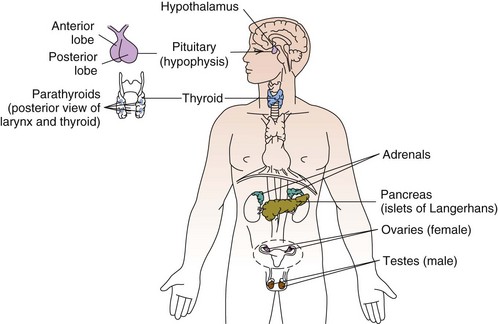
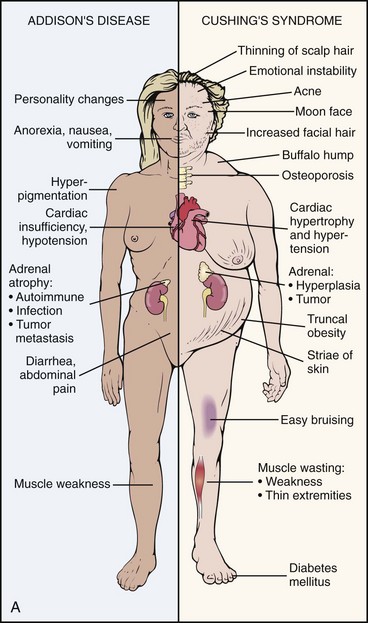
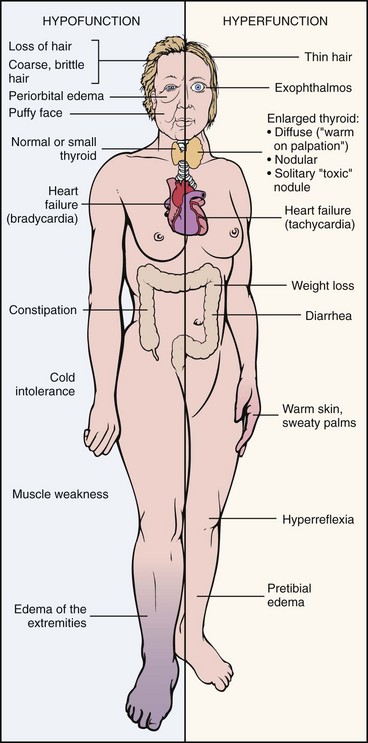
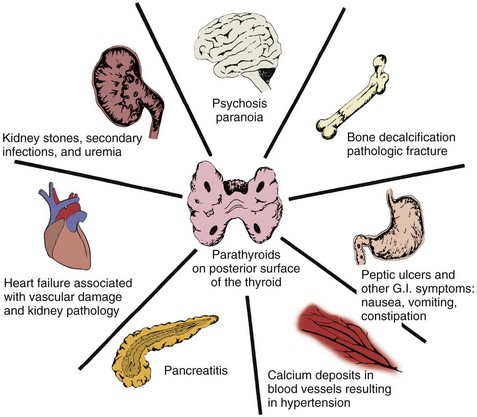
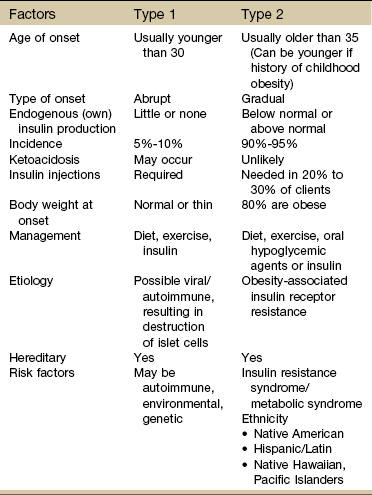
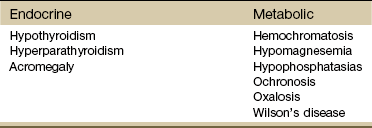
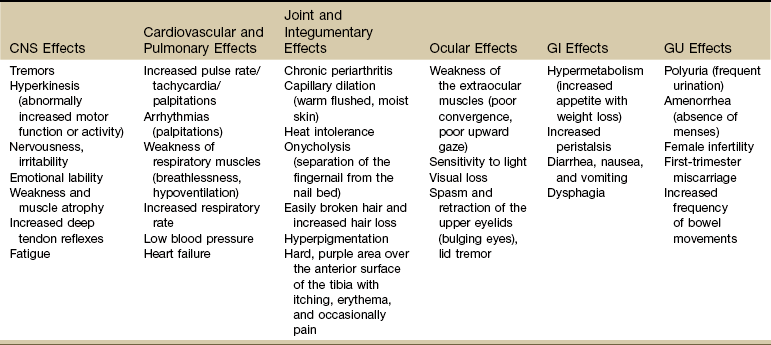
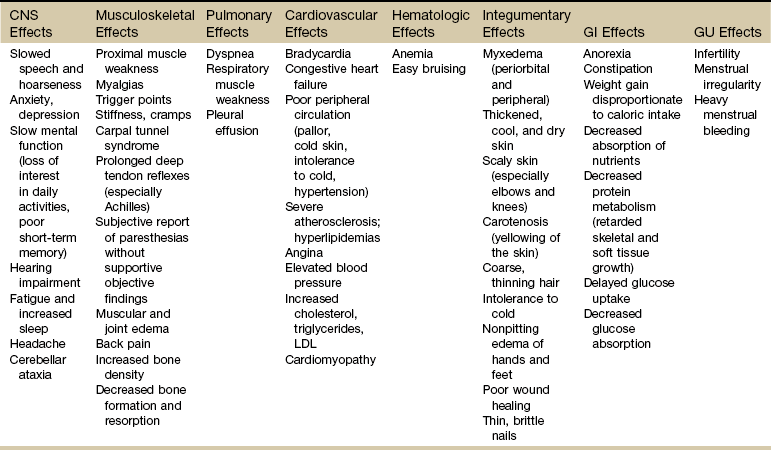
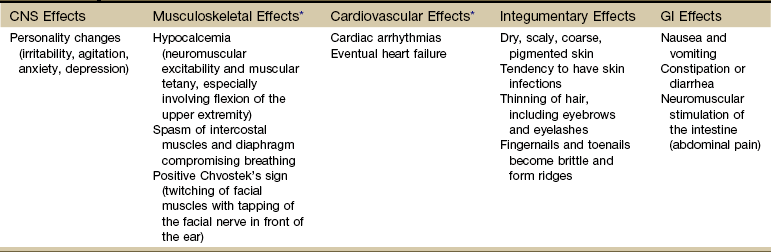
Chapter 11 The endocrine system is slower in response and takes longer to act than the nervous system in transferring biochemical information. The pituitary (hypophysis), thyroid, parathyroids, adrenals, and pineal are glands of the endocrine system whose functions are solely endocrine related and have no other metabolic functions (Fig. 11-1). The hypothalamus controls pituitary function and thus has an important indirect influence on the other glands of the endocrine system. Feedback mechanisms exist to keep hormones at normal levels. The musculoskeletal system is composed of a variety of connective tissue structures in which normal growth and development are influenced strongly and sometimes controlled by various hormones and metabolic processes. Alterations in these control systems can result in structural changes and altered function of various connective tissues, producing systemic and musculoskeletal signs and symptoms (Table 11-1). TABLE 11-1 Signs and Symptoms of Endocrine Dysfunction From Goodman CC, Fuller KS: Pathology: implications for the physical therapist, ed 3, Philadelphia, 2009, WB Saunders. Bilateral carpal tunnel syndrome (CTS), resulting from median nerve compression at the wrist, is a common finding in a variety of systemic and neuromusculoskeletal conditions1–3 but especially with certain endocrine and metabolic disorders (Table 11-2).4 The fact that the majority of persons with CTS are women at or near menopause suggests that the soft tissues about the wrist could be affected in some way by hormones.5–8 TABLE 11-2 Causes of Carpal Tunnel Syndrome *The role of repetitive activities and occupational factors (e.g., hand use of any type and keyboard or computer work in particular) has been questioned as a direct cause of carpal tunnel syndrome (CTS) and remains under investigation; sufficient evidence to implicate hand use of any type linked with CTS remains unproven.3,4 Modified from Goodman CC, Fuller K: Pathology: implications for the physical therapist, ed 3, Philadelphia, 2009, Saunders. The signs and symptoms often associated with CTS include paresthesia, tingling, and numbness and/or pain (or burning pain) with cutaneous distribution of the median nerve to the thumb, index, middle, and radial half of the ring finger. Nocturnal paresthesia is a common complaint, and this discomfort causes sleep disruption. It can be partially relieved by shaking of the hand or changing wrist and hand position. Pain may radiate into the palm and up the forearm and arm.9 It should be noted that bilateral tarsal syndrome affecting the feet also can occur either alone or in conjunction with CTS, although the incidence of tarsal tunnel syndrome is not high (see further discussion of tarsal tunnel syndrome in relation to carpal tunnel syndrome in Chapter 9). Bilateral median nerve neuritis can be characteristic of many systemic diseases, including rheumatoid arthritis, myxedema, localized amyloidosis, sarcoidosis, and infiltrative leukemia.10,11 Whenever a client presents with bilateral symptoms, it represents a red flag. With bilateral CTS the therapist can screen for medical disease by using the Special Questions to Ask: Bilateral Carpal Tunnel Syndrome section (see Appendix B-4). Chondrocalcinosis is the deposition of calcium salts in the cartilage of joints. When accompanied by attacks of gout-like symptoms, it is called pseudogout. Chondrocalcinosis is commonly seen on x-ray films as calcified hyaline or fibrous cartilage. There is an associated underlying endocrine or metabolic disease in approximately 5% to 10% of individuals with chondrocalcinosis (Table 11-3). TABLE 11-3 Endocrine and Metabolic Disorders Associated with Chondrocalcinosis Modified from Louthrenoo W, Schumacher HR: Musculoskeletal clues to endocrine or metabolic disease, J Musculoskel Med 7(9):41, 1990. Risk Factors: Risk factors for the development of SIADH include pituitary damage caused by infection, trauma, or neoplasm; secretion of vasopressin-like substances from some types of malignant tumors (particularly pulmonary malignancies); and thoracic pressure changes from compression of pulmonary or cardiac pressure receptors, or both. Clinical Presentation: Symptoms of SIADH are the clinical opposite of symptoms of DI. They are the result of water retention and the subsequent dilution of sodium in the blood serum and body cells. Neurologic and neuromuscular signs and symptoms predominate and are directly related to the swelling of brain tissue and sodium changes within neuromuscular tissues. Clinical Presentation: Degenerative arthropathy may be seen in the peripheral joints of a client with acromegaly, most frequently attacking the large joints. On x-ray studies, osteophyte formation may be seen, along with widening of the joint space because of increased cartilage thickness. In late-stage disease, joint spaces become narrowed, and occasionally chondrocalcinosis may be present. Myopathy in people with acromegaly is commonly reported but poorly understood. Changes in muscle size and strength are associated with acromegaly and are probably multifactorial in origin. Screening individuals with acromegaly for muscle weakness and poor exercise tolerance is now recommended.12 DISH (also known as Forestier’s disease) is characterized by abnormal ossification of the ALL, resulting in an x-ray image of large osteophytes seemingly “flowing” along the anterior border of the spine. DISH is particularly common in the thoracic spine and has been reported to be more prevalent among persons with diabetes than among the nondiabetic population. DISH appears to be an age-related predisposition to ossification of tendon, joint capsule, and ligamentous attachments. Identification of the presence of DISH syndrome prior to surgery is important in the prevention of heterotropic bone formation.13 Primary Adrenal Insufficiency: Chronic adrenocortical insufficiency (hyposecretion by the adrenal glands) may be primary or secondary. Primary adrenal insufficiency is also referred to as Addison’s disease (hypofunction), named after the physician who first studied and described the associated symptoms. It can be treated by the administration of exogenous cortisol (one of the adrenocortical hormones). Secondary Adrenal Insufficiency: Secondary adrenal insufficiency refers to a dysfunction of the gland because of insufficient stimulation of the cortex owing to a lack of pituitary ACTH. Causes of secondary disease include tumors of the hypothalamus or pituitary, removal of the pituitary, or rapid withdrawal of corticosteroid drugs. Clinical manifestations of secondary disease do not occur until the adrenals are almost completely nonfunctional and are primarily related to cortisol deficiency only. Cushing’s syndrome (hyperfunction of the adrenal gland) is a general term for increased secretion of cortisol by the adrenal cortex. When corticosteroids are administered externally, a condition of hypercortisolism called iatrogenic Cushing’s syndrome occurs, producing a group of associated signs and symptoms. Hypercortisolism caused by excess secretion of ACTH (e.g., from pituitary stimulation) is called ACTH-dependent Cushing’s syndrome.14 Therapists often treat people who have developed Cushing’s syndrome after these clients have received large doses of cortisol (also known as hydrocortisone) or cortisol derivatives (e.g., dexamethasone) for a number of inflammatory disorders (Case Example 11-1). Effects of Cortisol on Connective Tissue: Overproduction of cortisol or closely related glucocorticoids by abnormal adrenocortical tissue leads to a protein catabolic state. This overproduction causes liberation of amino acids from muscle tissue. The resultant weakened protein structures (muscle and elastic tissue) cause a protuberant abdomen, poor wound healing, generalized muscle weakness, and marked osteoporosis (demineralization of bone causing reduced bone mass), which is made worse by an excessive loss of calcium in the urine. Obesity, diabetes, polycystic ovarian syndrome, and other metabolic/endocrine problems can resemble Cushing’s syndrome. It is important to recognize critical indicators of this particular disorder, such as excessive hair growth, moonface, mood disorders, and increased muscle weakness, as indicators for further endocrine diagnostic testing.15 Genetics plays a role in thyroid disease. A family history of thyroid disease is a risk factor. Age and gender are also factors; most cases occur after age 50. Women are more likely than men to develop thyroid dysfunction.15 Data gathered on the medical history of the orthopedic physical therapy outpatient population indicate a 7% incidence of thyroid disease in the female population.16 The risk of having thyroid diseases increases with age, but in people older than 60 years of age, it becomes more difficult to detect because it masquerades as other problems such as heart disease, depression, or dementia. Fatigue and weakness may be the first symptoms among older adults, often mistaken or attributed to normal aging. New-onset depression in the older adult population and anxiety syndromes are also symptoms that can indicate thyroid dysfunction.17 Thyroiditis is an inflammation of the thyroid gland. Causes can include infection and autoimmune processes. The most common form of this problem is a chronic thyroiditis called Hashimoto’s thyroiditis. This condition affects women more frequently than men and is most often seen in the 30- to 50-year-old age group. Destruction of the thyroid gland from this condition can cause eventual hypothyroidism (Case Example 11-2). Clinical Presentation: Excessive thyroid hormone creates a generalized elevation in body metabolism. The effects of thyrotoxicosis occur gradually and are manifested in almost every system (Fig. 11-3 and Table 11-4). TABLE 11-4 Systemic Manifestations of Hyperthyroidism CNS, Central nervous system; GI, gastrointestinal; GU, genitourinary. In more than 50% of adults older than 70, three common signs are tachycardia, fatigue, and weight loss. In clients younger than 50, clinical signs and symptoms found most often include tachycardia, hyperactive reflexes, increased sweating, heat intolerance, fatigue, tremor, nervousness, polydipsia, weakness, increased appetite, dyspnea, and weight loss.18 Chronic periarthritis is also associated with hyperthyroidism. Inflammation that involves the periarticular structures, including the tendons, ligaments, and joint capsule, is termed periarthritis. The syndrome is associated with pain and reduced range of motion. Calcification, whether periarticular or tendinous, may be seen on x-ray studies. Both periarthritis and calcific tendinitis occur most often in the shoulder, and both are common findings in clients who have endocrine disease (Case Example 11-3). Thyroid Storm: Life-threatening complications with hyperthyroidism are rare but still important for the therapist to recognize. Unrecognized disease, untreated disease, or incorrect treatment can result in a condition called thyroid storm. In addition, precipitating factors, such as trauma, infection, or surgery, can turn well-controlled hyperthyroidism into a thyroid storm. Risk Factors: Women are 10 times more likely than men to have hypothyroidism. More than 10% of women over age 65 and 15% over age 70 are diagnosed with this disorder. Risk factors include surgical removal of the thyroid gland, external irradiation, and some medications (e.g., lithium, amiodarone). Clinical Presentation: As with all disorders affecting the thyroid and parathyroid glands, clinical signs and symptoms affect many systems of the body (Table 11-5). Because the thyroid hormones play such an important role in the body’s metabolism, lack of these hormones seriously upsets the balance of body processes. TABLE 11-5 Systemic Manifestations of Hypothyroidism CNS, Central nervous system; LDL, low-density lipoprotein; GI, gastrointestinal; GU, genitourinary. Ichthyosis, or dry scaly skin (resembling fish scales; the word ichthyosis is derived from the Latin word ichthus, which means “fish”), may be an inherited dermatologic condition (Fig. 11-4). It may also be the result of a thyroid condition. It must not be assumed that clients who present with this condition are merely in need of better hydration or regular use of skin lotion. A medical referral is needed to rule out underlying pathology. Myxedema: A characteristic sign of hypothyroidism and more rarely associated with hyperthyroidism (Graves’ disease) is myxedema (often used synonymously with hypothyroidism). Myxedema is a result of an alteration in the composition of the dermis and other tissues, causing connective tissues to be separated by increased amounts of mucopolysaccharides and proteins. This mucopolysaccharide-protein complex binds with water, causing a nonpitting, boggy edema, especially around the eyes, hands, and feet and in the supraclavicular fossae (Case Example 11-4). The binding of this protein-mucopolysaccharide complex causes thickening of the tongue and the laryngeal and pharyngeal mucous membranes. This results in hoarseness and thick, slurred speech, which are also characteristic of untreated hypothyroidism. Neuromuscular Symptoms: Neuromuscular symptoms are among the most common manifestations of hypothyroidism. Flexor tenosynovitis with stiffness often accompanies CTS in people with hypothyroidism. CTS can develop before other signs of hypothyroidism become evident. It is thought that this CTS arises from deposition of myxedematous tissue in the carpal tunnel area. Acroparesthesias may occur as a result of median nerve compression at the wrist. The paresthesias are almost always located bilaterally in the hands. Most clients do not require surgical treatment because the symptoms respond to thyroid replacement. Characteristically, the muscular complaints of the client with hypothyroidism are aches and pains and cramps or stiffness. Involved muscles are particularly likely to develop persistent myofascial trigger points (TrPs). Of particular interest to the therapist is the concept that clinically any compromise of the energy metabolism of muscle aggravates and perpetuates TrPs. Treatment of the underlying hypothyroidism is essential in eliminating the TrPs,19 but new research also supports the need for soft tissue treatment to achieve full recovery.20 There appears to be an association between hypothyroidism and fibromyalgia syndrome (FMS). Individuals with FMS and clients with undiagnosed myofascial symptoms may benefit from a medical referral for evaluation of thyroid function.21–24 Risk factors for thyroid cancer include female gender, age over 40 years, Caucasian race, iodine deficiency, family history of thyroid cancer, and being exposed to radioactive iodine (I-131), especially as children. In addition, nuclear power plant fallout could expose large numbers of people to I-131 and subsequent thyroid cancer. The use of potassium iodide (KI) can protect the thyroid from the adverse effects of I-131 and is recommended to be made available in areas of the country near nuclear power plants in case of nuclear fallout.25 The initial manifestation in adults and especially in children is a palpable lymph node or nodule in the neck lateral to the sternocleidomastoid muscle in the lower portion of the posterior triangle overlying the scalene muscles26 (Fig. 11-5). Symptoms of hyperparathyroidism are related to this release of bone calcium into the bloodstream. This causes demineralization of bone and subsequent loss of bone strength and density. At the same time, the increase of calcium in the bloodstream can cause many other problems within the body, such as renal stones. The incidence of hyperparathyroidism is highest in postmenopausal women.27 The major cause of primary hyperparathyroidism is a tumor of a parathyroid gland, which results in the autonomous secretion of PTH. Renal failure, another common cause of hyperparathyroidism, causes hypocalcemia and stimulates PTH production. Hyperplasia of the gland occurs as it attempts to raise the blood serum calcium levels. Thiazide diuretics (used for hypertension) and lithium carbonate (used for some psychiatric problems) can exacerbate or even cause hyperparathyroid disorders.28 Clinical Presentation: Many systems of the body are affected by hyperparathyroidism (Table 11-6). Proximal muscle weakness and fatigability are common findings and may be secondary to a peripheral neuropathic process. Myopathy of respiratory muscles with associated respiratory involvement often goes unnoticed. Striking reversal of muscle weakness and atrophy occur with successful treatment of the underlying hyperparathyroidism. TABLE 11-6 Systemic Manifestations of Hyperparathyroidism CNS, Central nervous system; GI, gastrointestinal; GU, genitourinary. Other symptoms associated with hyperparathyroidism are muscle weakness, loss of appetite, weight loss, nausea and vomiting, depression, and increased thirst and urination (Case Example 11-5). Hyperparathyroidism can also cause GI problems, pancreatitis, bone decalcification, and psychotic paranoia (Fig. 11-6). Clinical Presentation: Hypocalcemia occurs when the parathyroids become inactive. The resultant deficiency of calcium in the blood alters the function of many tissues in the body. These altered functions are described by the systemic manifestations of signs and symptoms associated with hypoparathyroidism (Table 11-7). TABLE 11-7 Systemic Manifestations of Hypoparathyroidism CNS, Central nervous system; GI, gastrointestinal. *The most common and important effects for the therapist to be aware of are the musculoskeletal and cardiovascular effects. The pancreas has dual functions. It acts as both an endocrine gland, secreting the hormones insulin and glucagon, and an exocrine gland, producing digestive enzymes. Disorders of endocrine function are included in this chapter, whereas disorders of exocrine function affecting digestion are included in Chapter 8. Diabetes is the leading cause of end-stage renal disease (ESRD) [kidney failure requiring dialysis or transplantation], nontraumatic lower extremity amputations, and new cases of blindness among adults in the United States, and a major cause of heart disease and stroke.29,30 Type 1 DM is a condition in which little or no insulin is produced. It occurs in about 10% of all cases and usually occurs in children or young adults. Type 2 DM commonly occurs after age 40 and is a condition of defective insulin and/or impaired cell receptor binding of insulin. Table 11-8 depicts the major differences between type 1 and type 2 in presentation and treatment. There has been some discussion as to whether Alzheimer’s disease is type 3 diabetes (“brain diabetes”), unique to the brain or if diabetes is just a risk factor for Alzheimer’s disease.31 A relationship between DM and dementia is undeniable, with numerous studies concluding that DM increases the risk of cognitive decline and dementia, including Alzheimer’s disease.32 Native Americans, Latino Americans, Native Hawaiians, and some Asian Americans and Pacific Islanders have been identified at particularly high risk for type 2 DM and its complications.33 Lack of exercise and obesity are two major risk factors for type 2 DM. As a result of these lifestyle factors (sedentary lifestyle, obesity), the overall number of persons in the United States with diabetes has increased from 10 million in 1977 to 24 million in 2007 and is projected to double or triple by 2050 if current trends in diabetes prevalence continue.34,35 Clinical Presentation: Specific physiologic changes occur when insulin is lacking or ineffective. Normally, the blood glucose level rises after a meal. A large amount of this glucose is taken up by the liver for storage or for use by other tissues such as skeletal muscle and fat. When insulin function is impaired, the glucose in the general circulation is not taken up or removed by these tissues; thus it continues to accumulate in the blood. Because new glucose has not been “deposited” into the liver, the liver synthesizes more glucose and releases it into the general circulation, which increases the already elevated blood glucose level. Diagnosis: To be diagnosed with diabetes, a person must have fasting plasma glucose (FPG) readings of 126 mg/dL or higher on two different days. The previous cutoff, set in 1979, was 140 mg/dL. This change occurred as a result of research showing that individuals with readings as low as the mid-120s have already started developing tissue damage from diabetes. A value greater than 100 mg/dL is a risk factor for future diabetes and cardiovascular disease. It has been suggested that the term “prediabetes” is no longer used: the person either has diabetes or does not.36 The American Diabetes Association offers consumers a risk test for diabetes (http://www.diabetes.org/risk-test.jsp). All adults should take this risk test; anyone 45 or older should be tested for diabetes every 3 years. Individuals with elevated FPG values as described should be tested every 1 to 2 years. The therapist can offer at-risk clients information on increased activity and exercise as a means of lowering their risk of developing diabetes.37 Physical Complications: At presentation, the client with DM may have a variety of serious physical problems. Infection and atherosclerosis are the two primary long-term complications of this disease and are the usual causes of severe illness and death in the person with diabetes. Microvascular changes, characterized by the thickening of capillaries and damage to the basement membrane, result in diabetic nephropathy (kidney disease) and diabetic retinopathy (disease of the retina). Diabetes is the leading cause of kidney failure and new cases of blindness in the United States as of 2007.30,38 Poorly controlled DM can lead to various tissue changes that result in impaired wound healing. Decreased circulation to the skin can further delay or diminish healing. Skin eruptions called xanthomas (Fig. 11-7) may appear when high lipid levels (e.g., cholesterol and triglycerides) in the blood cause fat deposits in the skin over extensor surfaces such as the elbows, knees, back of the head and neck, and heels. Yellow patches on the eyelids are another sign of hyperlipidemia. Medical referral is required to normalize lipid levels.
Screening for Endocrine and Metabolic Disease
Associated Neuromuscular And Musculoskeletal Signs And Symptoms
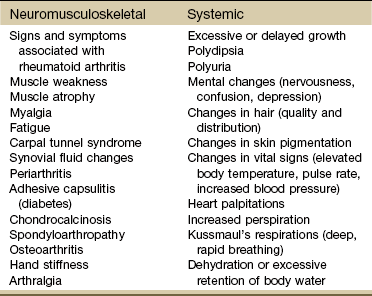
Bilateral Carpal Tunnel Syndrome
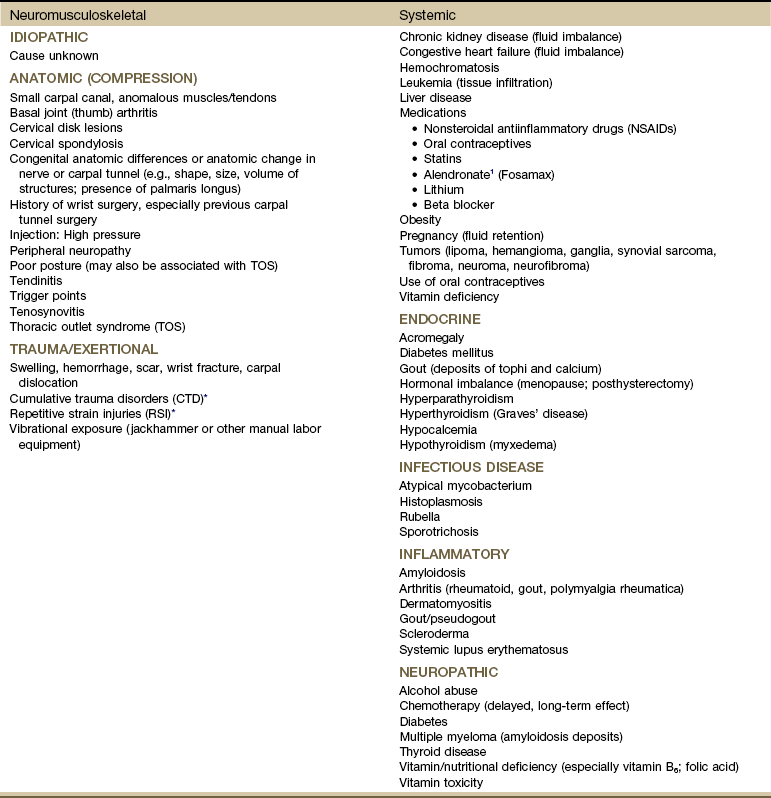
Chondrocalcinosis
Endocrine Pathophysiology
Pituitary Gland
Syndrome of Inappropriate Secretion of Antidiuretic Hormone
Acromegaly
Adrenal Glands
Adrenal Insufficiency
Cushing’s Syndrome
Thyroid Gland
Thyroiditis
Hyperthyroidism
Hypothyroidism
Neoplasms
Parathyroid Glands
Hyperparathyroidism

Hypoparathyroidism
Pancreas
Diabetes Mellitus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree