Shoulder Anatomy and Biomechanics
Dawn L. Swarm MD
Andrew T. Mahar MS
Derek W. Weichel BS
Robert A. Pedowitz MD, Phd
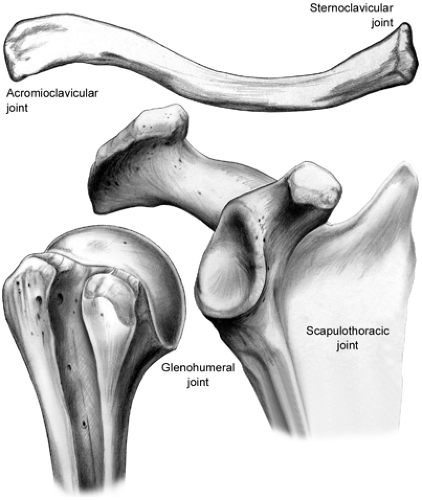
The shoulder complex is composed of three bones—the clavicle, the scapula, and the humerus—as well as four articulations—the acromioclavicular (AC), the sternoclavicular (SC), the scapulothoracic, and the glenohumeral (GH) joints.
The clavicle serves a variety of functions. It acts as a rigid base for muscular attachments of the shoulder, neck, and chest. It also provides protection for the major vessels at the base of the neck and for the nerves and vessels supplying the upper limb. In addition, it forms a strut that holds the GH joint in the parasagittal plane.
The scapula is a flat, triangular-shaped bone that serves as the articulating surface for the head of the humerus as well as provides areas for 17 muscle attachments.
The proximal humerus is composed of the humeral head, the lesser and greater tuberosities, the bicipital groove, and the proximal humeral shaft.
The AC joint is a diarthrodial joint and the only articulation between the clavicle and the scapula. The motion of the AC joint is minimal, involving small translations and, mainly, rotation between the clavicle and the acromion with arm movement.
The SC joint is the only true joint that connects the upper extremity to the axial skeleton. It is a gliding joint with little inherent bony stability.
The scapulothoracic articulation is not a true joint, but it represents the space between the concave surface of the anterior scapula and the convex surface of the posterior chest wall. The muscular and ligamentous attachments provide the stability of this articulation as the scapula retracts, protracts, and rotates along the posterior chest wall.
The GH joint is a diarthrodial joint with minimal bony constraint, allowing it the largest range of motion of any major diarthrodial joint in the body.
The glenoid labrum provides another static restraint to GH motion. The labrum is a fibrous ring that is attached to the glenoid articular surface through a fibrocartilagenous transition zone.
The GH ligaments function as static restraints to shoulder motion.
The rotator cuff (RTC) muscles, as well as the scapular rotators, contribute to GH stability by enhancing the concavity–compression mechanism. Contraction of the long head of the biceps tendon, coordinated scapulothoracic rhythm, and proprioceptive mechanoreceptors in the joint capsule also contribute to the stability.
The RTC is composed of the supraspinatus, the infraspinatus, the subscapularis, and the teres minor muscles. The RTC often serves more than one function simultaneously. The muscles act as prime movers if the line of action is within the intended direction of motion.
Nerve injuries can occur with both arthroscopic and open shoulder procedures.
RTC repair using an open technique has been clinically successful in terms of repair, although arthroscopic techniques are now more common.
The shoulder is a complex joint that has the greatest degree of mobility of all major joints in the human body. The osseous and ligamentous structures that comprise the joint, as well as the surrounding musculature, interact to provide a wide range of motion as well as stability. Under normal conditions, four articulations move in synchrony, allowing smooth, unhindered motion of the arm. The control of
glenohumeral (GH) stability is achieved by the complex interaction between the static restraints (i.e., the ligament and tendons) and the dynamic restraints (i.e., muscular contraction acting across the joint).
glenohumeral (GH) stability is achieved by the complex interaction between the static restraints (i.e., the ligament and tendons) and the dynamic restraints (i.e., muscular contraction acting across the joint).
The shoulder complex is composed of three bones—the clavicle, the scapula, and the humerus—as well as four articulations—the acromioclavicular (AC), the sternoclavicular (SC), the scapulothoracic, and the GH joints (Fig 10-1).
Clavicle
The clavicle, an “S”-shaped bone, is the only long bone that ossifies by an intramembranous process. It is the first bone in the body to ossify (fifth week of fetal gestation) and is the last bone to fuse (medial epiphysis at 25 years of age). The clavicle consists of cancellous bone surrounded by an outer layer of compact bone, and it is unique in that it does not have a medullary cavity (1,2).
The clavicle serves a variety of functions. First, it acts as a rigid base for muscular attachments of the shoulder, neck, and chest. It also provides protection for the major vessels at the base of the neck and for the nerves and vessels supplying the upper limb. In addition, it forms a strut that holds the GH joint in the parasagittal plane, increasing the range of motion of the shoulder as well as the power of the arm in motions above the horizontal (1).
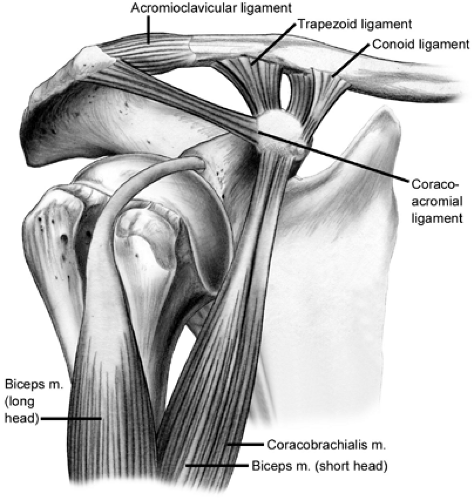
The clavicle articulates with the manubrium of the sternum through the SC joint and with the acromion at the AC joint. It is attached to the coracoid by the coracoclavicular ligaments, the conoid medially and the trapezoid laterally.
Scapula
The scapula is a flat, triangular-shaped bone that serves as the articulating surface for the head of the humerus as well as provides areas for 17 muscle attachments. With the arm at the side, the scapula overlaps the dorsal surfaces of the second to seventh ribs. It has three prominent projections: the spine, the coracoid process, and the acromion. The scapular spine divides the posterior aspect of the scapula into two depressions, the supraspinatus fossa and the infraspinatus fossa. In addition, the spine serves as a site for insertion of the trapezius muscle and as the origin for the posterior third of the deltoid muscle (2,3).
The coracoid process is a hooklike projection that curves anteriorly, upward, and outward in front of the glenoid cavity. The base of the coracoid is the attachment site of the coracoclavicular ligaments. The tip serves as the origin of the short head of the biceps and the coracobrachialis muscles and as the insertion site of the pectoralis minor muscle. The coracoid also serves as the anterior limit of the coracoacromial arch and is a palpable landmark during rotator cuff (RTC) surgery (2,3).
The acromion serves as an attachment site for the trapezius muscle above and the deltoid muscle below, and it articulates with the distal clavicle. The acromion usually forms from two or three ossification centers that appear during puberty and that fuse between 18 and 25 years of age. These three ossification centers are described as the preacromion, the mesoacromion, and the meta-acromion. The os acromiale, an unfused secondary ossification, occurs with an incidence of 1% to 15%, and 60% of cases involve bilaterality (4,5,6,7). The most common location is at the junction of the meso- and meta-acromion (4,7). An os acromiale can be identified on an axillary radiograph or magnetic resonance image (MRI) and should not be mistaken for a fracture.
In addition, the acromion has been classified into three morphologic patterns as viewed on a scapular outlet radiograph: flat (Type I), curved (Type II), and hooked (Type III) (8). A Type III morphology has been implicated in impingement and RTC pathology (9,10). Investigators have further classified the acromion based on thickness: Type A, <8 mm; Type B, 8–12 mm; and Type C, >12 mm (11).
Differences in the size of the acromion have been observed between men and women. Nicholson et al. (7) observed in men that the average length was 48.5 mm, the average anterior width was 19.5 mm, and the average anterior thickness was 7.7 mm. In women, the acromial length averaged 40.6 mm, the anterior width averaged 18.4 mm, and the
anterior thickness averaged 6.7 mm (7). That study also determined that basic acromial morphology is a primary anatomical characteristic independent of age and, in contrast, that anterior acromial spurs were dependent on age, because they were present in only 7% of patients <50 years and in 30% of patients >50 years.
anterior thickness averaged 6.7 mm (7). That study also determined that basic acromial morphology is a primary anatomical characteristic independent of age and, in contrast, that anterior acromial spurs were dependent on age, because they were present in only 7% of patients <50 years and in 30% of patients >50 years.
The acromion contributes to the coracoacromial arch, or supraspinatus outlet, which consists of the coracoid process, the acromion, and the coracoacromial ligament. This arch marks the superior boundary of the subacromial space. Interest has been focused on the structure and function of the coracoclavicular ligament and the importance of the coracoacromial arch (12,13,14,15). Although commonly described as having a “Y”-shaped configuration, other morphological types of the coracoclavicular ligament have been described (13,14,15,16). Soslowsky et al. (15) identified four types: quadrangular (48%); “Y”-shaped, with a broader lateral band and thinner medial band (42%); broad banded (8%); and with multiple bands (2%). The length of the coracoid attachment averaged 32 mm and the length of the acromial attachment averaged 19 mm. The average midpoint thickness was 1.3 mm. The length of the lateral band was significantly shorter, and the cross-sectional area was significantly larger, in specimens with a tear in the RTC (15).
The role of the coracoacromial arch as a secondary restraint to anterosuperior migration of the humeral head also has become of interest (17,18,19). The coracoacromial ligament has been shown to provide a static restraint to the GH joint as well as significantly contributing to anterior GH stability at 30 degrees of abduction (20,21). Release of the coracoacromial ligament has been suggested to increase both anterior and superior translation of the humeral head. It is important to maintain the integrity of the coracoacromial arch in the cuff-deficient shoulder, because the arch is the last restraint to anterosuperior migration (12,20,22).
The scapula also gives rise to the glenoid cavity, which is situated laterally, below the acromion. This lateral thickening of the scapula provides the bony articulation with the humeral head. The articular surface of the glenoid is concave and covered with hyaline cartilage, which is thinner in the center and thicker toward the periphery. A bare spot exists in the center of the inferior glenoid, which is equidistant to the anterior, posterior, and inferior glenoid rim when viewed with an arthroscope (23,24).
Glenoid version has been examined in several studies (25,26,27,28). In most, the glenoid displayed from 2 to 10 degrees of retroversion in relation to the long axis of the scapula, with an average of superior tilt of 5 degrees (26,27,28,29,30,31). In a study measuring the glenoid version in relation to the supraspinatus fossa, 40% were retroverted, 38% neutral, and 22% anteverted (32).
In addition, the shape of glenoid also changes from superior to inferior (28,33,34,35,36). Inui et al. (34,37) have shown that the superior part of glenoid surface is retroverted and that the inferior portion may be anteverted. In an MRI study of 40 subjects, Inui et al. (34) showed the upper aspect has a large radius of curvature, is convex, and subsequently, becomes flat and then concave in the lower portion with a small radius of curvature.
The shape of the glenoid resembles a pear, being 20% narrower superiorly than inferiorly (23,26,38). The reported average vertical diameter ranges from 33 to 39 mm (24,26,30,35) and the average transverse diameter from 23 to 29 mm (24,26,30,35,39). The distance from the anteroinferior margin of the glenoid to the bare area averages 12.8 mm (23,24).
Humerus
The proximal humerus is composed of the humeral head, the lesser and greater tuberosities, the bicipital groove, and the proximal humeral shaft, and it is highly variable. The anatomical neck lies at the junction of the articular surface of the head and the greater tuberosity and humeral shaft. The surgical neck lies below the greater and lesser tuberosities. The major blood supply to the humeral head is through the ascending branch of the anterior humeral circumflex artery, which penetrates the head at the bicipital groove and becomes the arcuate artery. This artery crosses under the tendon of the long head of the biceps, runs proximally just adjacent to the lateral aspect of the bicipital groove, and enters the humeral head at the proximal end of transition from the greater tuberosity to the bicipital groove. The posterior circumflex artery supplies the posterior portion of the greater tuberosity and a small posteroinferior part of the humeral head (2,3).
The bicipital groove lies on the anterior proximal humerus, just below the articular surface, and it is defined by the greater and lesser tuberosities. The long head of the biceps tendon lies in this groove and is covered by the transverse humeral ligament.
Both the greater and lesser tuberosities provide attachment for the RTC tendons. The supraspinatus, infraspinatus, and teres minor insert on the greater tuberosity from superior to posterior.
The subscapularis tendon attaches to the lesser tuberosity, also overlying the bicipital groove, and provides additional support to the long head of the biceps tendon (2,3).
Multiple studies have been performed to determine the head–neck ratio, the central axis of the humerus, and the anatomical relationships of the greater tuberosity and the bicipital groove assist in prosthetic replacement and design (22,26,40,41). The articular surface of the humeral head has an average radius of from 42 to 46 mm, whereas the average thickness of the humeral head is 19 mm. The thickness of the humeral head is proportional to both the length of the humerus and the head radius (41,42). The humeral head is retroverted from -6.5 to 35 degrees relative to the
transepicondylar axis of the distal humerus (31,40,41). The angle formed by the neck and shaft axes varies from 114 to 147 degrees (28,42,43). No significant differences between genders have been reported; however, a difference in the retroversion angle has been found between dominant and nondominant sides, with a measure of 33 degrees on the dominant side and 29 degrees on the nondominant side (22).
transepicondylar axis of the distal humerus (31,40,41). The angle formed by the neck and shaft axes varies from 114 to 147 degrees (28,42,43). No significant differences between genders have been reported; however, a difference in the retroversion angle has been found between dominant and nondominant sides, with a measure of 33 degrees on the dominant side and 29 degrees on the nondominant side (22).
The humeral head center is offset from the humeral axis by 7 mm medial and 2 mm posterior. A predictable relationship has been found between the central axis of the humeral head and the bicipital groove. In an evaluation of 18 cadavers, the average distance between the central axis of the humeral head and biceps tendon was 9 mm posterior to the posterior margin of the bicipital groove (44). The superior aspect of the humeral head is 6 mm higher than the superior aspect of the greater tuberosity (40). Iannotti et al. (26) reported that the mean distance between the greater tuberosity and the humeral head was 10 mm or less and that this distance was not correlated with other parameters. Takase et al. (45), however, found a significant correlation between the size of the humeral head and the neck shaft angle regardless of gender or age.
The bicipital groove rotates internally along its course between the upper and lower aspects of the proximal humerus. The mean change in rotation of the lateral lip from the proximal to distal groove was 15.9 degrees (40,46). Rotation of the bicipital groove in the proximal-to-distal direction is relevant to shoulder fracture work, particularly fracture arthroplasty, because the groove can assist with proper orientation of humeral head version.
Acromioclavicular Joint
The AC joint is a diarthrodial joint and the only articulation between the clavicle and scapula. Variable inclinations exist, with being nearly vertical to angled downward and medially accounting for up to 50 degrees (2,3). The AC joint has an incomplete fibrocartilagenous intra-articular disc, potentially predisposing it to degenerative changes.
Degenerative changes have been shown to occur as early as the second decade of life, with loss of articular cartilage, eburnation of subchondral bone, and formation of marginal osteophytes; however, these changes do not necessarily produce symptoms (47).
The motion of a normal AC joint is minimal, involving small translations and, mainly, rotation between the clavicle and the acromion with arm movement. The AC ligaments prevent anteroposterior instability (Fig 10-2). Biomechanical studies have shown that the inferior AC capsular ligaments represent the major restraint against anterior joint translations, whereas the superior and posterior ligaments provide the most stability against posterior translations (56% and 25%, respectively) (48,49). Therefore, the posterior and superior capsular ligaments should be spared during distal clavicle excision to prevent excessive posterior clavicle translations after resection (49,50). The coracoclavicular ligaments (the trapezoid and the conoid) together resist superior displacement of the joint, but with larger amounts of displacement and induced loads, the conoid ligament contributes the major share (48,49).
Sternoclavicular Joint
The SC joint is the only true joint that connects the upper extremity to the axial skeleton. It is a gliding joint with little inherent bony stability. Substantial incongruity exists between the two articular surfaces, but the interposition of an intra-articular disc compensates for this (2,3). This disc has not shown severe degenerative alterations until the seventh decade of life, but even then, the joint seems to be well preserved (47).
The SC joint is enveloped in a loose, fibrous capsule that blends with the margin of the disc (47). The stability of the joint, which is provided mainly by the surrounding ligaments, protects the important underlying vasculature, pleural domes, trachea, and esophagus. The SC ligaments consist of the anterior and posterior SC and capsular ligaments, the interclavicular ligaments, and the anterior and posterior costoclavicular ligaments (47,51). These allow motion in all planes, including rotation. The SC ligaments prevent upward displacement of the medial clavicle caused by downward forces on the lateral end of the clavicle. The posterior capsular ligament is the most important stabilizer (51). These ligaments allow the clavicle to move 30 degrees upward, 30 degrees in an anteroposterior direction, and rotate 45 degrees about its long axis (47,51).
Scapulothoracic Articulation
The scapulothoracic articulation is not a true joint; rather, it represents the space between the concave surface of the anterior scapula and the convex surface of the posterior chest wall. The muscular and ligamentous attachments provide the stability of this articulation as the scapula retracts, protracts, and rotates along the posterior chest wall (2,3).
Williams et al. (52) divided the anatomical structures of this articulation into three layers: superficial, intermediate, and deep. The trapezius and latissimus dorsi muscles and an inconsistent bursa between the latissimus and inferior angle of the scapula comprise the superficial layer. The intermediate layer is composed of the rhomboid major and the rhomboid minor, the levator scapulae muscles, and the spinal accessory nerve and bursa between the superomedial scapula and trapezius muscle. The spinal accessory nerve travels closely along this bursa at an average of 2.7 cm lateral to the superomedial scapular angle. Finally, the deep layer consists of the serratus anterior and subscapularis muscles and the corresponding scapulothoracic and subscapularis bursa (52,53).
Glenohumeral Joint
The GH joint is a diarthrodial joint with minimal bony constraint, allowing it the largest range of motion of any major diarthrodial joint in the body (2,3,31,54). The GH joint has been described as being similar to a golf ball on a tee, with a large humeral head balanced on a smaller glenoid. The GH joint approximates ball-and-socket kinematics, with only one-third of the humeral head being covered by the glenoid in any position of rotation, and the articular surface of the humeral head is threefold that of the glenoid (2,43,55).
In most shoulders, the glenoid and humerus have similar radii of curvature, providing a basically congruent articulation with less than 2 mm of mismatch between the glenoid and the humeral head. This matched concavity–convexity of the articulation provides stability when muscle forces act across the joint. This provides the foundation for the RTC musculature to establish a concavity–compression effect (33,54,55,56,57).
The combined version of the glenoid and humeral head results in a retroversion of approximately 30 to 40 degrees (2,28,31,57). In normal shoulders, the center of the humeral head is usually within 1 mm of the plane of the scapular spine (58). The spherical humeral articular surface articulates with the spherical concavity of the glenoid, whereas the proximal humeral convexity articulates with the spherical concavity of the coracoacromial arch (55).
A negative intra-articular pressure exists within the GH joint, creating a vacuumlike effect. The joint acts as a closed compartment with a flexible diaphragm. The weight of the arm tends to pull the joint surfaces away from each other, creating negative pressure (59,60). In addition, an adhesion–cohesion effect exists secondary to the viscous and intermolecular properties of the synovial fluid, similar to water keeping two glass surfaces together (55).
Glenoid Labrum
The glenoid labrum provides another static restraint to GH motion. The labrum is a fibrous ring attached to the glenoid articular surface through a fibrocartilagenous transition zone. The labrum functions as an anchor point for the GH ligaments and the biceps tendon; it also deepens the glenoid socket and enhances stability (2,3,39).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree