Short-stem Designs for Total Hip Arthroplasty: Neck Stabilized Femoral Components
Timothy McTighe
Declan Brazil
John M. Keggi
Louis Keppler
Edward J. McPherson
Introduction
Total hip arthroplasty (THA) is one of the most effective orthopedic procedures, providing consistently high success rates across all population segments as measured by pain relief, improved function, and patient satisfaction (1,2,3,4). While symptomatic hip arthritis typically affects older patients, this segment of the patient population is more active than it has ever been. Many septuagenarians and octogenarians maintain a vigorous lifestyle and will experience a greater longevity. In addition, THA has become an option for a growing subset of active patients aged 30 to 60 years who are affected by coxarthrosis and who were previously thought of as “too young for a hip replacement” (5,6). This cohort of patients is internet savvy and thus well informed about the treatment options for their disability. As a group, they are demanding earlier surgical intervention to restore the quality of their lifestyle (7,8).
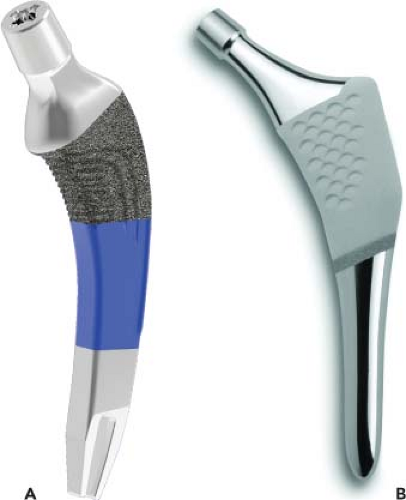
Over the past 10 years, the orthopedic community has witnessed an increased interest in more conservative surgical techniques for hip arthroplasty (9,10,11,12). During this time, second-generation hip resurfacing and minimally invasive surgery (MIS) enjoyed extensive marketing attention. After a decade of this renewed interest, both of these methods for THA have met with serious concerns (13,14,15). As hip resurfacing numbers decline, both patients and surgeons are looking for other potentially successful conservative treatments to THA. This search has recently focused surgeon interest toward short-stem designs (Fig. 64.1A,B).
Most reports on short stems have appeared as oral presentations and posters at continuing medical education (CME) meetings (16,17). The international experience precedes that of the United States by at least a decade (18,19,20). The initial response in the U.S. market was simply to modify certain current standard cementless stems by truncating the diaphyseal portion of the stem. Short-and midterm follow-up studies of a number of these stems suggest that stable, durable fixation and excellent clinical outcomes can be achieved (8,9,10,13,15,21). Today, a variety of short-stem implants are available with very little clarification of design rationale, fixation features, surgical technique, and clinical outcomes. Virtually every major implant company now offers a “short stem,” and now there are a plethora of different designs. It is important to note, however, that not all short stems achieve initial fixation at the same bone interface region. Furthermore, surgical techniques vary greatly, and postoperative radiographic interpretation of short-stem position and fixation needs to be carefully scrutinized (14,22). Finally, the surgeon who is new to short-stem technology is often
unaware of the surgical preparation difference for a short metaphyseal style stem versus a neck-persevering style stem. For example, a number of neck-preserving stems prefer rasping the medial femoral curve versus impaction broaching. This has a back-and-forth technique that cuts and shapes the bone to the rasp and final implant. The broach impacts cancellous bone into a dense material and can increase hoop tension, resulting in distal fractures in some cases.
unaware of the surgical preparation difference for a short metaphyseal style stem versus a neck-persevering style stem. For example, a number of neck-preserving stems prefer rasping the medial femoral curve versus impaction broaching. This has a back-and-forth technique that cuts and shapes the bone to the rasp and final implant. The broach impacts cancellous bone into a dense material and can increase hoop tension, resulting in distal fractures in some cases.
The purpose of this chapter is to review past, present, and potential future developments of short femoral stems and to present a classification system that can offer guidance when reporting on the many different stem variations.
Historical Review
Modern-day conservative (i.e., bone-preserving) implant designs for THA started in Europe, where surgeons have been implanting conservative devices since the introduction of the thrust plate in 1978 (23). The thrust plate closely resembles Philip Wiles’ 1938 implant, which also featured a side-plate fixation method (Fig. 64.2A,B). Fink et al. reported disappointing midterm results using the thrust plate, including higher loosening and infection rates (compared with cementless stemmed prostheses), pain over the side plate, and stress shielding that occurred under the plate (17).
Another conservative concept was the use of a short curved stem inserted into the proximal femoral neck. Many consider Professor Francesco Pipino, from Monza, Italy, to be the leading pioneer and innovator of the short curved stem. His concept was to preserve the majority of the femoral neck and insert a short curved neck-retaining stem. Pipino and Calderale (24) first presented the femoral neck-conserving Biodynamic hip prosthesis (Howmedica/Stryker Orthopaedics) for cementless fixation in 1979. This was a cobalt-chromium (CoCr) alloy stem available in four sizes with a cementless macroporous surface, a single medial curve, and one neck angle of 135 degrees (Fig. 64.3).
In 1982, Morrey from Mayo Clinic in Rochester, Minnesota, United States, designed a short (60 mm), double tapered titanium alloy proximal femoral stem with a modular head. The implant, named the Mayo stem, is described as an ultrashort, straight, multitapered component with a proximal wide trapezoidal cross section (Fig. 64.4). This basic design has not changed since it was first used in 1982. The early design featured a proximal fiber metal pad, which was the preferred technology that the manufacturer used at the time. Some other implant designs that featured this fixation method (noncircumferential porous surface) have been associated with periprosthetic osteolysis. However, the stem eventually received FDA clearance with a corundum blast (bead blast or matte) finish that replaced the porous insert pad design. Results are comparable with many cemented and cementless stems (25). The Mayo stem design has led to two additional stems that similarly reproduce its shape: the Nanos stem (Smith & Nephew) and the Metha stem (Aesculap Orthopaedics) (26). More information on these and other recently developed short stems is presented later in this chapter, as part of the section on the Joint Implant Surgery and Research Foundation (JISRF) classification system. This review does not include all the stems available worldwide but does give a good cross-sectional review.
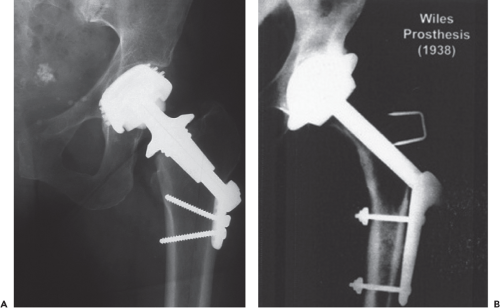 Figure 64.2. A: Thrust plate, 1978 (Zimmer, Warsaw, IN) (Picture courtesy of JISRF archives). B: Wiles 1938 Hip Plate S.S. (Manufacturer unknown). (Picture courtesy of JISRF archives.) |
 Figure 64.3. Biodynamic stem, 1979 (Howmedica, Rutherford, NJ). (Rendering courtesy of Chris Burgess.) |
Potential Advantages of Short Stems
Short stems offer numerous advantages (18,19,27,28). First, with some short-stem designs, a majority of the femoral neck is preserved. Surgically, this requires less surgical dissection and mitigates soft tissue and bone damage. Ultimately, preservation of the femoral neck provides a more natural barrier to migration of particulate debris, is associated with less blood loss and less time and energy to rehabilitate the hip, reduces stress shielding of the proximal femur (i.e., load redistribution and subsequent loss of proximal femoral bone mass), and reduces end-of-stem thigh pain. In consideration of all these aforementioned advantages, the use of a short stem can make patient rehabilitation faster and less painful. Because of its smaller size, the short stem is easier to insert, and this facilitates a more minimally invasive surgical approach. The novel design feature inherent in short-stem implants—namely, preservation of proximal native bone and tissue—theoretically affords easier revision surgery if or when it becomes necessary. For these reasons, short-stem procedures also have broader indications compared with hip resurfacing. Finally, many short-stem designs do not require many stem sizes. This translates to simplified instrumentation and reductions in requisite surgical inventory (e.g., instruments and implants). This can provide a significant net savings to healthcare facilities.
Short-Stem Technology: Principles of Stable Cementless Fixation
The biologic response of bone to stress greatly affects the outcome of cementless THA. The adaptive bone remodeling process, “Wolff’s law,” (29) should be considered when deciding on material, geometry, and size selection for cementless femoral components. Many clinical and radiologic studies have demonstrated the sensitivity of this adaptive remodeling process (1,13,15,18,30). It has been shown that trabecular microfracture and remodeling is a major mode of accelerated remodeling in response to changes in mechanical demands on the bone (27). Trabeculae that fail, either by fatigue mode or by overloading, will disappear if the ends do not contact each other and if the resulting trabeculae bear no load (disuse atrophy).
However, if the fractured trabeculae realign themselves and the fracture site still maintains control such that the structure is able to transmit load, the trabeculae will remodel in the new direction much more quickly than through the mechanism of ordered resorption and apposition. Interfaces created surgically within the structure and subsequently loaded by mechanical means result in severe overloading of the remaining cancellous structure. Cancellous bone is a poor material for structural support of a prosthesis. Cancellous bone is a biologically engineered material, and its strength depends on its having the entire bulk of the structure intact. The creation of a bone–prosthesis interface with areas of cancellous bone disproportionately weakens the structure. In addition, contacting an implant with only cancellous bone merely serves to increase the stress at the interface to a level that causes fatigue failure of the bone (31).
Through proper design and surgical technique, one can achieve significant enhancement of the mechanical properties of the prosthesis–bone biologic interface with basic biomechanical principles. It is recommended that most, if not all, of the cancellous bone be removed or impacted. Structuring the surface of an implant (i.e., adding surface roughness) will minimize the surface shear stresses. In addition, structuring will convert hoop stresses into compression stresses within the femur. For an uncemented femoral component to achieve osteointegration, it is universally agreed that initial stability is essential. In addition, there must be a surface coating to ensure long-term bony fixation (e.g., porous plasma spray with commercially pure titanium [CP-Ti], hydroxyapatite [HA] coating, or grit-blasted surface). Short-stem designs must resist subsidence, angulation, and rotation. Their decreased surface area results in increased stress per unit and consequently requires a dense cancellous or cortical interface for final seating.
The term “cementless fixation” can refer to either a press fit or a biologic surface to promote interlock with the surrounding bone structure. Circumferential porous coatings and HA have been shown to (1) provide an effective barrier to distal migration of wear debris and (2) enhance bone stability and long-term fixation (32




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree