Soft Tissue Management of Ankle Fractures and Use of the Gracilis Muscle Flap
S. Andrew Sems
Matthew DeOrio
Steven L. Moran
Soft tissue management of injuries around the distal tibia and ankle region will often dictate and drive the timing and methods of definitive fixation. Injuries in this region vary from low energy ankle fractures to high energy tibial pilon fractures. The soft tissue injuries often reflect the amount of energy that was involved in creating the bony injury. Regardless of the radiographic appearance of the fractures, certain initial treatment principles hold true for both low and high energy injuries. Early fracture reduction to restore limb alignment, rotation,
and appropriate limb length combined with fracture immobilization will allow sooner resolution of soft tissue swelling and impairment that might otherwise prevent or delay early internal fixation.
and appropriate limb length combined with fracture immobilization will allow sooner resolution of soft tissue swelling and impairment that might otherwise prevent or delay early internal fixation.
Ankle Fractures
Indications/Contraindications
Operative treatment is generally recommended for all unstable ankle fractures in which the talus is unable to be maintained in a position beneath the tibial plafond by closed reduction. Nonoperative management is appropriate for stable ankle fractures in which there is no lateral subluxation of the talus within the ankle mortise.
Comorbidities
Open reduction and internal fixation can generally be safely performed on most patients regardless of associated comorbidities. In patients with severe peripheral vascular disease, preoperative transcutaneous pressure oximetry measurements should be obtained to assess the likelihood of the patient healing the surgical wounds. TcPO2s less than 30 mm Hg have a higher risk of wound failure and fracture nonunion. Involving Vascular Medicine to assist with maximizing lower extremity perfusion is reasonable if vascular disease is a concern. The implications of insulin dependent diabetes mellitus and peripheral neuropathy should also be considered when determining operative versus nonoperative treatment but are not contraindications to surgery. Postoperative soft tissue management should be modified in patients with high risks of developing wound complications. Longer periods of cast immobilization and protected weight bearing may be indicated for patients with these comorbidities.
Nonoperative management of fractures in the nonambulatory patient is reasonable provided the fracture does not cause deformity which would result in subsequent skin breakdown. Modified techniques of internal fixation in patients who are nonambulatory may be utilized in order to maintain the anatomy around the ankle joint to prevent soft tissue compromise.
Preoperative Planning
Plain radiographs should be obtained in all patients with unstable ankle fractures prior to surgical intervention. Anteroposterior (AP), mortise, and lateral views are necessary to assess the fracture orientation. Ankle fractures tend to include the medial malleolus, lateral malleolus, and occasionally, the posterior malleolus. Recognition of the three-dimensional plane in which each fracture occurs is important so that surgical incisions are placed appropriately and the correct internal fixation is selected. While computed tomography is utilized more often for pilon type tibial fractures, it may be used if there is not a clear understanding of the fracture pattern.
Surgical approach selection for treatment of ankle fractures depends on the location of the fractures and the quality of the surrounding tissues. Fractures of the medial malleolus are typically approached with an anteromedial incision overlying the medial malleolus. This incision can be adjusted anteriorly or posteriorly depending on the size and orientation of the medial malleolar fragment. Fractures which include both the anterior and posterior caliculus may require slight posterior adjustment of the incision while fractures that only involve the anterior caliculus may be approached through a more anteromedial incision. Fibular fractures are typically treated with a direct lateral approach, although a posterolateral approach is useful for fibula fractures which occur in the coronal plane or in cases of associated posterior malleolus fragments that may be addressed through this same incision.
The timing of surgery is dictated by the state of the soft tissue envelope. For ankle fractures, immediate fixation within the first 24 to 48 hours is feasible so long as the swelling will not compromise wound healing. Patients who present to the clinic or emergency department with ankle fractures within 48 hours from injury can often be treated with immediate open reduction and internal fixation prior to the onset of the maximal amount of soft tissue swelling. Surgery should be delayed when soft issue is so edematous that the surgeon is unable to create skin wrinkles by gently pinching the skin over both the medial and lateral malleolus. Open fractures require immediate surgical intervention for debridement of all contaminated soft tissues. Antibiotic cement bead pouches or Vacuum Assisted Closure (VAC) devices may be used until definitive fixation or final wound closure. External fixation may be necessary to restore length, alignment, and rotation of both the soft tissues and the bone prior to definitive internal fixation.
Ankle fractures should ideally be treated within 3 weeks of injury prior to early callus formation, which can create significant difficulty in fracture reduction. Patients who present in the first week following an ankle fracture and whose soft tissues are not amenable to immediate surgical fixation should be treated with a Robert Jones type compressive dressing with plaster immobilization. These patients should be encouraged to maintain strict elevation of their limb at all times. They are then seen back in
the clinic or preoperative area approximately 7 to 10 days after their injury for soft tissue evaluation prior to surgical intervention. This dressing should be taken down and the skin should be evaluated prior to any type of anesthetic administration. In patients who are admitted to the hospital, sequential compression boots can be applied to the foot prior to the application of the Robert Jones dressing. These pneumatic boots are usually well tolerated so long as they do not extend up past the ankle.
the clinic or preoperative area approximately 7 to 10 days after their injury for soft tissue evaluation prior to surgical intervention. This dressing should be taken down and the skin should be evaluated prior to any type of anesthetic administration. In patients who are admitted to the hospital, sequential compression boots can be applied to the foot prior to the application of the Robert Jones dressing. These pneumatic boots are usually well tolerated so long as they do not extend up past the ankle.
Surgery
Medial/Lateral Approaches
Patient Positioning
The patient is positioned supine on a radiolucent table with a thigh high pneumatic tourniquet and a small bump (towel) placed under the ipsilateral hip to prevent excessive external rotation of the limb. The bump placed underneath the hip area should be adjusted so that the foot points vertically when in its resting position. A foam block or bump of towels can be utilized underneath the leg and ankle area so as to elevate the operative limb from the nonoperative limb. This facilitates obtaining lateral radiographs without manipulation of the operative leg. The intraoperative fluoroscopy unit is brought in from the contralateral side, and it is positioned perpendicular to the long axis of the patient.
Prophylactic antibiotics are utilized for internal fixation of ankle fractures. They should be administered prior to inflation of the tourniquet. Once the tourniquet is inflated, it should be maintained as long as necessary, but not for more than 2 hours. If it is impossible to complete the procedure in the allotted 2 hours, the tourniquet should be deflated and hemostasis should be obtained, and the procedure should be completed without the aid of a tourniquet. If small vessel bleeding continues to be an issue, consider moving the operative bed into a Trendelenburg position and asking the anesthesiologist to decrease the systolic blood pressure within safe limits.
Technique
Anatomic Landmarks—Medial Approach
Palpate the medial malleolus to define the location of the anterior aspect of the anterior caliculus, the posterior aspect of the posterior caliculus, as well as the fracture location. The leg should be palpated to determine the longitudinal axis of the tibia.
Incision and Surgical Approach
The incision is made along the midlateral axis of the distal tibia. Beyond the tip of the medial malleolus the incision may be slightly curved anteriorly (Fig. 32-1). Be aware that excessive curvature of the incision may create difficulties in placing internal fixation in the medial malleolar fragment. Dissection should be carried through the skin and subcutaneous and hemostasis obtained as this is performed (Fig. 32-2). Care should be taken to preserve and protect the saphenous vein and nerve throughout the case. In this location, the saphenous vein is often very subcutaneous and an aggressive skin incision may lacerate the vein. With the saphenous
vein and nerve protected, the medial malleolar fragment can be retracted distally with sharp bone hooks to allow inspection of the ankle joint (Fig. 32-3). A 15 blade, used to elevate the periosteum along the fracture edges, can be utilized to ensure that the fracture is reduced in an anatomic position. Preservation of the soft tissue and minimal periosteal stripping is recommended. Following internal fixation, the subcutaneous tissue can be closed using a 2-0 absorbable suture, and the skin closed with a nonabsorbable monofilament suture (Fig. 32-4).
vein and nerve protected, the medial malleolar fragment can be retracted distally with sharp bone hooks to allow inspection of the ankle joint (Fig. 32-3). A 15 blade, used to elevate the periosteum along the fracture edges, can be utilized to ensure that the fracture is reduced in an anatomic position. Preservation of the soft tissue and minimal periosteal stripping is recommended. Following internal fixation, the subcutaneous tissue can be closed using a 2-0 absorbable suture, and the skin closed with a nonabsorbable monofilament suture (Fig. 32-4).
 FIGURE 32-1 The incision is made along the mid-lateral axis of the distal tibia, curving anteriorly beyond the tip of the medial malleolus. |
 FIGURE 32-2 Exposure of the medial malleolar fracture line prior to elevation of the periosteum along the fracture edges. |
Lateral Approach—Lateral Malleolar Fixation
The direct lateral approach to the fibula allows placement of fixation along the lateral aspect of the fibula. This incision is positioned in line with the longitudinal axis of the fibula and may be curved anterior distally to allow access for reduction of a Chaput-Tillaux fragment (Fig. 32-5). If plate fixation along the posterior aspect of the fibula is desired, such as in a situation when an anti-glide plate is used, rather than committing excessive soft tissue stripping via a direct lateral approach, the incision can be adjusted posteriorly. The superficial peroneal nerve may cross the surgical approach in a subcutaneous location; therefore the skin incision should go no deeper than the skin (Fig. 32-6). Dissection through the subcutaneous tissues should be performed using combinations of sharp and blunt dissection with care to identify and protect the superficial peroneal nerve if encountered. Periosteal elevation at the fracture edges with a 15 blade is recommended to ensure an anatomic reduction of the fibular fracture.
For long spiral oblique fractures in which lag screw only fixation of the fibula is to be used, this incision can be altered with an apex anterior curve along the midportion of the incision. This “wave” in the incision will allow anterior retraction of the soft tissues and appropriate directional placement of lag screws across the fracture site. The same concerns remain with regards to protection of the superficial peroneal nerve when this modification is performed.
Following internal fixation, closure is performed with interrupted 2-0 absorbable sutures in the subcutaneous tissue followed by nonabsorbable monofilament sutures in the skin (Fig. 32-7).
 FIGURE 32-5 The incision is positioned in line with the longitudinal axis of the fibula, curving anteriorly at the distal end to allow access for reduction of a Chaput-Tillaux fragment. |
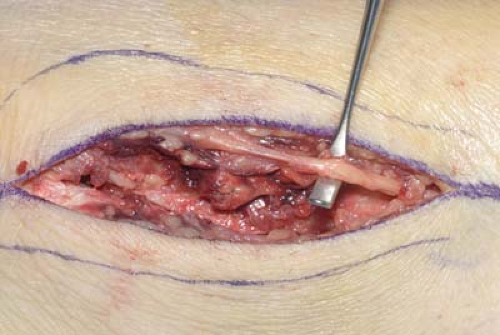 FIGURE 32-6 The superficial peroneal nerve may cross the incision, and care should be taken to identify and protect this structure. |
Posterolateral Approach—Posterior Malleolus Fractures
Patient Positioning
Fractures which require fixation of the posterior malleolus can be approached through a posterolateral incision. Controversy exists regarding the size of the fragment, but internal fixation is typically recommended for fractures which include 20% to 30% of the articular surface. This approach requires the patient to be in either a lateral or prone position (Fig. 32-8). The prone position allows direct visualization and better stabilization of the limb during the approach and is therefore preferred. The patient should be placed on a well-padded radiolucent table with care to be taken to prevent hyperextension of the shoulders and neck. If the arms are placed in an abducted position, care should be taken to avoid direct compression of the ulnar nerve at the cubital tunnel. A thigh high tourniquet is utilized and can be placed prior to prone positioning. Once the patient is in the prone position, they are translated towards the foot of the bed so that the hindfoot is slightly hanging off the end of the bed to aid with reduction and fixation. The C-arm fluoroscopy unit is placed perpendicular to the longitudinal axis of the patient and intraoperative films can be used on the patient’s uninjured side to guarantee symmetry following reduction.
Technique
Palpation of the fibula and Achilles tendon is possible due to the subcutaneous location of these structures. The incision is made midway between the posterior border of the lateral malleolus and the lateral border of the Achilles tendon and will need to extend to the tip of the fibula distally and as far proximally as necessary to obtain visualization of the fibular fracture and the posterior malleolar fracture (Fig. 32-9). The short saphenous vein and sural nerve are located immediately behind the lateral malleolus and the incision is placed posterior and medial to these structures. The deep fascia of the leg is split in line with the incision and the peroneal retinaculum is incised to release the peroneus longus and brevis (Fig. 32-10). The peroneal tendons and muscles are retracted laterally and the flexor hallucis longus is elevated from its origin on the fibula and retracted medially (Fig. 32-11




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree












