specialized systems of soft tissue manipulation. They are sometimes referred to as bodywork systems (McPartland & Miller, 1999; Oschman, 1997).
Further evidence of the growing interest in CAM can be seen in the increasing support from many national research granting agencies. Many of these organizations have been promoting vigorous research into the efficacy and use of techniques such as acupuncture, acupressure, shiatsu, reflexology, herbal medicine, moxibustion, and homeopathy (Vickers, 1995). Surveys of Western medical practitioners in the Netherlands, Great Britain, New Zealand, the United States, and Canada have highlighted a growing interest in and willingness to accept CAM (Carpenter & Neal, 2005; Eisenberg et al., 1993; Hadley, 1988; Lynoe & Svensson, 1992; Micozzi, 1996; Verhoef & Sutherland, 1995; Wharton & Lewith, 1986). This is particularly the case in the management of chronic pain and musculoskeletal dysfunction (Sarac & Gur, 2006). The most widely used techniques are those that appear to be more efficacious, such as acupuncture, the deep pressure and stretching employed in acupressure, shiatsu, myofascial release, and rolfing structural integration.
Although a detailed discussion of all of these methods is well beyond the scope of this book, a number of these techniques are briefly explored here, especially those in which soft tissue manipulation is an important part of the treatment concept. These techniques include myofascial release, reflexology, trigger point massage, rolfing structural integration, and a brief discussion of the lesser-known techniques of point percussion therapy and craniosacral therapy. Chapter 17 reviews some more ancient systems of massage, especially those with an Eastern heritage. These include acupressure, shiatsu, traditional Oriental massage, and Huna (Hawaiian) massage.
The proliferation of complementary/alternative practitioners, both within and outside of the established health care systems, is evidence of dissatisfaction with the orthodox medical approach. In general, modern (orthodox) medicine has focused on treating illness rather than promoting wellness and preventing disease. In contrast, much of the focus of CAM is directed toward promoting wellness and preventing disease, without the use of drugs or surgery (Fritz, 2004; Jahnke, 1985) and detoxification (Cassar, 1999). Although these techniques are popular, they are not without risk. Many of the complementary/alternative techniques produce their beneficial outcomes by invoking a reflex autonomic effect. It is important to note that when autonomic responses are elicited—for example, with connective tissue massage (CTM), acupressure, shiatsu, reflexology, trigger point, and myofascial techniques—problems can arise. Although most techniques are perfectly safe, contraindications need to be taken seriously. These may include pregnancy, serious cardiopulmonary conditions, and psychological problems such as panic disorder. The safe and effective practice of any of the complementary/alternative therapies requires proper training and certification where appropriate.
Many of the complementary/alternative therapies incorporate soft tissue manipulation techniques (massage) as a major part of their practice (Westland, 1996), especially to counterbalance the negative effects of gravity on the body. The ever-present force of gravity coupled with aging and a stressful modern lifestyle place a significant burden on the musculoskeletal system in just about everyone. Muscles, tendons, fascia, joint capsules, and ligaments often become tight (shortened), resulting in postural malalignment and movement dysfunction. The net result is often chronic pain and a host of other physical and psychological symptoms. In contrast, many of these issues can be significantly reduced, if not eliminated, by restoring the correct structural integrity (valance) to the affected body system(s). This concept will be a familiar theme in many of the treatment systems described in this chapter and Chapter 17.
MYOFASCIAL RELEASE TECHNIQUES
Myofascial release is a relatively new concept in the larger picture of Western medical thought; however, techniques similar to it can be found in classical Eastern health and medical writings. As its name suggests, the techniques of myofascial release refer to a specialized system of prolonged manual stretching of the fascial tissues of the body, to the point where there is a release of tension. This release of tension is felt by the therapist and implies a slight lengthening of the fascial tissues (J.F. Barnes, 1997; M.F. Barnes, 1997a; M.F. Barnes, 1997b). It should be emphasized that the stretching technique is a subtle one. Tension is applied slowly and gently and is released in a similar manner. There is some evidence to suggest that fascia may have an ability to contract in a way similar to smooth muscle, and, if so, it may have the ability to relax and thereby lengthen (Schleip et al., 2005).
Fascia is a much-neglected tissue of the body, often being thought of as simply a connective tissue scaffolding associated with muscles and tendons. In fact, it is an extremely important whole-body network, on a par with the vascular or nervous system. Fascial tissue does indeed provide a scaffold-like net to every type of tissue in the body, even down to the extracellular level. As such, the fascial system connects all parts of the body together with a continuous web of tissue. There is a tradition of describing different body systems in a particular order. For example, there is a tendency to think of the bony skeleton as the foundation of the body, with all the other structures attached to it or contained by it. Alternatively, bones can be rightly considered as rigid spacers entrapped in a fascial net. One might imagine a classic circus tent, where the canvas material and rigging are held up by the giant wooden masts. Without the tent poles, the material of the tent has no defined shape and will not function properly on its own.
Fascia is a type of connective tissue that has three layers: superficial, potential space, and deep. It has important biomechanical properties and greatly assists in maintaining muscle force. The interconnectedness of the fascial system throughout the body is extremely important, because many acute and chronic musculoskeletal problems have their origins in this tissue. Excessive strain, poor ergonomic environments, trauma, and abnormal postural alignment are among the common causes of strain of the fascial system. This strain leads to a type of contracture (tightness), which in turn causes pain and restricted movements. In fact, a host of symptoms can be caused in many different body parts as the long-term result of restricted fascial movement. Whereas a fasciotomy to release tight fascia can result in a 15% loss of muscle strength, myofascial release techniques reduce constriction and pain without compromising muscle strength (Manheim, 2001). Symptomatic relief of the pain produced by this situation obviously will not cure the underlying tightness somewhere in the fascia. A treatment technique that is directly applied to the fascia is likely to be more effective at producing a long-term solution. For example, myofascial release techniques, in conjunction with trigger point stimulation, can be extremely important to the long-term success of therapy because the fascia tightens and shortens with inflammation (as the potential space swells), heals slowly (because of a poor blood supply), and is a pain focus (because of its abundant nerve supply).
Technique
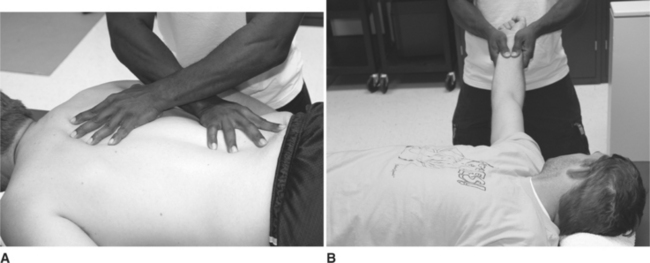
A wide variety of specific techniques can be used, depending on the body part to be treated. For example, on the posterior trunk, the therapist’s hands can be placed flat on the patient’s back, whereas on the limbs, the therapist’s hands may lightly grasp around the patient’s tissues. Figure 16-1 illustrates these two different types of hand positions. There are, of course, many variations, depending on the areas to be treated.
In Figure 16-1, A, the therapist gradually applies pressure to the patient’s skin and underlying tissues while simultaneously stretching them apart. The therapist achieves this result by pushing his or her hands apart in opposite directions. The therapist’s right hand pushes toward the patient’s right hip while the therapist’s left hand applies pressure toward the patient’s left shoulder. Good body mechanics are essential during this technique, especially because it can take several minutes to complete. Wherever possible, the therapist should use his or her own body weight to provide the pressure needed during the technique. As the tissues are stretched, some movement (lengthening) will occur, but eventually, a block to further stretching will be felt. At this point, pressure is maintained for as long as it takes for the tissues to release the tension. The therapist will feel this release of tension as the resistance to the stretching gives. This can typically take anywhere from 90 to 120 seconds to happen, although sometimes it will occur sooner. As the tissue tension is released, the therapist’s hands remain in the same position but continue to apply a stretching tension at the new tissue length. In this manner, the tissues are stretched out as the therapist follows the releasing of the tissues. It may take several applications of tension to chase the tight areas of fascia in the tissues. Once again, it must be emphasized that the technique is a subtle one. Pressure is gentle but firm. The therapist’s hands are feeling their way into the tight areas.
Figure 16-1, B, illustrates a different technique. In this case, a gentle traction force is applied to the entire upper limb. As the limb elongates in a telescopic-like manner, a block to further movement is felt, at which point the tension is maintained until the tissues release. Further tension is applied at the new length. Once again, this process is repeated several times until a more normal tissue length has been achieved.
Myofascial release is a specialized technique, requiring proper training and experience. As with many other forms of soft tissue manipulation, it does not replace other rehabilitation procedures, but rather it compliments them in an important way. Myofascial release allows the tissues to return to their normal physiological state (or close to it) so that other techniques, such as therapeutic exercise and manual mobilization, can be maximally effective. Manheim (2001) has provided postural assessment methods and a detailed description of techniques of myofascial release. Other authors have provided a wide range of descriptions of the technique and its use (Mock, 1997a, 1997b, 1998; Morris, 1999: Shea & Keyworth, 1997; Stone, 2000; Whalen, 1999).
The role of myoglobin in myofascial pain and its dispersion (and associated pain relief) by massage techniques has been studied (Brendstrup et al., 1957; Danneskiold-Samsøe et al., 1982, 1986; Krusen et al., 1965; Simons, 1990). Ronald Melzack (1981) has reported on the similarity of the neural mechanisms involved in the relief of pain produced by acupuncture, acupressure, ice massage, and trigger point stimulation. This hyperstimulation analgesia is one of the oldest recorded remedies and should become a useful technique for relieving pain of musculoskeletal lesions, especially when chronic conditions have affected posture, gait, and other activities (Ehrett, 1988; Friction et al., 1985; Friedmann, 1989; Ingber, 1989; Kine & Warfield, 1986). The presence of type C nociceptors and adaptive shortening in the muscles and fascia contribute to the pain of chronic disorders (Reynolds, 1981; Rubin, 1981). Mobilization of peripheral nerves and manipulation (stretching and releasing) of the fascia that is continuous with nerve roots relieve pain and help to restore function (Cantu & Grodin, 2001).
TRIGGER POINT Therapy
A trigger point—also called a myofascial trigger point (MTrP)—is a sensitive spot on the body surface that, when stimulated, causes local and referred pain elsewhere in the body. The stimulated spot literally triggers a painful response somewhere else in the body—hence its name. Depending on the location of the trigger point, it may also cause a local, painful muscle twitch. Myofascial trigger points are commonly found in taut bands, which are often felt as contraction knots within a muscle. Both local twitch responses and the referred pain are mediated through a spinal cord reflex. Many of these sensitive spots occur in the myofascial structures of the body and are often the focal points of the concept of a myofascial pain syndrome. This syndrome is often confused with fibromyalgia and is characterized by musculoskeletal pain that originates from a hyperirritable spot (Brendstrup et al., 1957; Danneskiold-Samsøe et al., 1982, 1986; Friction et al., 1985; Hey & Helewa, 1994; Kine & Warfield, 1986; Kostopoulos & Rizopoulos, 2001; Reynolds, 1981; Rubin, 1981; Simons, 1990; Waylonis et al., 1988; Yunus et al., 1988).
These trigger points—called myofascial triggers by Janet Travell and myodysneuric points by R. Gutstein—are sensitive points or areas that produce pain some distance away (Travell, 1981; Travell & Simons, 1983, 1992).
An active trigger point may be found in tight or taut fascial or muscular bands. It may be in the skin (scar tissue), a ligament, a tendon, or even deeper at the joint capsule or periosteal level. Knowledge of the location of acupuncture points associated with pain may help to locate an active trigger point, as about 70% of both points are located at the same site (Hong, 2000; Melzack, 1981). Active trigger points often produce a localized sharp pain that may radiate to the referred, or target, area some distance away. Any or all of the signs or phenomena in the following list may be associated with manual or electrical stimulation of an active trigger point:
Figure 16-2 illustrates the sites of common trigger points and associated muscle groups. The referred pain and any motor, sensory, or autonomic responses are ameliorated by desensitizing (releasing) the active primary point(s). Together with appropriate myofascial release techniques (discussed earlier), the treatment of active trigger points is an important adjunct to the management of chronic musculoskeletal conditions (Laing et al., 1973; Lundberg et al., 1984). In addition, careful palpation and awareness of any associated acupuncture points can assist in the assessment of related soft tissues (Fischer, 1988; Goldenberg, 1989).
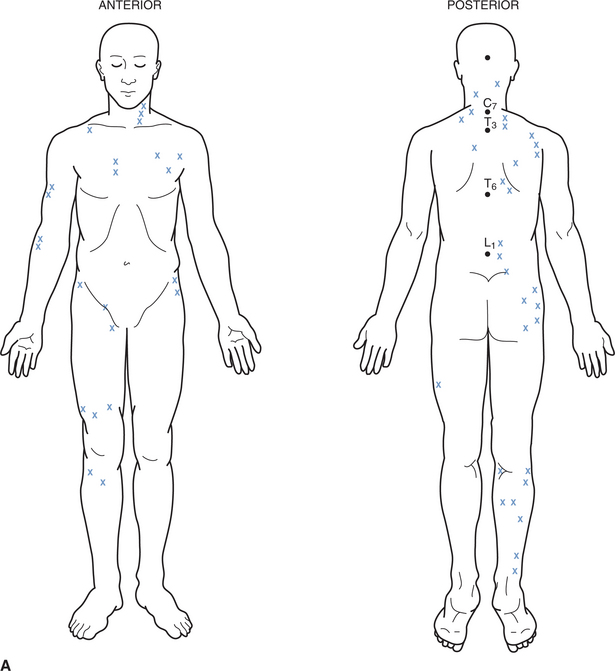
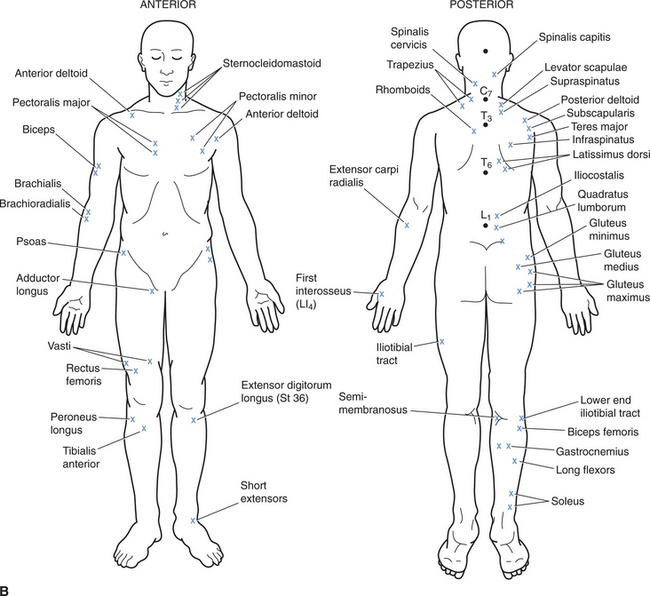
Figure 16-2 Common Trigger Points
A, The common sites of trigger points in the body. B, The muscles associated with these points.
An active trigger point can be desensitized using a sustained pressure. There are several ways in which mechanical pressure may be given, including the use of one finger, two or more fingers, a knuckle, an elbow, or by strumming (as in applying connective tissue massage) with the fingers extended (Kostopoulos & Rizopoulos, 2001; Kovacs et al., 2000; Manheim, 2001; Peppard, 1983; Travell & Simons, 1983).
Stimulation Technique
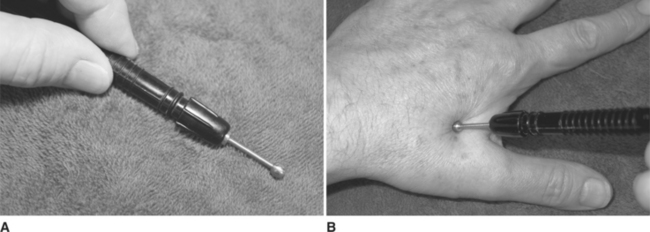
Active trigger points can be located in a number of ways, including direct digital palpation by the therapist (or patient, where appropriate) or with the use of trigger point location devices. These devices are usually small, handheld instruments that are used to apply a small voltage to the skin and tissues. The device emits a low continuous tone when applied to the skin a short distance (6 to 8 inches) away from an active point. The probe is then moved toward the trigger point. When located directly over the point, the tone changes to a high-pitched note and an indicator light may also illuminate. In effect, the device has located the area of lowered skin resistance associated with an active trigger point. Ohm’s law predicts that when the same voltage is applied to a lowered resistance, a greater current will flow, and this is the operating principle for these devices. Although these devices can be useful, they do have limitations, not the least of which is the fact that they are usually removed in order for direct digital pressure to be applied. A much more useful device is a ball-headed hand probe. These devices allow pressure to be concentrated into a small area without puncturing the skin. They are ideal for manual trigger/acupuncture point stimulation and may allow the patient to self-administer treatment at home. These probes are also ideal for electrical stimulation of trigger points. Figure 16-3 illustrates such a device.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree