CHAPTER 22 Sedation for Percutaneous Procedures
INTRODUCTION
‘Sedation and analgesia’ describe a state in which patients can tolerate unpleasant procedures while maintaining cardiac and respiratory function and still maintain the ability to respond purposefully to both verbal commands and tactile stimulation. The Task Force on sedation and analgesia decided that the term ‘sedation and analgesia’ (sedation/analgesia) more accurately defines this therapeutic goal than does the commonly used but imprecise term ‘conscious sedation.’ This level of sedation does not include a level in which the only intact reflex is withdrawal from a painful stimulus.1 Although sedation has been described as ‘light sleep’2 and textbooks note that ‘the terms sleep, hypnosis, and unconsciousness are used interchangeably in anesthesia literature to refer to the state of drug-induced sleep,’3 pharmacological sedation is not the same as physiological sleep.
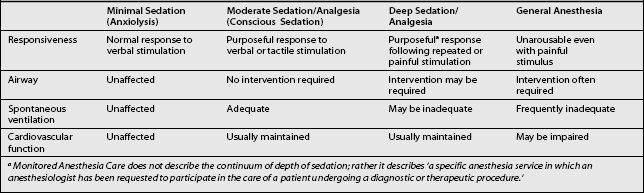
LEVELS OF SEDATION
Deep sedation and general anesthesia are not usually recommended for most of pain management procedures, as an awake, cooperative patient is needed to prevent complications related to nerve injury, allergic reactions, or medication toxicity (Table 22.2).
Table 22.2 Ramsay Level of Sedation Scale2
| Clinical Score | Level of Sedation Achieved |
|---|---|
| 6 | Asleep, no response |
| 5 | Asleep, sluggish response to light glabellar tap or loud auditory stimulus |
| 4 | Asleep, but with brisk response to light glabellar tap or loud auditory stimulus |
| 3 | Sleepy, but responds to commands |
| 2 | Patient cooperative, oriented and tranquil |
| 1 | Patient anxious, agitated or restless |
GENERAL PREPARATION
Preprocedural assessment
All patients who are scheduled to receive sedation should be thoroughly evaluated prior to the procedure. Relevant issues that should be addressed include past medical history, past surgical history to include any anesthetic complications, drug allergies, and current medications to include anticoagulants, smoking, alcohol use and recreational drug history, and NPO status. The risk stratification classification of the American Society of Anesthesiologists (ASA) provides an excellent preprocedure assessment tool for this purpose (Table 22.3).
Table 22.3 American Society of Anesthesiologist Physical Class Risk Stratification
| Class I | Normal healthy patient |
| Class II | Mild systemic disease |
| Class III | Severe systemic disease |
| Class IV | Life-threatening illness |
| Class V | Moribund patient |
Table 22.4 provides a summary of the American Society of Anesthesiologists preprocedure fasting guidelines. The recommendations apply to healthy patients who are undergoing elective procedures. They are not intended for women in labor. Following the guidelines does not guarantee complete gastric emptying has occurred.
Table 22.4 Summary of American Society of Anesthesiologists Preprocedure Fasting Guidelines for Healthy Patients Who Are Undergoing Elective Procedures
| Ingested Material | Minimum Fasting Period |
|---|---|
| Clear liquids | 2 h |
| Nonhuman milk | 6 h |
| Light meal | 6 h |
The fasting periods noted in Table 22.4 apply to all ages.
Examples of clear liquids include water, fruit juices without pulp, carbonated beverages, clear tea, and black coffee.
Since nonhuman milk is similar to solids in gastric emptying time, the amount ingested must be considered when determining an appropriate fasting period.
A light meal typically consists of toast and clear liquids. Meals that include fried or fatty foods or meat may prolong gastric emptying time. Both the amount and types of foods ingested must be considered when determining an appropriate fasting period.
Airway assessment procedures for sedation and analgesia
The airway should be evaluated prior to giving sedative medications. Oversedation will cause respiratory depression and may require respiratory support. Oversedation can also cause aspiration, obstruction, bronchospasm, and laryngospasm requiring tracheal intubation and ventilatory support. Intubation may be especially difficult in patients with atypical airway anatomy. Airway abnormalities may also increase the likelihood of airway obstruction following the administration of sedatives and analgesics. Warning signs of a difficult airway are listed in Table 22.5. Recommendations for frequency of monitoring and documentation during sedation/analgesia are listed in Table 22.6.
Table 22.5 Warning Signs of a Difficult Airway
| Previous problems with sedation |
| Stridor, snoring, or sleep apnea |
| Advanced rheumatoid arthritis |
| Chromosomal abnormality (e.g. trisomy 21) |
| Significant obesity (especially involving the neck and facial structures) |
| Short neck and limited neck extension |
| Decreased hyoid-mental distance (<3 cm in an adult) |
| Neck or anterior mediastinal mass |
| Cervical spine disease or trauma |
| Tracheal deviation |
| Dysmorphic facial features (e.g. Pierre–Robin syndrome) |
| Small opening (< 3 cm in an adult) |
| Edentulous |
| Protruding incisors |
| Loose or capped teeth |
| Dental appliances |
| High, arched palate |
| Macroglossia |
| Tonsillar hypertrophy |
| Nonvisible uvula |
| Micrognathia |
| Retrognathia |
| Trismus and significant malocclusion |
Table 22.6 Recommendations for Frequency of Monitoring and Documentation During Sedation/Analgesia1
| Monitoring | Conscious Sedation | Deep Sedation |
|---|---|---|
| Heart rate | Continuous | Continuous |
| Oxygen saturation | Continuous | Continuous |
| Respiratory rate | Minimum of every 15 min | Minimum of every 5 min |
| Noninvasive blood pressure | Minimum of every 15 min | Minimum of every 5 min |
| Level of consciousness | Minimum of every 5 min | Minimum of every 5 min |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree