CHAPTER 115 Sacroiliac Joint Rehabilitation and Manipulation
INTRODUCTION
The path taken to diagnose sacroiliac joint (SIJ) pain may not be a straight or clearly marked one. Although several studies point to a battery of tests for diagnosing SIJ problems, a standardized protocol has yet to be devised. As a result, the treatment of SIJ pain can be difficult. Similar to many musculoskeletal problems, treatment success with SIJ pain is often varied due to cofactors surrounding each patient. Accordingly, one uniform approach is not likely. Instead, a combination of treatment options that can be applied to varied patient classifications will be more effective. A sacroiliac joint belt with manual therapy may be very successful in one individual and merely provoke pain in another. The treatment must be tailored to the individual. The patient’s history regarding the circumstances around when the pain began is often paramount in selecting treatment and management. For the sake of consistency in this chapter, the authors will use the term posterior pelvic pain to be inclusive of pain related to the sacroiliac joint, but not exclusive to only intra-articular pain. Posterior pelvic pain includes reference to periarticular pain including muscle, fascia, and ligaments around the sacroiliac joint.
TREATMENT
Manual therapy
Manual therapies can be used separately or in combination with other pain-reducing modalities. In fact, evidence suggests that decreasing musculoskeletal pain may be one of the most important roles for manual therapy.1,2 In several studies, manual therapy has been shown to be superior to traditional modalities in reducing pain, sometimes even in the absence of change to objective variables, such as range of motion.3,4 Accordingly, the authors believe it is important to consider manual therapy as a tool to reduce pain, and to pair it with rehabilitative strategies, such as stabilization exercise, to restore function. Unfortunately, there is a paucity of studies substantiating this position; however, the authors’ collective experiences suggest that this form of treatment can be beneficial.
Therapeutic rehabilitation
There is a vast array of physical therapy approaches to treatment of posterior pelvic pain. One theory proposed by Sahrmann5,6 seeks resolution in symptoms by correcting muscle and joint dysfunction based on specific muscle(s) activation. This theory relies on conscious correction of motor patterns and avoiding activities that promote pain and/or poor movement patterns. A person treated for acute posterior pelvic pain utilizing this treatment method might be instructed to use crutches so as to not develop or enhance a poor gait pattern. In contrast, other theories of treatment develop recommendations based on gross movement patterns. An example is McKenzie’s theory of systematic treatment for spine dysfunctions.7 Treatment applied is based on specific movement patterns related to spine pathology. A spine stabilization program attempts to combine therapeutic exercises based on deficiencies in spine, abdominal, and hip muscle length and strength. This method also relies on conscious overriding of poor movement patterns. At times, deciding what is acceptable and unacceptable pain while performing exercises in the latter two treatment groups can be difficult for the patient. Another theory proposed by Gray8 recommends using multiple joint movement patterns to improve function but relies on unconscious retraining of movement. The movement patterns are directed either into the restrictive range of movement or away from the restriction. Movement pattern direction is determined by the patient’s pain tolerance. If moving towards the restrictive movement is too painful, applying joint motion, loading, and unloading in the movement pattern and plane tolerated is suggested. As the motion and pain improves, the direction and combination of planes of motion advances. Gray’s approach also incorporates the pelvic floor musculature, an area often omitted from traditional programs. The pelvic floor and diaphragm are thought to play an important role in core or trunk stability. This theory is somewhat ahead of current research validation, but is a growing area of interest in some centers. In general, Gray’s approach to treatment focuses on developing a therapeutic exercise program to resemble the patient’s functional activity requirements.
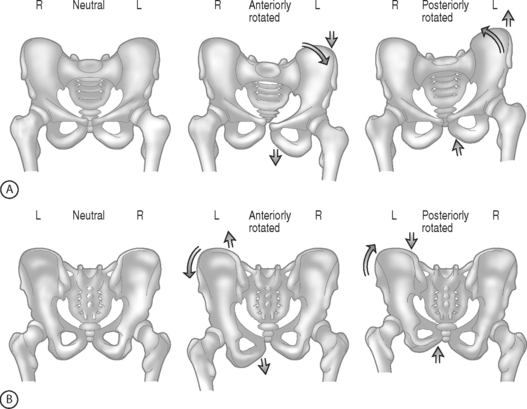
Regardless of what method or combination of methods are used, rehabilitation for posterior pelvic pain must incorporate spine, hip, and pelvic structures and mechanics. Pool-Goudzwaard et al.9 and Vleeming et al.10 have described the importance of the muscle and connective tissue network that assists in the stability of the lumbopelvis and specifically the sacroiliac joint. They have demonstrated through dissection and biomechanical modeling that there is a direct relationship between the tensioning of the dorsal sacral ligament, sacrotuberous ligament, erector spinae muscles, hamstrings, and the movement of the SIJ.11 Additionally, the iliopsoas commonly works in a shortened position. This shortened position can enhance the development of an anteriorly rotated ilium (Fig. 115.1). Hamstring strengthening cannot be accomplished until the iliopsoas is restored to activating in a biomechanically efficient length. An anterior pelvic tilt forces the hamstring to work in a lengthened position. The hamstring is a key muscle in providing stability to the sacroiliac joint because of its direct attachment and/or fascial connections to the sacrotuberous ligament. Other muscles commonly found to be working in a shortened position include the rectus femoris, tensor fascia lata, adductors, quadratus lumborum, latissimus dorsi,12 and obturator internus. Achieving appropriate muscle flexibility may take weeks to achieve. The authors advocate utilizing a stretching program that encompasses all three planes of motion. As muscle length is restored and stiffness reduced, strengthening of muscles inhibited by the biomechanical deficit can be completed. Neuromuscular re-education and facilitation techniques are helpful with this process. Closed kinetic chain strengthening should be attempted first and can then be incorporated into the lumbopelvic stabilization exercises. As trunk strengthening improves, adding multiplanar strengthening exercises will facilitate return to functional activities. Muscles commonly found to be weak include the gluteus medius, gluteus maximus, lower abdominals, and hamstrings. These are merely suggestions that are based on the authors’ experience with respect to muscle patterns of movement proposed by Janda,13,14 and Norris.15,16 As Norris points out,16 these ‘muscle imbalance categorization can usefully assist the astute practitioner, they are not cast in stone.’ Each patient presents with a unique set of circumstances with regards to pain, muscle imbalance, and joint mechanics. The healthcare practitioner must take the patient’s individual set of problems, strengths, and goals into account when creating a treatment program.
Manipulation is commonly used to treat posterior pelvic pain related to the sacroiliac joint. Manipulation is a term that may have several definitions. For the sake of discussion in this chapter it will refer to manipulation as treatment that involves manual techniques that restore joint motion. An explanation of the barrier systems utilized to direct manual therapy is useful in understanding the different approaches of manual medicine. The absolute end range of motion within any single plane of motion is referred to as the anatomic barrier (Fig. 115.2). Motion that goes beyond this barrier results in fracture, dislocation, or ligamentous or tendon tear. Within the total range of motion of any joint there are different limits to active and passive range. Active range of motion is limited by a physiological barrier. This barrier is maintained by muscle, ligament, tendon, and capsule. With passive range of motion, increased motion is obtained to the elastic barrier. Again, this barrier is maintained by the previously mentioned soft tissue structures, but at their endpoint of elasticity or length. A restrictive barrier forms as a result of a biomechanical dysfunction. This barrier reduces the active range of motion and increases the space between available active range of motion and the elastic barrier. A restrictive barrier is created by skin, fascia, long and short muscles, ligament, tendon, and joint capsules. Regardless of the specific type of manipulation used, the goal is to move the restrictive barrier back toward the elastic barrier. There are many techniques that can be used to achieve this goal. The choice of technique is examiner dependent as well as dependent on what is thought to be causing the restriction(s).
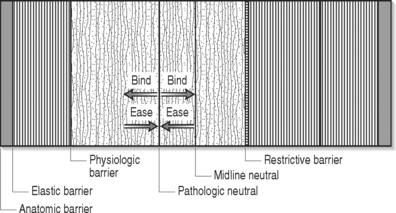
Fig. 115.2 Illustration of barriers enhances understanding of the basis of the theory of manipulation.
There are many different techniques used to manipulate a joint to restore motion. Strain–counterstrain developed by Jones,17 an osteopathic physician, is a technique where the healthcare provider palpates for tender points within the restricted area. There are many theories regarding the location and significance of trigger points. Overlap in location is noted in the trigger points identified as Travell’s myofascial trigger points,18 Chapman’s reflex points,17 and acupuncture. Strain–counterstrain utilizes any or all of these identified trigger points to assess and treat the patient. The treatment consists of the examiner monitoring the trigger point while passively positioning the patient until the pain is relieved at the trigger point. Once this position of relief is determined, it is maintained for 90 seconds. The examiner then passively repositions the patient back to a neutral position. In general, the position of comfort is found in the direction away from the restrictive barrier. Pain relief is thought to occur by reducing the inappropriate proprioceptor activity. The inappropriate strain reflex in the painful muscle is inhibited by stretching (counterstrain) the antagonist muscle. This technique is especially helpful to reduce pain related to muscle tone when more active intervention is painful.
Muscle energy techniques were first described in osteopathic medicine in the 1960s by physicians T.J. Ruddy and Fred Mitchell, Snr.19 More recently, further expansion has been made by Karel Lewitt and Vladimir Janda. The basic principle involves the healthcare provider passively placing a joint in the position away form the restrictive barrier and the patient then performs an isometric contraction against the force of the healthcare provider. After completing the contraction, the healthcare provider stretches the soft tissues to allow the joint to move through the restrictive barrier. This method of treatment applies both passive positioning and muscle activation to move through a barrier. Lewitt20 has modified this approach and termed it postisometric relaxation (PIR). Importantly, PIR emphasizes a light contraction of the muscle and does not engage the stretch reflex. The procedure is very gentle and usually very comfortable. The doctor identifies the muscle that is overactive and takes the muscle to pathological barrier of functional resistance. The doctor will then ask the patient to lightly contract the muscle being lengthened for approximately 3–5 seconds. After the light contraction, the patient is asked to relax. With relaxation the doctor lengthens the muscle to a comfortable, improved length. This is typically repeated 3–4 times.
Active release therapy (ART) is a (patented) technique used to treat soft tissue problems involving muscles, tendons, ligaments, and nerves. ART is a method of soft tissue mobilization which lengthens hypertrophied or shortened muscles, tendons, ligaments, and connective tissue.21 Preliminary studies with ART have produced encouraging results with a variety of musculoskeletal conditions.22 Once the practitioner has identified the area of tension or adhesion of tissue, a firm manual contact is applied with the thumb or finger to the area of soft tissue pathology. The practitioner will then shorten the muscle or tissues being treated. While maintaining specific opposition on the area of identified tension or fibrosis, the practitioner will ask the patient to lengthen the muscle and release and/or break up the restrictive tissue. This often promotes better inter- and intramuscular gliding and can improve muscle activation. In cases of posterior pelvic pain, ART can help restore movement for the pelvis by addressing dorsal sacral ligament, sacrotuberous ligament, and hamstrings. This may also be applied to conditions of nerve entrapment by muscles or fascia. Common entrapment sites for posterior pelvic pain include sciatic, gluteal, or lateral femoral cutaneous nerve locations.
High-velocity low-amplitude (HVLA) manipulation is the technique often associated with the term ‘manipulation.’ Evidence and international guidelines identifying the efficacy of this type of manipulation for low back pain have flourished since 1986.23–27 This type of manipulation is the form most commonly used by chiropractors. With this technique the patient is moved passively to the restrictive barrier and the examiner then applies an extrinsic force (quick thrust) to move the joint through the restrictive barrier.28 Optimally, one joint is mobilized at a time and restoration of motion at that joint is achieved. The thrust is thought to gap the joint and the gapping is thought to cause the audible pop. While the effects of thrust manipulation remain poorly understood, evidence suggests that the impact is largely a central neurological mechanism.29 Zhu et al.30 demonstrated that decreased pain response after lumbar manipulation was associated with abnormal somatosensory-evoked potentials from paraspinal patients with low back pain. Lehman and McGill,31 in their preliminary investigation, suggested that manipulation could attenuate the muscular response that directly inhibits pain. Suter et al.32 studied the effects of SIJ manipulation on the inhibitory effect of the quadriceps muscle in knee joint pathology. They showed an interaction between manipulation and inhibition of voluntary activity produced by pain.
Joint mobilization is a general term coined by physical therapy which is similar in theory to HVLA with one exception. While the goal of HVLA is to move through the restrictive barrier, joint mobilization involves applying grades of pressure to improve motion up to the restrictive barrier but not through it. Lewitt,20 a Czech neurologist, describes several approaches to this type of mobilization for the SIJ. This can include engaging the barrier of resistance and holding or rhythmically springing the barrier.
The risk surrounding HVLA for the lower back is often perceived high although it is actually relatively low. Shelkelle33 estimated the serious complication rate for lumbar manipulation at 1 in 100 million manipulations. Haldeman34 revealed that 16 of the 26 cases reported to have complications between 1911 and 1989 had been performed with anesthesia. Therefore, manipulation under anesthesia should be applied with caution.
Manipulation used for posterior pelvic pain may include any one or combination of the aforementioned techniques. Choosing which to use is usually determined by the practitioner’s skill, experience, and training. When addressing asymmetries in the pelvis, a technique using muscle activation (ART, muscle energy, contract–relax) is often helpful. Utilizing the muscle activation is helpful as the muscles around the hip and pelvis are large, powerful, and have different functions depending on positioning of the hip. Repositioning can continue until all planes of motion have been addressed. The natural follow-up to the muscle activation treatment is a muscle flexibility and strengthening home exercise program that mimics the manipulation. For example, after a muscle energy technique is applied to reverse a unilateral anterior iliac rotation, the patient should be educated how to perform an iliopsoas stretch encompassing three planes (frontal, sagittal, transverse) of motion (Fig. 115.3). The home exercise program can then facilitate maintaining the improvements made with manipulation. A HVLA treatment might be chosen when muscle activation techniques have failed to provide consistent improvement. There are several sacral thrust maneuvers (Fig. 115.4). In general, a thrust is applied to the sacrum, but is directed in the plane of restriction. The theory is that the applied force will allow a return of improved motion to the joint. Again, the home exercise program should be created to enhance the benefits of the manipulation. For example, the patient who benefits from a sacral thrust performed distally, thereby freeing a unilateral posterior iliac rotation, will likely benefit from a hamstring stretch as part of the home exercise program.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree