Short-Stem Designs for Total Hip Arthroplasty: Metaphyseal-Engaging Femoral Components
S. David Stulberg
Ronak M. Patel
Introduction
Uncemented total hip arthroplasty (THA) has proven to be clinically and functionally successful in the treatment of end-stage degenerative joint disease of the hip (1,2,3,4,5,6,7,8). Uncemented implants rely on diaphyseal or metaphyseal contact, and ultimately, bone fixation to ingrowth or ongrowth surfaces to provide long-term stability and dependable clinical results (3,9,10,11,12,13,14,15,16,17,18,19). Uncemented femoral components with a variety of shapes, metallurgy, and surface treatment have been developed to address the broad spectrum of proximal femoral morphology which exists.
Successful THA relies on initial and long-term rotational and axial stability. The diaphyseal portion of the femoral implant contributes to the initial stability. This area of the stem can be cylindrical or tapered. Cylindrical, extensively porous-coated implants (e.g., AML) achieve durable fixation but can be associated with stress shielding and thigh pain. Cylindrical implants without porous-coated stems achieve varying degrees of initial axial and rotational stability through contact points in the diaphysis, but rely on metaphyseal bone contact to enhance their initial rotational stability. Furthermore, these implants seek long-term fixation and stability through bone ingrowth or ongrowth at the metaphysis. Long-term clinical results of these implants have been satisfactory and reliable with an overall lower incidence of thigh pain and proximal stress shielding relative to their extensively coated counterparts.
Tapered uncemented implants achieve primary axial fixation through a three-point contact mechanism with the creation, and ultimate relaxation of hoop stresses between a tapered stem and cylindrical femur. Rotational stability is achieved in the proximal femur through surface treatment, various shape geometries, and overall fit and fill. Secondary fixation depends on the extent of contact between the ingrowth/ongrowth surfaces of the implant and metaphyseal bone. Many studies have established the long-term clinical and radiographic reliability and durability of tapered femoral implants. These stems have been associated with relatively little thigh pain compared to cylindrical stems.
The tapered or uncoated cylindrical diaphyseal stem provides primary axial stability but varying degrees of rotational stability. Rather, rotational stability is attained from metaphyseal bone–implant contact.
Despite the success of these uncemented implant designs, varying patient factors such as size, age, level of physical activity, and bone quality present particular challenges in uncemented THA. These challenges include (1) the need for long-term fixation; (2) the preservation of proximal bone stock; (3) the potential need for effective, reliable, and safe femoral component revision; (4) the elimination of thigh pain in extremely active patients of all ages and bone quality; and (5) the ability to insert implants safely, securely, and reproducibly via specific surgical approaches such as the direct anterior approach.
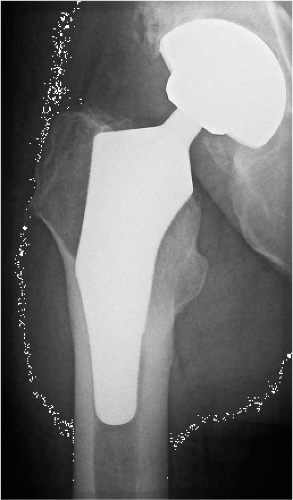
Short-stem uncemented femoral implants have been developed to address some of these challenges while maintaining the current level of success achieved by uncemented implants of conventional length (Fig. 63.1). The purposes of this chapter are to (1) describe the rationale and types of short-stem implants; (2) explain implant–bone contact points of short-stem implants of various designs and consider the effects of various types of proximal femoral contact; (3) summarize the clinical results with these implants; and (4) describe the surgical technique for successful and reproducible implantation of short-stem implants.
Design Rationale and Types of Uncemented Short-Stem Metaphyseal-Engaging Femoral Implants
Designers of short-stem metaphyseal-engaging implants theorize secure initial fixation is achieved in the metaphysis and that the axial and rotational stability provided by the diaphyseal portion of the femoral implant is negligible. Metaphyseal ingrowth or ongrowth secures long-term fixation, with the pattern of bone–implant contact varying by implant design. Although a variety
of implants have been introduced over the past few years, most implants fall into one of two categories: (1) standard neck resection (Fig. 63.2A) and (2) femoral neck sparing (Fig. 63.2B). Standard neck resection short-stem implants can further be classified into (a) anatomic and (b) wedge-fit implants. These implants also tend to be shortened versions of conventional uncemented implants. Femoral neck sparing or preserving implants instead have unique design features to accommodate the native anteversion of the femoral neck.
of implants have been introduced over the past few years, most implants fall into one of two categories: (1) standard neck resection (Fig. 63.2A) and (2) femoral neck sparing (Fig. 63.2B). Standard neck resection short-stem implants can further be classified into (a) anatomic and (b) wedge-fit implants. These implants also tend to be shortened versions of conventional uncemented implants. Femoral neck sparing or preserving implants instead have unique design features to accommodate the native anteversion of the femoral neck.
 Figure 63.3. Cross sections of osteotomy levels for standard neck versus femoral neck sparing implants designs. |
Femoral neck sparing or high-femoral neck resection designs seek to optimize proximal load transfer by engaging solely the femoral neck and the metaphysis. A more proximal and horizontal femoral neck osteotomy produces an oval-shaped intramedullary opening compared to a standard cut which offers a relatively broad opening (Fig. 63.3). Studies have shown greater resistance to torsional stresses with these high-neck osteotomies. The concept of femoral neck preservation in uncemented designs has been well described since the earliest days of arthroplasty (20,21). Proponents of this concept have suggested improved bone and soft tissue preservation. Moreover, soft tissue preservation enhances implant fixation, reduces surgical morbidity, improves abductor function and preserves bone stock for potential future surgery.
Santori et al. reported satisfactory midterm results in a high-femoral neck resection short-stem implant. They performed a complete clinical review at a mean interval of 8 years
in their cohort of patients under the age of 60 who underwent THA. Despite other encouraging results reported by the developers of uncemented femoral components inserted with high-femoral neck resection, widespread use of these devices has not yet occurred.
in their cohort of patients under the age of 60 who underwent THA. Despite other encouraging results reported by the developers of uncemented femoral components inserted with high-femoral neck resection, widespread use of these devices has not yet occurred.
A number of reasons have been proposed for the slow adoption of this concept. First, the surgical technique for inserting stems of this design is different, and potentially more difficult, than more standard neck resection approaches. The long retained femoral neck can make exposure of the acetabulum difficult. Also, accurate, reproducible alignment of the femoral stem within the diaphysis may be difficult to accomplish given the native anteversion of neck–shaft. Next, the relatively small surface area of bone at the proximal femoral neck makes restoration of accurate leg length and avoidance of lengthening of the extremity difficult to achieve. Moreover, the high-neck resection limits exposure of the metaphysis and may reduce the extent and reliability with which metaphyseal fit and contact can be achieved. Concerns have been raised that the combination of high-neck resection and short-stems may be associated with an increased incidence of proximal femoral fractures. Finally, surgeons and investigators have suggested that the use of implants inserted using a high-femoral neck resection may result in increased bone–bone impingement and a consequent reduction in range of motion. Initial experimentation with femoral neck preserving short-stem implants may have been considered a radical shift in paradigm at the time. Recent renewed interest in these stems is largely due to a natural progression of uncemented femoral components from cylindrical to tapered to shortened.
Design teams continue to develop high-neck resection implants based on encouraging results from original designs and aim to address some of the design flaws listed above (Fig. 63.4). For example, the Fitmore stem (Zimmer, Warsaw, IN) has variability in its curve to allow for greater medial calcar contact for enhanced stability (Fig. 63.5). Development of these devices is being spurred by a renewed interest in the use of the direct anterior approach for THA, the desire for surgical and implant approaches that minimize soft tissue and bone trauma, and a concern about proximal bone preservation and positive bone remodeling.
Standard neck resection short-stem implants tend to be shortened versions of commercially available conventional length uncemented femoral implants (Fig. 63.6A,B). These stems have shortened tapered or cylindrical diaphyseal-reaching stems and a wide variety of metaphyseal shapes. The two main categories of metaphyseal shapes include two- or three-dimensional taper shapes that achieve two-point wedge fixation in the metaphysis and anatomic shapes that seek to fit and fill the metaphysis. Theoretical studies have shown that the use of a lateral flare configuration reduces distal femoral stress transfer in conventional length uncemented femoral components by engaging the proximal, lateral, medial, and anterior cortices (22,23). Use of this rationale has extended into short-stem designs.
Proponents of these short-stem designs state that the proximal, metaphyseal fixation achieved will be adequate for initial and long-term stability. Various designs have shown to have reliable fixation and successful clinical and radiographic outcomes up to 8 years postoperatively. Recently, a finite element analysis was completed in a composite bone model evaluating uncemented femoral stem length on primary stability (24). No significant reduction in stability was observed from reducing stem length from 146 to 105 mm; furthermore, decreasing stem length further did not lead to
micromotion that would inhibit osteointegration (25). Arno et al. (26) completed a cadaveric evaluation of femoral strain with the use of uncemented femoral components with three different stem lengths. As the stem length increased, there was a typical pattern of increased distal strain and decreased proximal femoral strain. These authors concluded while the stemless component best matched the strain pattern in a native femur, the ultra-short implant (one-third length of standard Revelation Lateral Flare, DJO Surgical Inc., Austin, TX) performed close to the stemless design. Lack of early biomechanical data restricted initial use of short-stems to patients under the age of 60 to 70 years or in patients with Dorr Type A or B bone. Surgeons, initially, also protected weight bearing in the immediate postoperative period. Early radiographic and clinical results of uncemented short-stem femoral implants failed to show gross subsidence or instability, allowing surgeons to resume standard postoperative weight bearing and activity protocols. Two-year and midterm follow-up in short-stem implants of varying designs showed stable fixation and comparable clinical outcome scores to uncemented conventional length THA. Indications expanded to include patients older than 70 years and those with Dorr Type C bone. However, the lack of true long-term follow-up (>10 years) has prevented widespread use of these implants.
micromotion that would inhibit osteointegration (25). Arno et al. (26) completed a cadaveric evaluation of femoral strain with the use of uncemented femoral components with three different stem lengths. As the stem length increased, there was a typical pattern of increased distal strain and decreased proximal femoral strain. These authors concluded while the stemless component best matched the strain pattern in a native femur, the ultra-short implant (one-third length of standard Revelation Lateral Flare, DJO Surgical Inc., Austin, TX) performed close to the stemless design. Lack of early biomechanical data restricted initial use of short-stems to patients under the age of 60 to 70 years or in patients with Dorr Type A or B bone. Surgeons, initially, also protected weight bearing in the immediate postoperative period. Early radiographic and clinical results of uncemented short-stem femoral implants failed to show gross subsidence or instability, allowing surgeons to resume standard postoperative weight bearing and activity protocols. Two-year and midterm follow-up in short-stem implants of varying designs showed stable fixation and comparable clinical outcome scores to uncemented conventional length THA. Indications expanded to include patients older than 70 years and those with Dorr Type C bone. However, the lack of true long-term follow-up (>10 years) has prevented widespread use of these implants.
 Figure 63.4. A: Coronal view of the Mayo implant. B: Sagittal view of the Proxima implant. C: Coronal view of the Silent implant. |
Midterm follow-up has revealed acceptable pain and function as well as stability. Two-year migration analysis of a metaphyseal-anchored short-stem implant using Ein Bild Roentgen Analyse femoral component analysis shows subsidence rates and patterns of stability comparable to conventional length uncemented implants. Although long-term studies remain the gold standard in joint arthroplasty, migration analysis allows prediction of implant survival.
A proposed benefit of short-stem femoral implants is optimal proximal bone remodeling. Although roentgen stereophotogrammetric and DEXA analyses are considered gold standards in accurate measurement of bone mass surrounding a prosthesis, many authors report appreciable changes on radiographic analysis. In comparison to conventional length uncemented femoral implants, short-stem implants have less bone resorption (27). Chen et al. found an average bone loss
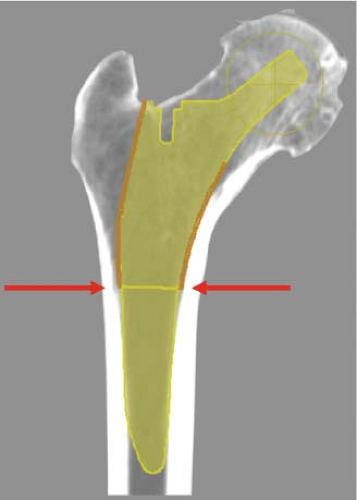
of 3.3% in DEXA analysis of the Mayo Conservative stem (Zimmer, Warsaw, IN). The average bone resorption found in the literature is 20% with an autopsy retrieval study showing 42.1% loss proximally and a gradual decline distally (28,29). Regardless of the methodology of evaluation, surgeons and implant engineers have put much focus on the design of the component. Two-point wedge designs attempt to achieve contact and fit at the metaphyseal–diaphyseal junction. Although these implants can be tapered in two or three dimensions, the wedge fit is primarily two-point at the medial and lateral cortices (Fig. 63.7). Anterior and/or posterior endosteal contact is variable on design. Similarly, anatomic implants attempt to fit and fill the metaphysis—either in the coronal or sagittal planes or both. This variability of implant design leads to variability in bone–implant contact, and ultimately, varying amounts of stability and proximal load transfer.
of 3.3% in DEXA analysis of the Mayo Conservative stem (Zimmer, Warsaw, IN). The average bone resorption found in the literature is 20% with an autopsy retrieval study showing 42.1% loss proximally and a gradual decline distally (28,29). Regardless of the methodology of evaluation, surgeons and implant engineers have put much focus on the design of the component. Two-point wedge designs attempt to achieve contact and fit at the metaphyseal–diaphyseal junction. Although these implants can be tapered in two or three dimensions, the wedge fit is primarily two-point at the medial and lateral cortices (Fig. 63.7). Anterior and/or posterior endosteal contact is variable on design. Similarly, anatomic implants attempt to fit and fill the metaphysis—either in the coronal or sagittal planes or both. This variability of implant design leads to variability in bone–implant contact, and ultimately, varying amounts of stability and proximal load transfer.
Implant–Bone Contact Points and Effects of Contact
Contact patterns in implant–bone interface have been measured in conventional implant design rationales with inconsistent endosteal contact in the metaphysis. Although short-stem implants have been designed to engage the proximal femur and optimize load transfer, there are limited data indicating what design parameters aid in fulfilling that rationale. Our center investigated this question with the aid of a CT-based workstation. Specifically, the goals of this analysis were to (1) describe the contact and fit–fill pattern of four short metaphyseal-engaging femoral implants; (2) recognize the design features that help to determine the priority contact zones on each implant design; and (3) analyze the effect of optimal bone–implant contact on femoral offset and anteversion and compare this to bone–implant contact after optimizing femoral offset and anteversion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree