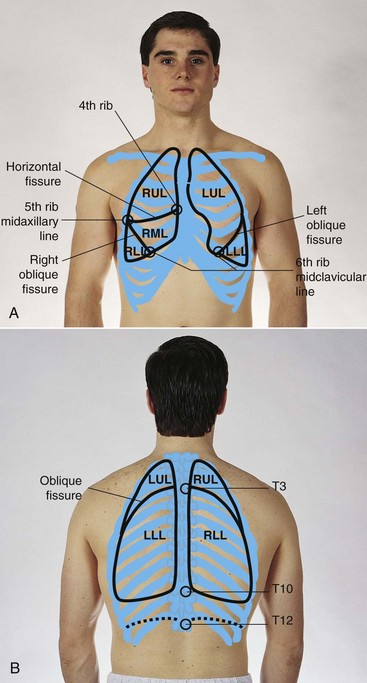
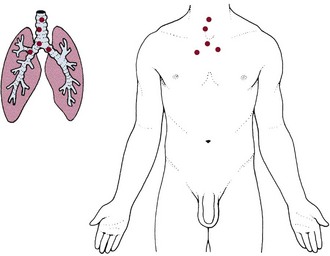
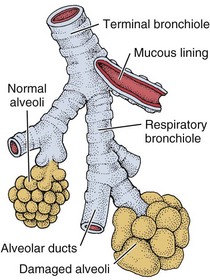
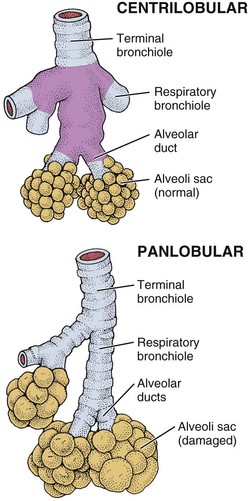
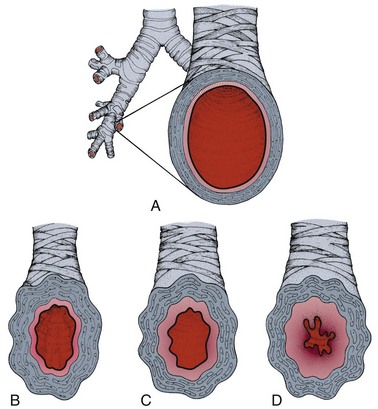
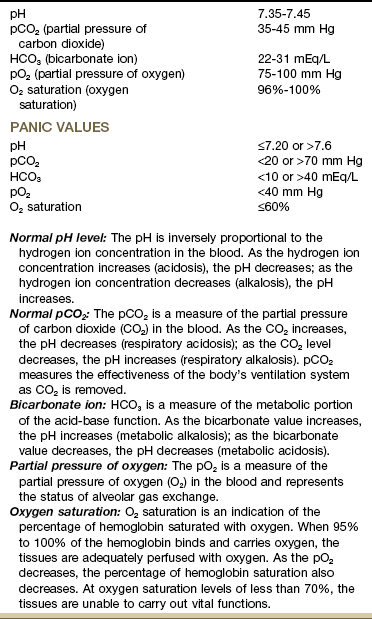
Chapter 7 The material in this chapter will assist the therapist in treating both the client with a known pulmonary problem and the client with musculoskeletal signs and symptoms that may have an underlying systemic basis (Case Example 7-1). Thickening and widening of the terminal phalanges of the fingers and toes result in a painless clublike appearance recognized by the loss of the angle between the nail and the nail bed (see Figs. 4-36 and 4-37). Conditions that chronically interfere with tissue perfusion and nutrition may cause clubbing, including cystic fibrosis (CF), chronic obstructive pulmonary disease (COPD), lung cancer, bronchiectasis, pulmonary fibrosis, congenital heart disease, and lung abscess. Most of the time, clubbing is due to pulmonary disease and resultant hypoxia (diminished availability of blood to the body tissues), but clubbing can be a sign of heart disease, peripheral vascular disease, and disorders of the liver and gastrointestinal tract. Changes in the rate, depth, regularity, and effort of breathing occur in response to any condition affecting the pulmonary system. Breathing patterns can vary, depending on the neuromuscular or neurologic disease or trauma (Box 7-1). Breathing pattern abnormalities seen with head trauma, brain abscess, diaphragmatic paralysis of chest wall muscles and thorax (e.g., generalized myopathy or neuropathy), heat stroke, spinal meningitis, and encephalitis can include apneustic breathing, ataxic breathing, or Cheyne-Stokes respiration (CSR). Exercise may induce pleural pain, coughing, hemoptysis, SOB, and/or other abnormal changes in breathing patterns. When asked if the client is ever short of breath, the individual may say “no” because he or she has reduced activity levels to avoid dyspnea (see Appendix B-12). The most common sites for referred pain from the pulmonary system are the chest, ribs, upper trapezius, shoulder, and thoracic spine. The first symptoms may not appear until the client’s respiratory system is stressed by the addition of exercise during physical therapy. On the other hand, the client may present with what appears to be primary musculoskeletal pain in any one of those areas. Auscultation may reveal the first signs of pulmonary distress (see Chapter 4 for screening examination by auscultation). Pulmonary pain patterns are usually localized in the substernal or chest region over involved lung fields that may include the anterior chest, side, or back (Fig. 7-1). However, pulmonary pain can radiate to the neck, upper trapezius muscle, costal margins, thoracic back, scapulae, or shoulder. Shoulder pain may radiate along the medial aspect of the arm, mimicking other neuromuscular causes of neck or shoulder pain (see Fig. 7-10). Pleural irritation then results in sharp, localized pain that is aggravated by any respiratory movement. Clients usually note that the pain is alleviated by autosplinting, that is, lying on the affected side, which diminishes the movement of that side of the chest (see further discussion of pleural pain in this chapter).1 Within the pulmonary system, the trachea and large bronchi are innervated by the vagus trunks, whereas the finer bronchi and lung parenchyma appear to be free of pain innervation. Tracheobronchial pain is referred to sites in the neck or anterior chest at the same levels as the points of irritation in the air passages (Fig. 7-2). This irritation may be caused by inflammatory lesions, irritating foreign materials, or cancerous tumors. Stimulation of the peripheral portions of the diaphragmatic pleura results in sharp pain felt along the costal margins, which can be referred to the lumbar region by the lower thoracic somatic nerves. Stimulation of the central portion of the diaphragmatic pleura results in sharp pain referred to the upper trapezius muscle and shoulder on the ipsilateral side of the stimulation (see Figs. 3-4 and 3-5). The blood test used most often to measure the effectiveness of ventilation and oxygen transport is the arterial blood gas (ABG) test (Table 7-1). The measurement of arterial blood gases is important in the diagnosis and treatment of ventilation, oxygen transport, and acid-base problems. TABLE 7-1 *Modified from Chernecky C, Berger B: Laboratory tests and diagnostic procedures, ed 5, Philadelphia, 2008, WB Saunders. Although bronchitis, emphysema, and asthma may occur in a “pure form,” they most commonly coexist. For example, adult subjects with active asthma are as much as 12 times more likely to acquire COPD over time than subjects with no active asthma.2–5 COPD is a leading cause of morbidity and mortality among cigarette smokers. Other factors predisposing to COPD include air pollution; occupational exposure to aerosol pesticides, irritating dusts or gases, or art materials (e.g., paint, glass, ceramics, sculpture); hereditary factors; infection; allergies; aging; and potentially harmful drugs and chemicals.6 COPD rarely occurs in nonsmokers; however, only a minority of cigarette smokers develop symptomatic disease, suggesting that genetic factors or other underlying predisposition may contribute to the development of COPD.7 In all forms of COPD, narrowing of the airways obstructs airflow to and from the lungs (Table 7-2). This narrowing impairs ventilation by trapping air in the bronchioles and alveoli. The obstruction increases the resistance to airflow. The severity of symptoms depends on how much of the lungs have been damaged or destroyed. TABLE 7-2 Respiratory Diseases: Summary of Differences COPD develops earlier in life than is usually recognized, making it the most underdiagnosed and undertreated pulmonary disease. Smoking cessation is the only intervention shown to slow decline in lung function. Identifying risk factors and recognizing early signs and symptoms of COPD increases the affected individual’s chances of reduced morbidity through early intervention.6 Acute: Acute bronchitis is an inflammation of the trachea and bronchi (tracheobronchial tree) that is self-limiting and of short duration with few pulmonary signs. This condition may result from chemical irritation (e.g., smoke, fumes, gas) or may occur with viral infections such as influenza, measles, chickenpox, or whooping cough. Chronic: Chronic bronchitis is a condition associated with prolonged exposure to nonspecific bronchial irritants and is accompanied by mucus hypersecretion and structural changes in the bronchi (large air passages leading into the lungs). This irritation of the tissue usually results from exposure to cigarette smoke or long-term inhalation of dust or air pollution and causes hypertrophy of mucus-producing cells in the bronchi. In bronchitis, partial or complete blockage of the airways from mucus secretions causes insufficient oxygenation in the alveoli (Fig. 7-3). The swollen mucous membrane and thick sputum obstruct the airways, causing wheezing, and the client develops a cough to clear the airways. The clinical definition of a person with chronic bronchitis is anyone who coughs for at least 3 months per year for 2 consecutive years without having had a precipitating disease. Bronchiectasis: Bronchiectasis is a form of obstructive lung disease that is actually a type of bronchitis. It is a progressive and chronic pulmonary condition that occurs after infections such as childhood pneumonia or CF. All pulmonary irritants, especially cigarette smoke, should be avoided. Postural drainage, adequate hydration, good nutrition, and bronchodilator therapy in bronchospasm are important components in treatment. Antibiotics are used during disease exacerbations (e.g., increased cough, purulent sputum, hemoptysis, malaise, and weight loss). The use of immunomodulatory therapy to alter the host response directly and thereby reduce tissue damage is under investigation.8,9 Emphysema: Emphysema may develop in a person after a long history of chronic bronchitis in which the alveolar walls are destroyed, leading to permanent overdistention of the air spaces and loss of normal elastic tension in the lung tissue. Types of Emphysema: There are three types of emphysema. Centrilobular emphysema (Fig. 7-4), the most common type, destroys the bronchioles, usually in the upper lung regions. Inflammation develops in the bronchioles, but usually the alveolar sac remains intact. Clinical Signs and Symptoms: The irreversible destruction reduces elasticity of the lung and increases the effort to exhale trapped air, causing marked dyspnea on exertion later progressing to dyspnea at rest. Cough is uncommon. Lung volume reduction surgery is available for some individuals and improves not only lung function and exercise performance, but also activities of daily function and quality of life.10,11 Asthma and other atopic disorders are the result of complex interactions between genetic predisposition and multiple environmental influences. The marked increase in asthma prevalence in the last 3 decades suggests environmental factors as a key contributor in the process of allergic sensitization.12 Fifteen million persons of all ages are affected by asthma in the United States. This represents a 61% increase over the last 15 years with a 45% increase in mortality during the last decade. Women are affected more than men, accounting for about 60% of the nearly 18 million cases of adult asthma. Hormones are thought to be a possible cause for this increase in incidence in women.13 The lungs become hyperreactive, responding to allergens and other irritants in an exaggerated way. This hyperresponsiveness causes the muscles of the airways to constrict, making breathing more difficult (Fig. 7-5). The second component is inflammation, which causes the air passages to swell and the cells lining the passages to produce excess mucus, further impairing breathing. EIA or hyperventilation-induced asthma potentially can be prevented by exercising in a moist, humid environment and by grading exercise according to client tolerance using diaphragmatic breathing. Any type of sustained running or cycling or activity in the cold is more likely to precipitate EIA (Box 7-2). Complications: Status asthmaticus is a severe, life-threatening complication of asthma. With severe bronchospasm the workload of breathing increases five to ten times, which can lead to acute cor pulmonale. When air is trapped, a severe paradoxic pulse develops as venous return is obstructed. This condition is seen as a blood pressure drop of more than 10 mm Hg during inspiration. Medical treatment for the underlying inflammation and resulting airway obstruction is with antiinflammatory agents and bronchodilators to prevent, interrupt, or terminate ongoing inflammatory reactions in the airways. A new class of antiinflammatory agents known as leukotriene modifiers works by blocking the activity of chemicals called leukotrienes, which are involved in airway inflammation. Reducing, eliminating, and avoiding allergens or triggers are important in self-care (see Box 7-2).
Screening for Pulmonary Disease
Signs and Symptoms of Pulmonary Disorders
Clubbing (see Chapter 4)
Altered Breathing Patterns
Pulmonary Pain Patterns
Tracheobronchial Pain
Diaphragmatic Pleural Pain
Pulmonary Physiology
Acid-Base Regulation
Pulmonary Pathophysiology
Chronic Obstructive Pulmonary Disease
Disease
Primary Area Affected
Results
Bronchitis
Membrane lining bronchial tubes
Inflammation of lining
Bronchiectasis
Bronchial tubes (bronchi or air passages)
Bronchial dilation with inflammation
Pneumonia
Alveoli (air sacs)
Causative agent invades alveoli with resultant outpouring from lung capillaries into air spaces and continued healing process
Emphysema
Air spaces beyond terminal bronchioles (small airways)
Breakdown of alveolar walls; air spaces enlarged
Asthma
Bronchioles (small airways)
Bronchioles obstructed by muscle spasm, swelling of mucosa, thick secretions
Cystic fibrosis
Bronchioles
Bronchioles become obstructed and obliterated. Later, larger airways become involved. Plugs of mucus cling to airway walls, leading to bronchitis, bronchiectasis, atelectasis, pneumonia, or pulmonary abscess
Inflammatory/Infectious Disease
Immune Sensitization and Inflammation
Clinical Signs and Symptoms