Sacral Fractures
Jodi Siegel
Paul Tornetta III
INTRODUCTION
Sacral fractures most commonly occur in association with a pelvic-ring disruption that can occur from high- and low-energy trauma. Most sacral fractures are stable injuries and are treated nonoperatively. Unstable sacral fractures are less common but are more challenging to treat. A small subset of these patients present with hemodynamic instability, often with other injuries, requiring a multidisciplinary approach.
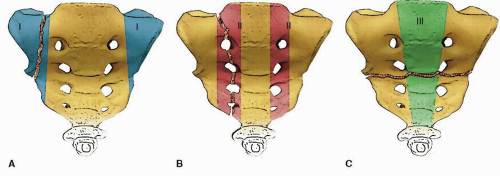
The classification of sacral fractures should start with use of one of the widely accepted classification schemes of pelvic-ring disruption. The AO/OTA, Tile, and Young and Burgess classifications of pelvic fractures attempt to describe the mechanism of injury and/or resulting instability. Sacral fractures have been sub-classified by Denis into three zones, which describe the location of the fracture in relation to the adjacent sacral foramina (Fig. 40.1). Denis Zone 3 sagittal plane injuries have been further characterized by Roy-Camille as modified by Strange-Vognsen (1), and Isler added a classification that describes injuries to the facets at the lumbosacral junction.
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
The majority of sacral fractures are inherently stable injuries and are managed nonoperatively. Impacted sacral fractures, often seen as a component of a lateral compression type 1 pelvic-ring disruption, with <20 degrees of internal rotation deformity, are stable injuries and can be treated nonoperatively with immediate weight bearing (2). Complete, nondisplaced, nonimpacted sacral fractures may also be treated nonoperatively; however, limited weight bearing with close follow-up must be employed to ensure early detection of any displacement. Patients are mobilized as soon as their overall condition allows. Pain levels are variable, and adequate pain medications are provided. The increasing numbers of insufficiency fractures seen in elderly osteopenic patients after minimal trauma are typically this fracture pattern and treated nonoperatively. A recent randomized controlled trail evaluating parathyroid hormone use in this population revealed accelerated fracture healing and improved pain scores and functional outcomes (3).
Most displaced sacral fractures that occur following higher-energy trauma are indicated for surgery. Typically, these fractures have associated injuries to the anterior pelvis, which may require treatment. Posterior pelvic-ring instability is present when there is vertical displacement of the hemipelvis, fracture displacement >1 cm, highly comminuted fracture patterns, and injuries extending into the lumbosacral articulation. Additionally, some patients with sacral fractures with disruption or displacement of the sacral foramina and neurologic dysfunction are candidates for surgery.
The determination of pelvic stability in patients with comminuted fractures without significant displacement is difficult. In these patients, two options have been recommended. One method is to perform a stress examination under anesthesia in the operating room using a push-pull technique under fluoroscopy to determine the presence or absence of instability. If substantial fracture displacement is demonstrated, surgery is typically indicated. The other method to determine stability is to mobilize the patient and obtain follow-up radiographs to assess fracture displacement (4).
PREOPERATIVE PLANNING
History and Physical Examination
Most unstable sacral fractures are the result of high-energy trauma such as motor vehicle and motorcycle crashes, falls from height, and pedestrian-motor vehicle accidents. Many patients are critically ill with associated injuries to the head, chest, and abdomen. A multidisciplinary approach using Advanced Trauma Life Support protocols is recommended.
A careful and detailed physical examination should be performed. The pelvis and lower extremities should be observed for asymmetry or deformity. The skin and soft tissues should be inspected for abrasions, contusions, or open wounds. A closed internal degloving soft-tissue injury around the pelvis, the so-called Morel-Lavallee lesion, must be identified and treated as it is associated with a 46% rate of bacterial colonization (5). Associated long-bone fractures are common but ligamentous knee injuries and subtle injuries to the ankle and foot are often overlooked.
A detailed neurovascular examination of both lower extremities—documenting the peripheral pulses as well as motor and sensory function—is essential. Patients with displaced fractures and all patients with neurologic injuries require a rectal examination. Similarly, some female patients with displaced pelvic fractures should have a gynecologic evaluation.
Imaging Studies
Radiographic evaluation includes pelvic anteroposterior (AP), inlet, and outlet views, as well as obturator and iliac oblique views (Judet). In virtually all patients with a displaced pelvic fracture, a computed tomography (CT) scan should be obtained. Modern imaging techniques allow axial and reformatted sagittal and coronal views. Correctly interpreted, these images provide a better understanding of the fracture, its deformity, soft-tissue injury, and possible treatment strategies. Additionally, sacral dysmorphism may be identified on these films, which may impact treatment. Finally, high-quality imaging can identify occult spina bifida, especially in the lower sacral segments, which may be very important when surgery is indicated. Inadvertent clamp placement for reduction can result in an iatrogenic nerve injury.
In physiologically stable patients who do not require ongoing resuscitation, no additional pelvic imaging studies are required. In hemodynamically unstable patients with continued bleeding, a clinical decision must be made regarding management. After other sources of bleeding have been excluded, two treatment methods exist for attempts to control pelvic bleeding: external stabilization combined with an exploratory laparotomy and pelvic packing or invasive angiography with potential therapeutic embolization. The optimal method of treatment remains controversial, but clinical judgment, knowledge of the institution’s resources, and understanding common injury patterns based on the pelvic imaging aid in appropriate decision making. Patients who respond to initial resuscitation, but slowly deteriorate, may benefit from CT angiography to assist with diagnosis and location of potential pelvic bleeding.
In hemodynamically unstable patients with an external rotation component to the deformity and increased pelvic volume, a sheet or pelvic binder wrapped around the pelvis at the level of the greater trochanters is part of the resuscitation. In patients going to the operating room for treatment of other injuries, the placement of a C-clamp or external fixator may be beneficial. Prior to application of an external fixator, the surgeon must
have a clear understanding of the injury and the deforming forces. Single-plane external rotation deformity can be reduced and stabilized with a pelvic C-clamp or a supra-acetabular (Hannover-pin) external fixator. Vertical displacement requires traction to reduce and stabilize the injury prior to placement of an external fixator (6).
have a clear understanding of the injury and the deforming forces. Single-plane external rotation deformity can be reduced and stabilized with a pelvic C-clamp or a supra-acetabular (Hannover-pin) external fixator. Vertical displacement requires traction to reduce and stabilize the injury prior to placement of an external fixator (6).
Once the patient is stable, the genitourinary system must be thoroughly evaluated. Because of the intimate location of the bladder to the pelvic ring, there is a relatively high incidence of bladder injuries. A urinalysis as well as a retrograde urethrogram and cystogram should be obtained in most male patients.
SURGERY
Preoperative Planning
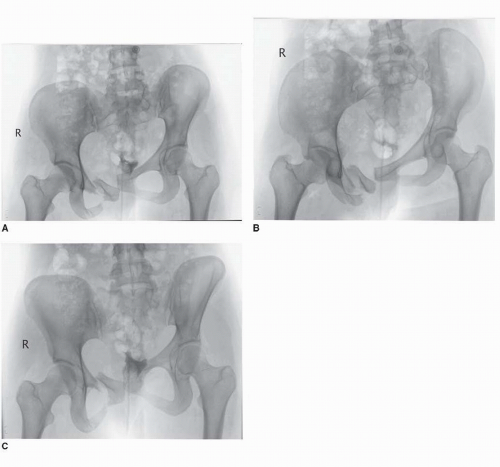
The steps necessary for reduction of most displaced unstable sacral fractures begin prior to the patient’s arrival to the operating room. A careful analysis of the preoperative radiographs and CT scan clarifies the pathologic anatomy. Posterior translation and internal and external rotation deformities can be identified on the pelvic inlet radiograph (Fig. 40.2A-C). Flexion of the hemipelvis is best seen on the pelvic outlet x-ray. When flexion occurs through the sacral fracture, the anterior pelvic ring will be displaced cephalad. This may be assessed by the heights of the ischial tuberosities. Importantly, this should be differentiated from vertical displacement of the hemipelvis as the displacement of the anterior ring is greater than the displacement of the posterior ring. When there is true vertical displacement of the hemipelvis, the amount of anterior and posterior displacement is approximately the same. Aside from lateral translation of the sacrum, most other deformities are correctable preoperatively with skeletal traction and should be confirmed with a portable AP pelvis radiograph in traction (Fig. 40.3). Initially, 15% to 20% of body weight is applied to the extremity through a distal femoral skeletal traction pin. The need for additional weight is determined by the traction radiographs. The reduction achieved preoperatively can be expected in the operating room and allows the surgeon to plan for a percutaneous procedure with the patient in the supine position or an open procedure with the patient prone.
Surgical Tactic
The anterior pelvic-ring disruption must also be addressed. A symphyseal dislocation is treated by open reduction and internal fixation through a Pfannenstiel approach first. If displaced pubic rami fractures are present instead, then surgery will typically begin posteriorly. In patients with good bone stock where a closed reduction adequately aligns the anterior pelvis, iliosacral screws alone may be the only fixation that is necessary. In patients with osteopenic bone or inadequate fixation with iliosacral screws alone, supplemental anterior fixation is usually indicated.
When the CT scan shows severe sacral comminution, some surgeons fear that iliosacral screws placed in compression may cause a neurologic injury. Also, bony fragments in the spinal canal or neural foramina may warrant an open procedure with nerve decompression. H-type or U-type sacral fractures may also benefit from open reduction and neural decompression (7). The CT scan also allows for precise evaluation of the lumbosacral junction. Injury to the L5/S1 facet joint may require stabilization with lumbopelvic fixation. In these circumstances, the patient should be positioned prone for open reduction and internal fixation of the sacrum with screws or plates.
Surgery and Surgical Approaches
The authors prefer general anesthesia with chemical paralysis. Spinal or regional anesthetic techniques are not commonly used. A Foley catheter is placed if a urologic injury is not present. Arterial lines, central venous pressure monitoring, and Swan Ganz catheters are determined on a case-by-case basis.
A first-generation cephalosporin antibiotic is given intravenously within 1 hour of surgery. If the patient has been in the ICU for a prolonged period of time, or has a positive screen for methicillin-resistant Staphylococcus aureus, vancomycin is preferred.
Patient Positioning, Prep and Drape, Imaging
The reduction obtained with traction prior to surgery can usually be obtained intraoperatively. Adjustments can be implemented under fluoroscopic control with a traction table and positioning tools.
The patient is positioned supine on a radiolucent flat-top table in traction through a distal femoral pin on the affected side (Fig. 40.4A). The patient is positioned with the injured side close to the edge of the table to facilitate drill, guidewire, and screw placement from slightly posterior to anterior. A bump is placed beneath the ipsilateral lower thorax and flank to improve the trajectory for the screws placement in the supine patient. The hip is slightly flexed, and the leg is supported with a sling. The uninjured side is attached to the table in a boot that allows the leg to remain in full extension (Fig. 40.4B). Lifting the foot off the table allows the knee to go into slight hyperextension, functioning as a countertraction post. The contralateral extremity must be rigid to allow for adjustments to the reduction without displacing the patient when traction is applied. We routinely use bilateral sequential compression devices during the procedure. A lateral padded positioner is secured to the table just below the axilla on the injured side (Fig. 40.4C). This prevents the chest and torso from moving when traction is applied. If this proximal lateral pad is not utilized, then traction on the affected side will not reduce the pelvis distally but instead will rotate it around the intact, contralateral hip joint and pull the patient’s torso toward the affected side of the table.
The C-arm is brought in from the noninjured side, opposite the surgeon. The monitor is placed at the foot of the bed so that both the surgeon and the x-ray technologist can view the images. The C-arm is positioned over the pelvis with its base perpendicular to the operating room table. The height of the table, the position of the C-arm base, and the degree of the cephalad and caudad tilt needed for perfect inlet and outlet images are determined and recorded prior to prepping and draping. Additionally, the surgeon should note if the pelvis is rotated to one side by the position of the spinous processes of the lumbar spine as seen on fluoroscopy. This should be corrected to an AP plane to ensure perfect intraoperative imaging, which is necessary to obtain perfect inlet and outlet images to evaluate the reduction and to safely place screws.
Once perfect images are obtained, the reduction is evaluated. When necessary, additional traction is applied using the fine adjustment function of the traction arm (Fig. 40.5A). A very precise reduction can usually be obtained and visualized using this controlled traction setup (Fig. 40.5B). Since the acetabulum is an anterior structure and the hip is flexed, when traction is applied to the femur, the injured hemipelvis will extend and translate distally. The force from the traction will move the hemipelvis, but the remainder of the patient does not move. The pad on the chest prevents the torso from translating laterally, toward the side of the traction; the uninjured leg cannot translate distally as it is locked in an extended position and acts as a post to pull against (Fig. 40.6A-D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree