Chapter 47 Soft Tissue Coverage Around the Elbow
Presentation, investigation and treatment options – indication for soft tissue cover (causes of defects and how to choose the method of soft tissue cover)
Trauma
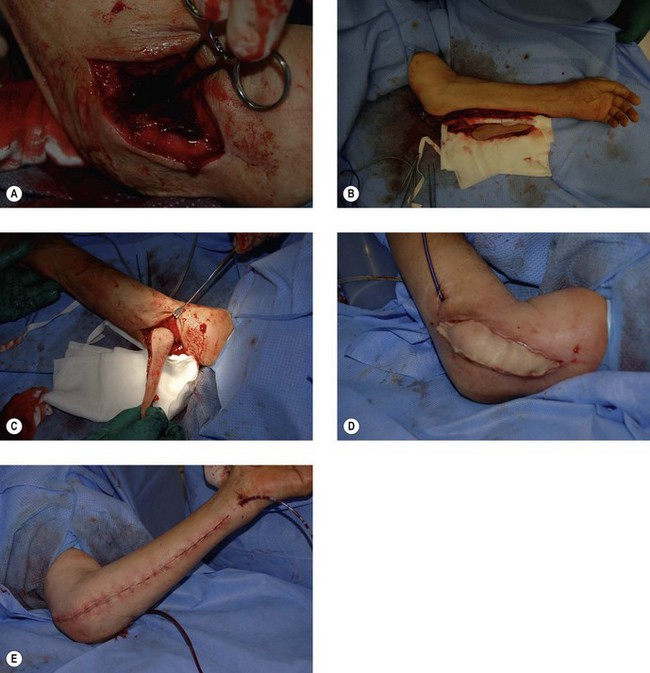
Trauma tends to produce soft tissue defects over the olecranon and, to a lesser extent, the antecubital fossa such as in a displaced open supracondylar fracture (Figs 47.1A,B). Traumatic defects in the ante-cubital fossa less obviously require flap coverage as bone and joint are covered by the thicker layer of soft tissue in this region, and the ability to close the defect by flexing the elbow. However, such an approach may compromise the ability to mobilize the elbow fully and result in an elbow flexion contracture. Most of these antecubital fossa wounds are often initially closed directly but may result in scar contracture necessitating a secondary release.
Olecranon wounds frequently expose the fracture and fixation. Well-vascularized soft tissue cover should be achieved as rapidly as possible to minimize the risk of deep infection and infective non-union with osteomyelitis (Fig. 47.1C). In traumatic wounds in particular, there may be a role for flap coverage of the important or mobile structures with skin grafting of adjacent graftable areas.
Tumour excision
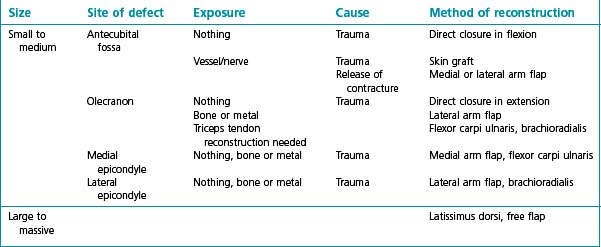
Soft tissue sarcomas around the elbow frequently require flap reconstruction following excision, as skin involvement is common. Fasciocutaneous flaps are favoured as they are more resistant to radiotherapy than muscle and skin graft. The design of the flaps must take into consideration the general principle of postoperative irradiation of the whole surgical field including any in-continuity flap donor site. The design of the donor site must therefore never extend past the surgical field such that circumferential limb radiotherapy becomes necessary. This would lead to marked limb morbidity and distal lymphoedema. Instead, radiation-free corridors should be preserved preferably along the course of a major neurovascular bundle. As a result of this unusual planning restraint, free fasciocutaneous flaps are commonly used in soft tissue reconstruction of this subgroup (Table 47.1).
Surgical techniques and rehabilitation
Local muscle flaps
Brachioradialis
Brachioradialis can be used with or without the overlying skin due to skin perforators that traverse the muscle.1 Only the skin overlying the muscle component of brachioradialis can be safely used. The muscle is supplied by a main artery and accompanying venae comitantes, arising from the radial recurrent artery or in 10% of cases directly from the brachial artery. The pedicle hilum inserts into the deep surface of brachioradialis approximately 10 cm distal to the humeral origin of the muscle, so this can be marked as the pivot point of the flap. This pedicle length of 3–4 cm allows a greater arc of rotation such that the flap can be used to cover the anterior aspect of the elbow, the lateral epicondyle and the olecranon and posterior aspect of the joint. The tendinous portion can be used to reconstruct the triceps.
Extensor carpi radialis longus
As the extensor carpi radialis longus also obtains its main blood supply from the radial recurrent artery, it can be used either with brachioradialis to increase the volume and surface area of the required reconstruction, or as a muscle or myocutaneous flap separately.2 The pedicle hilum inserts into the muscle 10 cm from the origin of the muscle or about 5 cm from the elbow flexion crease, forming the pivot point for transfer of the flap. This flap will cover the anterior, posterior or lateral elbow.
Flexor carpi ulnaris
This is another forearm muscle with a dominant vascular pedicle allowing its dissection and transfer, though flexor carpi ulnaris obtains its blood supply from the ulnar artery rather than the radial.3 The vessel originates 8 cm below the medial epicondyle marking the pivot point of the flap. Skin directly overlying the muscle can be raised with the muscle, supplied by cutaneous trans-muscular perforators. The flexor carpi ulnaris easily covers the antecubital fossa, the medial epicondyle and the medial aspect of the posterior elbow (Fig. 47.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree