Shoulder Labral Tears and Instability
George F. (RICK) Hatch III MD
John G. Costouros MD
Peter J. Millett MD, MSC
Jon J.P. Warner MD
The goal of therapeutic approaches to glenohumeral joint instability is the restoration of anatomy.
The glenohumeral joint is inherently unstable, with the large humeral head articulating with the small and shallow glenoid.
The labrum acts as the anchor point for the capsuloligamentous structures, increases the depth of the glenoid socket, and facilitates the concavity-compression mechanism as the humeral head is compressed in the glenoid during rotator cuff contraction.
Bankart lesions have been considered the primary pathology leading to recurrent anterior dislocation. These lesions were originally described as injuries to the labrum corresponding to the detachment of the anchoring point of the inferior glenohumeral (IGHL) and middle glenohumeral (MGHL) ligaments from the glenoid rim.
Traumatic intra-substance injury of the joint capsule is commonly associated with anterior dislocation. Depending on the magnitude of the anterior shear force, either plastic deformation or a complete tear of the joint capsule can occur.
The most common bony lesion associated with traumatic glenohumeral instability is a compression fracture at the posterolateral margin of the humeral head. Commonly known as a Hill-Sachs lesion, this fracture occurs as the humeral head impacts the glenoid edge during dislocation.
Shoulder instability is categorized on the basis of four criteria: frequency, etiology, degree, and direction.
The degree of instability–dislocation, subluxation, or microinstability–is also important in determining appropriate treatment options.
Many athletes with ligamentous laxity have instability that is primarily posterior in nature. These patients suffer recurrent posterior subluxation and have a history of posterior shoulder pain rather than complaints of rank instability.
A true anteroposterior (AP) view with an axillary lateral view is the minimum radiographic workup necessary for evaluation of an acute dislocation or suspected subluxation.
The goal of treatment in both open and arthroscopic surgery is to restore the labrum to its anatomic attachment site and to establish the appropriate tension to the inferior capsuloligamentous complex of the joint.
Interscalene regional blockade has been effective in providing early postoperative pain relief and in decreasing overall narcotic requirements following surgery.
Strong indications for open stabilization procedures include significant degrees of glenoid or humeral bone loss, capsular deficiencies, or irreparable rotator cuff tears, particularly those of the subscapularis. In individuals with significant anterior glenoid erosion, an osseous reconstruction should be performed.
Revision instability surgery is the most technically challenging of all open shoulder surgery. When attempting to salvage failed anterior instability cases, surgeons should be prepared to face challenging scenarios such as distorted anatomic tissue planes, severe scarring, capsular deficiencies from multiple prior surgeries or thermal capsulorrhaphy, bony deficiencies due to erosion or fracture, and subscapularis deficiencies.
The treatment of shoulder instability has evolved rapidly in recent years due to a better understanding of shoulder biomechanics and pathoanatomy, advancements in imaging technology, and improvements in surgical implants and techniques. The goal of contemporary therapeutic approaches to glenohumeral joint instability is the restoration of anatomy. This requires a thorough and clear understanding of the anatomy and biomechanics of the glenohumeral articulation.
This chapter will summarize the relevant basic science, evaluation, and treatment of patients with labral pathology with an emphasis on shoulder instability, including discussion of those rare patients with instability secondary to bony abnormalities or posterior labral pathology. This chapter will also include a section on special considerations in revision surgery for failed stabilization procedures, complications, and future directions.
Anatomy
The glenohumeral joint is formed by a unique articulation between a larger and nearly spherical humeral head with a shallow and much smaller glenoid. Minimal bony constraints combined with a unique anatomical architecture and functional arrangements allow the shoulder joint to have the largest range of motion in the body. Despite its minimally constrained nature, the glenohumeral joint can carry both small and large loads at various speeds of arm motion while maintaining stability due the joint’s tremendous reliance on soft tissue support. Instability is defined as abnormal or painful excessive movement of the humeral head out of the glenoid during active shoulder motion and must be distinguished from laxity, which is asymptomatic instability in both normal and unstable shoulders.
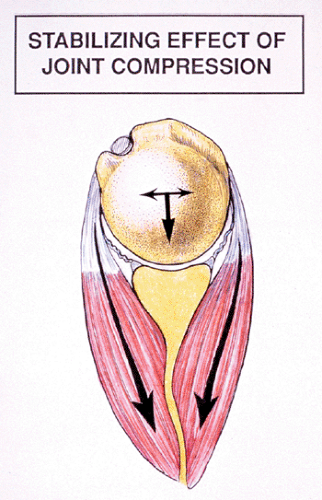
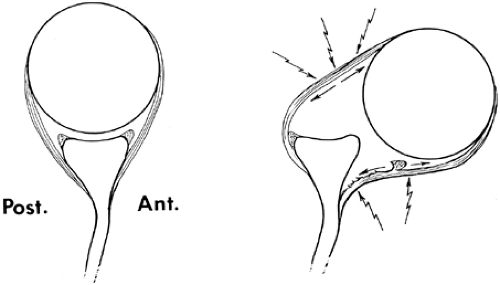
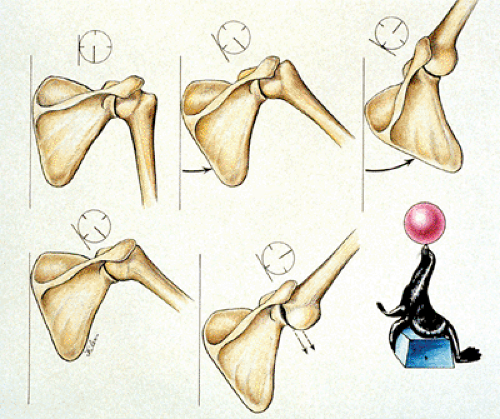
Glenohumeral stability is achieved by the complex interactions between static and dynamic constraints. Static constraints include the capsule, ligaments, and tendons; dynamic constraints are obtained by active muscle contraction. In the middle range of rotation, joint stability is provided by the dynamic action of the rotator cuff and the biceps muscles through compression of the humeral head in the glenoid socket (1) (Fig 12-1). The ligamentous structures provide passive restraints at the extremes of rotation, preventing excessive translation of the humeral head on the glenoid (Fig 12-2). Contraction of the muscles around the shoulder may also have the secondary effect of protecting the smaller ligamentous structures from injury at the end-range positions (2,3). Authors have demonstrated differences in rotator cuff and scapular muscle firing patterns between patients with stable and unstable shoulders (4).
The osseous anatomy, capsuloligamentous structures, negative intra-articular pressure, synovial fluid adhesion-cohesion, the rotator cuff, scapular stabilizers, and biceps tendon all play roles in providing stability (1,5,6). Additional factors that contribute to stability are patient age and gender, capsular integrity, and strength and conditioning of the rotator cuff, and scapular stabilizing muscles of the shoulder complex.
Static Stability Factor
The glenohumeral joint is inherently unstable, with the large humeral head articulating with the small and shallow glenoid. Static stability is provided by the orientation of the articular surfaces, the articular conformity of humerus and the glenoid, the glenoid labrum, the negative intra-articular pressure, the adhesion-cohesion of synovial joint fluid, and the glenohumeral joint capsule and its ligaments (1,7,8,9).
The glenoid labrum is a wedge-shaped fibrous ring attaching to the glenoid articular surface through a fibrocartilaginous transition zone. Below the glenoid equator, the inferior labrum is firmly continuous with the articular cartilage; above the equator it is more mobile and meniscal in nature.
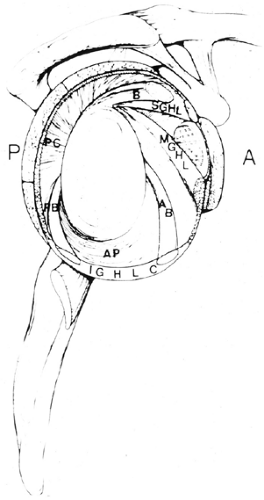
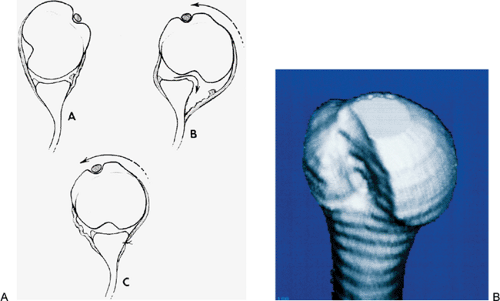
The contribution of the labrum to glenohumeral stability has been clearly established: It acts as the anchor point for the capsuloligamentous structures, increases the depth of the glenoid socket, facilitates the concavity-compression mechanism as the humeral head is compressed in the glenoid during rotator cuff contraction (10) (Fig 12-3). Loss of the labrum (Bankart lesion) has been reported to result in a 50% decrease in the glenoid depth. Lippit et al. (9) demonstrated that the translational force required to dislocate the humeral head was 20% smaller after removal of the glenoid labrum. Although the functional anatomy of the glenoid labrum is becoming better understood, its role in the glenohumeral restraining mechanism, particularly at the extremes of motion, remains unclear.
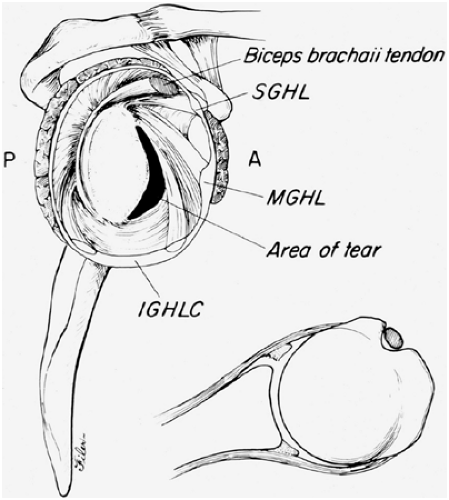
Discrete thickenings of the joint capsule have traditionally been described as the glenohumeral ligaments (Fig 12-4). The nomenclature is based on their attachment from superior to inferior and anterior to posterior. Improved understanding of the anatomy and biomechanics of the glenohumeral ligaments has resulted from numerous cadaveric studies and intraoperative observations. Because of the orientation of these ligaments, portions of the capsule reciprocally tighten and loosen as the glenohumeral joint rotates, thus limiting translation and rotation by load sharing (11,12,13) (Table 12-1). In the middle range of motion, these structures are relatively lax with a surface area two times that of the humeral head (14,15); therefore, stability in the midrange rotation is maintained primarily by the action of the rotator cuff muscles compressing the humeral head into the conforming glenoid socket (16).
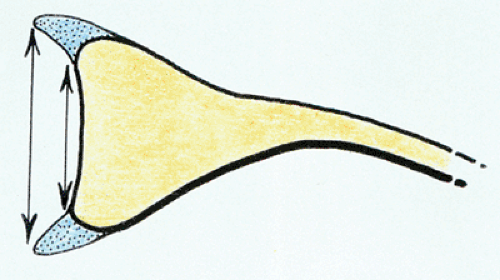 Fig 12-3. The labrum’s contribution to increasing the depth of the glenoid socket. (Adapted from Warner JJP, Carbon DM. Overview of shoulder instability. Crit Rev Phys Rehabil Med. 1992;4:145–198. ) |
Superior Glenohumeral Ligament
The superior glenohumeral ligament (SGHL) and coracohumeral ligament (CHL) originate on the supraglenoid tubercle and coracoid process, respectively, and both insert on the lesser tuberosity. Both make up the reinforcing structures of the rotator interval and are present in over 90% of individuals (17). These structures both provide resistance to inferior translation and external rotation when the arm is adducted (18). Additionally, both structures limit posterior translation when the arm is forward flexed, adducted,
and internally rotated. Lastly, the SGHL and the CHL are believed to prevent anterior-superior migration of the humeral head.
and internally rotated. Lastly, the SGHL and the CHL are believed to prevent anterior-superior migration of the humeral head.
Table 12-1 Anatomy and Function of the Glenohumeral Ligaments and Capsule | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
Middle Glenohumeral Ligament
The middle glenohumeral ligament (MGHL) is a highly variable structure between individuals. It presents as either a discrete band or a thickening of the anterior capsule confluent with the inferior glenohumeral ligament (IGHL) complex in 60% to 80% of the population (17,19). The MGHL originates from the glenoid tubercle or the anterior labrum and inserts on the lesser tuberosity, coursing oblique to the SGHL and CHL. The MGHL statically limits rotation of the adducted humerus, inferior translation of the adducted humerus and externally rotated humerus. In addition, the MGHL also limits anterior and posterior translation of the partly abducted (45 degree) and externally rotated arm.
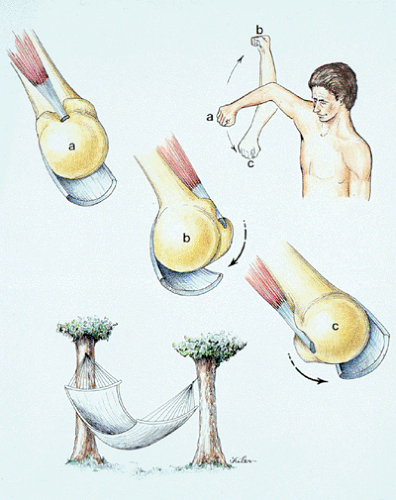
Inferior Glenohumeral Ligament
The IGHL functions as the primary restraint to anterior, posterior, and inferior glenohumeral translation between 45 degree and 90 degree elevation of the arm (20). The IGHL originates from the inferior half of the glenoid neck or the anterior-inferior labrum, to insert inferior to the MGHL on the lesser tuberosity. The IGHL forms a hammocklike structure with discrete anterior and posterior bands with an interposed pouch. This formation allows for reciprocal tightening and loosening, depending on arm position (Fig 12-5). In external rotation, the complex moves anteriorly; in internal rotation, the complex moves posteriorly (18).
Posterior Capsule
The posterior capsule starts just proximal to the posterior band of the IGHL. The posterior capsule is the thinnest portion of the shoulder capsule, measuring less than 1 mm in thickness (average thickness 1.5 mm), and as a result is believed to be the cause of poor results following posterior instability surgery (21). The posterior capsule limits posterior translation when the arm is in the forward flexed, adducted, and internally rotated position.
Rotator Interval
The rotator interval is the region of the shoulder defined by the borders of the supraspinatus superiorly, the subscapularis inferiorly, the corcoid process medially, and biceps laterally. The SGHL, CHL, and MGHL reinforce the rotator interval region. As a result, this region is highly variable among individuals (22). The rotator interval may be completely devoid of tissue or composed solely of loosely arranged collagen tissue; in a stable shoulder, this likely represents a normal variant. The rotator interval functions to limit inferior translation in the adducted arm, and tightens when the adducted arm is externally rotated (1). Laxity in the rotator interval may contribute to inferior and posterior glenohumeral instability. At the other end of the spectrum, an excessively tight rotator interval is associated with both adhesive capsulitis and post-operative stiffness (23).
Dynamic Stability Factors
Glenohumeral stability is mainly achieved through dynamic factors. Active contraction of the rotator cuff contributes to joint stabilization by coordinated muscular activity and by secondary tightening of the ligamentous constraints. This effect works in combination with the concavity-compression mechanism, in which muscle contraction causes compression of nearly congruent articular surfaces into one another.
The rotator cuff consists of the subscapularis, supraspinatus, infraspinatus, and teres minor muscles. The tendons of the rotator cuff muscles almost completely surround the humeral head as they blend together at their insertions on the greater and lesser tuberosities of the humerus. Because the rotator cuff muscles insert very close to the center of rotation of the axis of rotation of the humerus, the rotator cuff provides a joint compression force at the glenohumeral articulation. This coordinated compressive function of the rotator cuff muscles is required to counteract the upward shearing force of the strong deltoid muscle during abduction and/or flexion. The rotator cuff, therefore, maintains stability and allows for a spinning motion of the humerus on the glenoid by counteracting the shearing motion of the deltoid. Ligament and capsulolabral sectioning studies have demonstrated that muscle action of the rotator cuff and deltoid provided joint stability even after a large Bankart lesion was created or the entire capsule and glenohumeral ligaments were sectioned (21,24,25). Dynamic stability of the glenohumeral joint is also provided for by the contraction of the long head of the biceps, coordinated scapulothoracic rhythm, and the proprioceptive modulation of all dynamic factors (26).
The scapular rotators include the trapezius, rhomboids, the serratus anterior, and the levator scapulae. Of these, scapulothoracic rotation is primarily achieved by the serratus anterior and trapezius muscles, which provide the overall rhythm of the shoulder motion. The ratio of normal glenohumeral to scapulothoracic motion is 2:1 (glenohumeral
rotation to scapulothoracic rotation) (Fig 12-6). This normal relationship is important because it maintains the glenoid as a stable platform underneath the humeral head as the shoulder rotates into positions required for overhead motions such as throwing. Because the axioscapular muscles (scapular rotators) tend to fatigue first during repetitive overhead motions such as throwing and swimming, a lag in normal scapulothoracic rotation has been implicated as a contributing factor for instability and pain during shoulder motion in these sports activities (27).
rotation to scapulothoracic rotation) (Fig 12-6). This normal relationship is important because it maintains the glenoid as a stable platform underneath the humeral head as the shoulder rotates into positions required for overhead motions such as throwing. Because the axioscapular muscles (scapular rotators) tend to fatigue first during repetitive overhead motions such as throwing and swimming, a lag in normal scapulothoracic rotation has been implicated as a contributing factor for instability and pain during shoulder motion in these sports activities (27).
The serratus anterior acts as a scapular rotator and protractor, therefore normal positioning of the scapula and glenoid is dependent on proper serratus anterior function (28). Several authors have noted an association between altered serratus anterior function and anterior instability (2,29,30). Decreased serratus anterior function in unstable shoulders may cause decreased upward scapular rotation with shoulder abduction, scaption, or flexion which would alter the position of the humerus relative to the glenoid. This could be important in unstable shoulders where this altered scapulothoracic rhythm may act to increase shear forces across the glenohumeral joint via inefficient glenoid positioning.
The possible association between glenohumeral and scapulothoracic problems has been investigated by several authors, who have demonstrated scapular malpositiong or abnormal scapular function in patients with instability (2,4,30). However, although scapular malpositioning, or muscle dysfunction, is associated with shoulder instability (4,30,31,32), whether this represents a primary phenomenon or if painful conditions such as instability inhibit the scapulothoracic muscles secondarily is still unknown. The association between the scapular dyskinesias and instability form the rationale for supplementing rotator cuff strengthening with an axioscapular strengthening program when treating shoulder instability.
Bankart Lesions
For the humeral head to escape the glenoid fossa, the soft-tissue restraint must be disrupted. The location of the disruption depends on several factors such as the direction of the force applied to the shoulder; the position of the arm at the time of injury; and most importantly, the age of the patient. In older patients the more common lesion is a tear of the rotator cuff, the “posterior mechanism” of dislocation, with or without labral pathology; however, in patients younger than age 40 years, the predominant finding is a tear of the anteroinferior labrum, a Bankart lesion.
Bankart lesions have been considered the primary and most common pathology leading to recurrent anterior dislocation (33,34) (Fig 12-7). These lesions were originally described as injuries to the labrum corresponding to the detachment of the anchoring point of the IGHL and MGHLs from the glenoid rim. Taylor and Arciero (35) reported the arthroscopic findings in 63 patients who sustained an initial anterior dislocation. All patients in the study were younger than 24 years of age. Sixty-one of the 63 patients (93%) had an avulsion of the anteroinferior glenoid labrum (Bankart lesion) with no evidence of intracapsular injury. Fourteen of the 63 (22%) had an associated osseous lesion of the glenoid
rim. In addition, there were six superior labral tears, two included the biceps origin. There were no full-thickness rotator cuff tears.
rim. In addition, there were six superior labral tears, two included the biceps origin. There were no full-thickness rotator cuff tears.
Skeletal Lesions
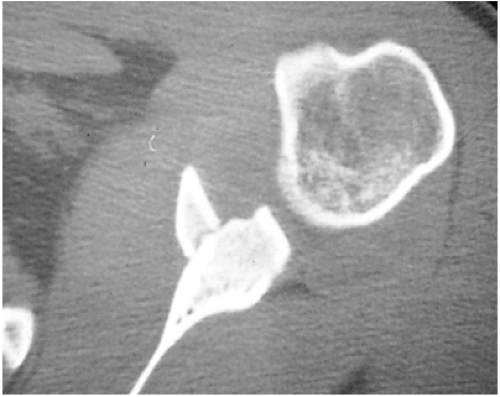
The limited constraint provided by the glenoid is further decreased by bony lesions of the anterior or posterior glenoid rim. These lesions may result from an osseous (anterior or posterior) Bankart lesion, a displaced glenoid fracture, or wear and erosion of the glenoid rim as a result of multiple recurrent dislocations (Fig 12-8). Burkhart and De Beer (36) reported on 194 consecutive arthroscopic Bankart repairs using a suture anchor technique with an average of 27 months follow-up. The 173 patients without significant bone defects sustained 4% recurrence rate, whereas 21 patients with significant bone defects (either glenoid rim fractures resulting in inverted-pear shaped glenoids or humeral engaging Hill-Sachs lesions) sustained a 67% recurrence rate. The authors concluded that restoring bony anatomy is imperative for preventing recurrence and that arthroscopic Bankart repairs should not be performed in patients with the aforementioned significant bone defects.
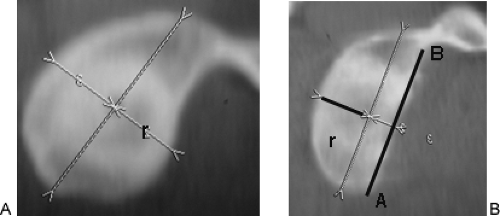
Gerber et al. (37) have reported their clinical experience, which suggests that if a defect involves more than 25% of the glenoid surface, it should be repaired with intra-articular bone grafting. Gerber and Nyffeler (38) demonstrated a method for quantifying the degree of glenoid bone loss with computed tomography (CT) scan by measuring the glenoid surface on either an oblique sagittal image or a three-dimensional reconstruction. Through biomechanical testing, they determined that the force required for anterior dislocation is reduced by 70%, compared with that required when the glenoid is intact, if the length of the glenoid defect exceeds the radius (Fig 12-9). The goal of surgery is to increase the glenoid constraint and provide support for the joint capsule; however, in cases of excessive glenoid bone loss, standard Bankart repairs (arthroscopic or open) are likely to fail, and osseous augmentation is recommended (39).
Capsular Lesions
Traumatic intra-substance injury of the joint capsule is commonly associated with anterior dislocation. Depending on the magnitude of the anterior shear force, either plastic deformation or a complete tear of the joint capsule can occur. The recognition of a concomitant posttraumatic capsular laxity or rupture and a Bankart lesion is essential in order to select the correct surgical procedure. A traumatic capsular rupture or open rotator interval leads to venting of the joint, which increases glenohumeral translation. A positive sulcus sign in external rotation is the clinical sign for an open rotator interval.
Wolf et al. (40) described an intra-articular lesion associated with anterior instability where the glenohumeral ligaments are disruptive from the humerus and not the glenoid as in the case of a classic Bankart lesion. The authors coined the term a humeral avulsion of the glenohumeral ligaments, or HAGL lesion (40). Although the entity appears to be rare, the authors concluded that the diagnosis must be kept in mind particularly in cases of traumatic anterior dislocations in the absence of Bankart lesions. Boker et al. (41) reported on the largest series (41 cases) so far in the literature of HAGL lesions in contact athletes. The authors demonstrated that the surgeon must keep a high suspicion for a HAGL lesion in patients who have sustained a traumatic anterior dislocation and fail to have evidence of a Bankart lesion at arthroscopic examination. Although there is debate as to the best way to address the HAGL lesion, either open or arthroscopically, the current consensus appears to be that the lesion must be addressed in some way if surgical intervention is chosen (42).
Rarely, HAGL lesions may occur in conjunction with a Bankart lesion. Thus, appreciation of the humeral capsular insertion is important at the time of surgery. Tensioning of the capsule in the midrange can potentially overtighten and constrain the joint limiting rotation. In extreme cases, this can lead to posterior subluxation of the humeral head and arthritis (43,44).
Superior Labral Lesions
Lesions of the superior labrum have been associated with glenohumeral instability. Hinterman and Gachter (45) noted
that 7% of their patients (14 of 212) with traumatic anterior instability requiring surgery had lesions of the superior labrum. Taylor and Arciero (35) reported 10% (6 of 63) of their patients had superior labral lesions associated with an initial anterior dislocation. Pagnani et al. (46) showed in a cadaver study that superior labral lesions contributed to instability of the glenohumeral joint if the biceps attachment was destabilized.
that 7% of their patients (14 of 212) with traumatic anterior instability requiring surgery had lesions of the superior labrum. Taylor and Arciero (35) reported 10% (6 of 63) of their patients had superior labral lesions associated with an initial anterior dislocation. Pagnani et al. (46) showed in a cadaver study that superior labral lesions contributed to instability of the glenohumeral joint if the biceps attachment was destabilized.
Hill-Sachs Lesions
The most common bony lesion associated with traumatic glenohumeral instability is a compression fracture at the posterolateral margin of the humeral head (Fig 12-10). Commonly known as a Hill-Sachs lesion, this fracture occurs as the humeral head impacts the glenoid edge during dislocation. The lesion is present in 80% of anterior dislocations, 25% of anterior subluxations, and almost 100% of cases of recurrent anterior instability (19). With posterior instability, a reverse Hill-Sachs lesion results from impaction of the articular surface when the humeral head dislocates over the posterior glenoid rim. These articular humeral lesions rarely contribute to instability, as they are usually small; however, when the lesion includes more than 30% of the articular surface and associated with instability, it may be an important indication for surgery (17). Such large lesions occur only after recurrent dislocations. Gerber and Lambert (47) have demonstrated that one option of treating these kinds of injuries is restoration of normal articular cartilage conformity by allograft reconstruction.
Instability
We use a classification system originally proposed by the Hospital of Special Surgery (Table 12-2). This system categorizes shoulder instability on the basis of four criteria: frequency, etiology, degree, and direction.
Frequency
The instability itself may be acute or chronic, the differentiating feature being whether the event occurred within the
previous 24 hours. The number of recurrences (frequency of instability) is also critical in the classification scheme because it contributes to the level of damage to anatomic structures. This characteristic is extremely important when considering the degree and cause of instability. This component of the history is critical in determining the appropriate treatment.
previous 24 hours. The number of recurrences (frequency of instability) is also critical in the classification scheme because it contributes to the level of damage to anatomic structures. This characteristic is extremely important when considering the degree and cause of instability. This component of the history is critical in determining the appropriate treatment.
Table 12-2 Classification of Shoulder Instability | |
|---|---|
|
Etiology
Etiology can be subdivided into traumatic, microtraumatic, or atraumatic groups also includes congenital and neuromuscular causes. The atraumatic group includes patients who exhibit a voluntary component of their instability. In this classification, these patients can be further subdivided into group I: voluntary instability, which is arm-position dependent and usually posterior; and group II: voluntary instability exhibited by the ability to selectively contract muscles, causing dislocation. Although patients in group I can voluntarily demonstrate instability, they chose to avoid dangerous arm positions. This condition subsequently affects activities of daily living (48). Conversely, patients in group II tend to have an underlying psychiatric problem, using their instability as a means to control their environment (49).
Degree of Instability
The degree of instability (dislocation, subluxation, and microinstability) is also important in determining appropriate treatment options. Dislocation refers to complete dissociation of the articular surfaces of the humeral head and the glenoid cavity. Subluxation describes increased humeral head translation within the glenoid cavity, where the humeral head translates to the edge of the glenoid without true dislocation. Microinstability in the shoulder joint is a more subtle instability pattern.
Recurrent subluxation may manifest as pain rather than instability. Repetitive, high-energy, overhead activities can cause progressive attenuation of the capsular, ligamentous, and labral structures (50,51,52). As these static stabilizers fail and the dynamic stabilizers weaken, anterior subluxation occurs leading to impingement symptoms. This results from recurrent microtrauma which can ultimately lead to rotator cuff tearing and destabilization of bicep-labral complex.
Direction of Instability
The direction of instability has been a critical component of most classification systems. Traditionally, there was an assumption that 95% of shoulder instability was anterior (53). It has become increasingly apparent, however, that many athletes with ligamentous laxity have instability that is primarily posterior in nature (54,55,56,57). These patients suffer recurrent posterior subluxation and have a history of posterior shoulder pain rather than complaints of frank instability. This category of patients is more prevalent than previously recognized but should be distinguished from the rare true posterior dislocation that results from an acute traumatic event (58,59).
Traumatic posterior shoulder dislocation is notoriously overlooked on initial patients presentation. Hawkins et al. (60) reported on a series of 40 patients with 41 locked posterior shoulder dislocations. The initial physician missed the diagnosis in the majority of the cases reviewed. In this often quoted series, the causes of posterior dislocation were motor-vehicle accidents, seizures, alcohol-related injuries, or electroshock therapy.
History
The history can raise suspicion of shoulder instability. A patient’s age, occupation, employment status, activity level, hand dominance, and other medical problems ate helpful in classifying the nature of the instability. Certain circumstances, such as work-related injuries or those with associated litigation, might affect patients’ perception of their disabilities as well as their expectations for recovery and compliance (61).
The clinician should seek out specific complaints. For example, a patient who is a contact athlete may indicate that the arm “went dead” during a football tackle or ice-hockey check (62). This symptom is likely associated with a traumatic subluxation of the joint and the presence of a Bankart lesion. Another example is the patient who gives a history of having a seizure and then awaking with the sensation of the joint “out of place.” This situation suggests posterior dislocation or subluxation as the result of unchecked internal rotation forces overcoming the weak external rotators of the shoulder.
A careful history and physical exam will provide information about the onset, direction, degree, duration, frequency of symptoms, and previous surgical treatments. Determining the presence of a traumatic cause will provide clues about the pathoanatomy that can be expected. Arm position, at the time of initial injury and during symptoms, can help differentiated the direction of the instability.
If pain is a major component of the patient’s complaint, which activities cause the pain? When examining athletes, the clinician should always question as to the type of sports, the position played, and the duration, frequency and level of involvement. For example, throwers, swimmers, and tennis players may develop excessive capsular laxity as a result of subjecting their shoulders to repetitive microtrauma (63,64). The result is recurrent shoulder subluxation, which can create a sense of “looseness” or “slipping” with activity. In addition, secondary “non-outlet” impingement can occur as anterior instability decreases the subacromial space, causing pain with over-head activities. Furthermore, these same subluxations can create damage to the superior labral area, creating a SLAP lesion, especially in the setting of a contracted posterior capsule (65).
In recent years the existence of posterior instability has become better recognized. Posterior subluxation has been well documented in athletes who require repetitive arm motion in front of the body, such as offensive-line football
players, volleyball, softball, and baseball players (54,56,57). Throwing sports in particular lead to posterior shoulder pain during late-cocking and follow-through phases, which has been associated with posterior subluxation and resultant microtrauma to the posterior capsulolabral complex (65,66).
players, volleyball, softball, and baseball players (54,56,57). Throwing sports in particular lead to posterior shoulder pain during late-cocking and follow-through phases, which has been associated with posterior subluxation and resultant microtrauma to the posterior capsulolabral complex (65,66).
Physical Findings
A systematic evaluation includes observation for abnormal motion patterns and atrophy, palpation to localize painful areas, assessment of both active and passive range of motion, measurement of strength of the rotator cuff, deltoid and scapular stabilizer muscles, neurovascular examination, and finally provocative testing maneuvers for instability. It is important to examine the opposite shoulder for comparison.
In evaluating shoulder motion, the examiner must carefully document any scapulothoracic substitution for glenohumeral motion, scapular winging, and other abnormal muscle patterns. Atrophy of the spinatus muscles may indicate longstanding associated rotator cuff tear or injury to the suprascapular nerve. Similarly, atrophy of the deltoid may indicate axillary nerve injury.
In addition, patients should always be assessed for findings of generalized ligamentous laxity, including the ability to hyperextend their elbows more than 10 degrees, apply the thumb to the forearm, hyperextend the metacarpalphalangeal joints more than 90 degree, or touch the palm of each hand to the floor while keeping the knees extended (Fig 12-11). While there is no direct relationship between generalized laxity and shoulder instability, there is some association between hyperlaxity and glenocapsular development (61).
The patient with an acute, unreduced anterior shoulder dislocation typically holds the arm in slight abduction and internal rotation (20,50). Before attempting any reduction maneuvers, carefully perform a neurovascular examination to rule out brachial plexus injury, and specifically an axillary nerve injury (67,68). The latter condition may sometimes escape detection, as decreased sensation over the lateral deltoid is not always present with an injury to this nerve. In patients older than 60 years of age or younger patients involved in severe trauma, be aware of the possibility of an associated fracture of the humerus (69). Therefore, proper radiographic imaging is particularly important before attempting closed reduction in such cases.
 Fig 12-11. Example of generalized ligamentous laxity, demonstrating the ability to apply the thumb to the forearm. |
Regardless of the particular closed reduction maneuver employed, perform all maneuvers as a gradual and gentle technique with appropriate analgesia (either intravenous or intra-articular) to ensure muscle relaxation. A method of gentle traction in line with the arm using counter-traction is usually successful.
Always be alert to the possibility of an unrecognized chronic (fixed) dislocation. The direction is typically posterior, however a chronic anterior dislocation is also possible. Many of these patients are poor historians secondary to dementia or chronic alcohol abuse (60). On exam, a patient with a fixed posterior dislocation will have severe limitation of external rotation compared to their opposite shoulder. Upon inspection, there is typically a flattening of the anterior aspect of the shoulder with an associated prominence of the coracoid process and possibly some prominence and rounding of the posterior aspect of the shoulder. The application of excessive force in attempting to close reduce such an injury risks neurovascular injury and/or fracture.
Athletes with instability are typically first seen by an orthopedic surgeon in the office, or in the training room, not in the emergency department. They may have had a documented episode of instability, or an injury with pain, but no true sense of shoulder instability. After a careful neurovascular examination, it is important to assess both active and passive range-of-motion. A discrepancy between active and passive motion may indicate either an associated rotator cuff tear or a nerve injury.
It is particularly important to identify a subscapularis tear in the setting of shoulder instability, a condition that is frequently missed (70,71). Patients with such tears can passively increase externally rotation with the arm adducted at the side, as well as associated apprehension in this position. Strength assessment is also important. Significant external rotation weakness may indicate a rotator cuff tear.
A subscapularis tear also typically demonstrates internal rotation weakness. In this situation, the patient has an associated lift-off sign and belly-press test. The belly-press test maneuver is very useful in situations when the patient lacks adequate internal rotation to perform a lift-off test. To perform the belly-press test, the patient places their hand on their abdomen, with their elbow flexed at 90 degree, and attempts to bring their elbow anterior to the coronal plane of their body, while keeping the hand on their abdomen at all times. If the elbow remains posterior to the anterior aspect of the mid-abdomen (i.e., the coronal plane of their body), there is likely a subscapularis tendon tear.
Specific tests for shoulder instability allow the clinician to classify the instability pattern. The apprehension test was originally described by Neer and Foster (72). With the patient seated or standing, place the symptomatic shoulder into a position of 90 degree of abduction and maximum external rotation. The patient’s withdrawing from the examiner or complaining about a sense of shoulder instability demonstrates apprehension.
Pain as a chief complaint is not specific for shoulder instability. Other shoulder conditions such as arthritis and rotator cuff disease commonly present with shoulder pain. Kvitne and Jobe (73) proposed a modification of the apprehension maneuver to increase specificity for subtle anterior instability. Place the patient in a supine position, and perform the apprehension test as described above. Ask whether the patient has a sense of instability or simply pain. Place posterior pressure on the humerus, and ask whether this pressure relieves the sense of apprehension or pain. This “relocation maneuver” increases specificity of the diagnosis of instability if the patient reports decreased apprehension. If this maneuver simply reduces pain, it is not diagnostic of instability and may be associated with a variety of other diagnoses, including a SLAP lesion or impingement syndrome (74).
Inconsistencies in the apprehension test led Gerber and Ganz (75) to develop the anterior and posterior drawer test to assess the shoulder for excessive translation compared with the contralateral side. Others have found merit in this method of examination and have developed grading scales for the degree of shoulder laxity (76,77,78). These tests may offer some insight into the degree and direction of the instability. If one assesses laxity of the shoulder in the office setting, it is important to determine whether translation of the humeral head is greater on the painful side and whether this translation causes symptoms (55). Laxity testing assessment in the office setting can be of limited value if pain is causing the patient to guard the affected shoulder. Instead, this method is best used during examination under anesthesia to confirm the suspected degree and direction of shoulder instability.
Altchek et al. (76) and Hawkins et al. (78) proposed a grading scale for translation of the humeral head on the glenoid. Instability is graded on a scale of 0 – 3+ for all three directions (anterior, posterior, and inferior). For anterior and posterior drawer testing, a grade of 0 represents no humeral head translation, while movement of the humeral head up to but not over the glenoid rim represents 1+ instability. Translation of the humeral head over the glenoid rim with an associated spontaneous reduction with relief of pressure represents 2+ instability. Frank dislocation and locking of the humeral head over the glenoid rim is graded as 3+ instability. Whether in the office or under anesthesia, when performing drawer tests, it is important to bear in mind that the position of the arm determines the degree of tension in the glenohumeral ligaments. With the arm at the side in adduction, the IGHL is relatively lax, and anterior and posterior drawer testing may be of limited value. In abduction, the IGHL comes underneath the humeral head and forms a hammock that passively limits anterior, posterior, and inferior translation (79,80). Perform anterior drawer testing with the shoulder positioned in abduction in the plane of the scapula. Maintain the arm in neutral rotation while using one hand to place an axial load along the humerus and the other hand to apply an anterior or posterior force to the humerus. Often the examiner can feel the humeral head move back into the glenoid rather than out of the glenoid during the maneuver. The patient may note a painful click with such a maneuver. This can be particularly helpful in identifying posterior instability.
Posterior apprehension can be elicited by a modification of the posterior drawer test. To perform this modification, place the patient’s arm in 90 degree of forward flexion and adduction while applying an axial load down the shaft of the humerus. Pain and a palpable shift and click suggests posterior labral injury and instability (61).
A modification of this test, termed the jerk test, has been described for posterior instability (81,82). With the patient seated, load the adducted shoulder axially into the glenoid with one hand, and with the other hand, palpate the posterior aspect of the shoulder. Then bring the arm into horizontal abduction anterior to the plane of the scapula; the humeral head may sublux posteriorly. Then bring the humerus posterior to the plane of the scapula; the humeral head may suddenly reduce into the glenoid. A palpable shift and pain accompany a positive test.
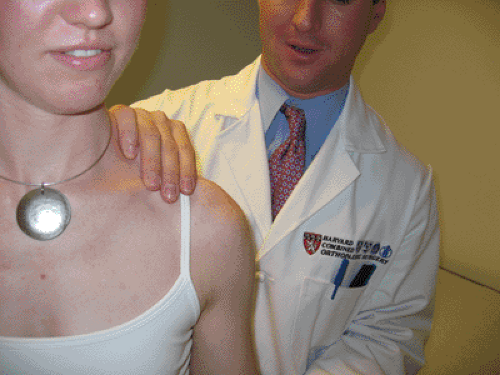
The sulcus sign is basically an inferior drawer test (Fig 12-12). Originally described by Neer and Foster (72), it was initially believed to be pathognomonic for inferior and multidirectional instability. Unfortunately, a common misconception has been that a large sulcus sign that is asymptomatic, thus indicates inherent joint laxity, is a positive finding. The key point is that this maneuver should be associated with pain and should reproduce the patient’s symptoms to be clinically relevant as a finding of inferior instability. A positive
sulcus sign in the absence of clinical symptoms is diagnostic only for inferior laxity, not inferior instability.
sulcus sign in the absence of clinical symptoms is diagnostic only for inferior laxity, not inferior instability.
To perform the sulcus test, have the patient seated and the arm adducted at the side. Rotation of the shoulder is very important in assessing the degree of inferior instability. First, with the arm in neutral rotation, pull the humerus inferiorly, and estimate the amount of separation between the acromion and the humeral head. Grade is based on a scale of 0 – 3+ (76): A separation of 1 cm is a 1+ sulcus sign, 2 cm is a 2+ sulcus sign, and 3 cm is a 3+ sulcus sign. Anatomically, a sulcus sign greater than 2+ indicates a capacious capsule and specific laxity of the anterosuperior capsular region (rotator interval).
The sulcus sign should always be repeated with the arm placed in external rotation. If the sulcus sign remains greater than 2+ with the arm in external rotation, there is a marked deficiency of the superior capsule, and a large rotator interval defect in the capsule is likely (61). This is the result of damage to the superior and MGHLs, as well as the CHL. With this information before surgical repair, the surgeon then knows that surgical reconstruction of this region (rotator interval closure) with a capsular shift must be a component of the operation (83,84).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree