Running
Greg Coppola
“I run to improve my perception of life.”46
—GEORGE SHEEHAN, MD
One of the basic principles of osteopathic medicine is how structure alters function. Perhaps nowhere else is this more evident than in the sport of running. When the human body is placed into motion, structural weaknesses or postural imbalances are often discovered. As the late George Sheehan wrote in a Runner’s World article entitled Detection and Correction in October 1988, running itself does not cause injuries (1). Runners are subject to a variety of somatic dysfunctions which are defined as an altered function of related components of the somatic system: skeletal, arthrodial, and myofascial structures; include also are vascular, lymphatic, and neural elements. The three classic diagnostic criteria for somatic dysfunction include asymmetry, tissue texture changes, and restricted range of motion.
The runner’s body is subjected to significant ground-reactive forces which, when coupled with improper joint movement and restricted muscular support, can lead to venous and lymphatic congestion. This cycle can affect proprioceptive input, as trophic flow is impaired and there is irritation of free nerve endings. The visceral afferent impulses bombard the dorsal root ganglion with nociceptive information. This can result in pain patterns that can keep a runner from training.
These concepts help form the framework to evaluate structure and function and apply manual medicine techniques to correct undetected deficiencies within the kinetic chain. This chapter focuses in part on how running can contribute to somatic dysfunctions and ways in which they may be effectively treated.
HISTORY
Running history credits the legendary Greek Philippides in 490 B.C. for completing the first marathon. On a hot summer’s day he ran 26 hilly miles from Marathon to Athens to deliver the news that the Athenian army defeated the Persians. Exhausted, the legend claims he died after the news reached the city. When the modern Olympic Games were inaugurated in 1896 in Greece, the legend of Philippides was revived by a 24.85 mile (40,000 meters) run from Marathon Bridge to the Olympic stadium in Athens. The first organized marathon on April 10, 1896 was especially important to the Greeks as the host nation. Twenty-five runners gathered on Marathon Bridge, and 2 hours, 58 minutes, 50 seconds later (7 minutes/11 seconds [7.11] per mile pace), the Greek postal worker Spiridon Louis finished 7 minutes ahead of the pack. The host nation was ecstatic, and the marathon was born (3).
Running has grown in popularity, and numerous running surveys point to its cost and time-efficient nature as reasons why many people choose the sport. Most clinicians agree that physical fitness is the best predictor of longevity. Individuals who run consistently have a reduced risk of cancer and cardiovascular disease, although the incidence of early arthritis and degenerative joint disease, long considered a side effect of running, is no higher than in sedentary controls.
Fields and Reece estimate that 40 to 50 million Americans run for fitness two to three times a week (4). This works out to be nearly one in seven people in the United States who are running several times a week. Recent studies indicate that 10 million people run on more than 100 days per year, and about 1 million compete in local races per year. Prospective studies reveal that 35% to 60% of runners have a significant injury each year. Running injuries are dependent on the age, experience, and size of the runners, as well as the type of running
(cross-country vs. track). There are different energy and physiologic demands, depending on the event in which the runner competes: sprints (100, 200 and 400 meters), middle distance (800 and 1,500 meters) and distance (3,000, 5,000, and 10,000 meters: a marathon) (4).
(cross-country vs. track). There are different energy and physiologic demands, depending on the event in which the runner competes: sprints (100, 200 and 400 meters), middle distance (800 and 1,500 meters) and distance (3,000, 5,000, and 10,000 meters: a marathon) (4).
TRAINING PRINCIPLES
A runner must gradually, but consistently, stress his or her body to improve performance. Training overload leads to improved performance and adaptation of the musculoskeletal system (4). However, there is a fine line between maximal training and overtraining. Runners are often subject to overuse injuries. Improper training can be linked to most running injuries. Doing too much mileage, too fast, too soon is a common part of a runner’s history. A careful review of an individual’s training log often reveals the reason for an overuse injury. Clearly, runners who run 7 days a week with too-frequent interval workouts, tempo runs, or long distance runs are at risk for overtraining injuries. Tempo runs are designed to help runners run at race pace. The benefit of specific speed workouts appears to be the physiologic changes within the cardiopulmonary and musculoskeletal systems. These changes appear secondary to circulatory and enzymatic enhancements within muscle groups along with adaptations within the nervous system. It is evident that increasing distance must be done reasonably slowly in order to prevent injuries.
A common training principle is to increase weekly mileage by no more than 10% at a time. Long runs should be no more than 30% of the cumulative weekly miles. For example, if a runner is logging 20 miles a week, long runs should not exceed 6 miles. This is a reasonable and conservative measure by which to counsel runners about training programs, although many training program abound which may vary.
Another training principle for runners returning from injury is to return at 50% of the runner’s normal training mileage at a subtempo pace (4). The severity of the runner’s injury may create a need for less mileage upon return. This is also the opportune time to discuss the use of recovery runs. Understanding how much weekly rest a runner has built into his or her schedule and how much sleep is actually needed is a significant part of evaluating and treating an injured runner.
There is a progression involved for a successful return to running and training that is designed to help the runner reach a goal. This plan involves scheduled rest days. Referring to Fields and Reece again, it has been found that runners that train 7 days a week on a regular basis are injured more than those that take intermittent rest days (4). Rest days should be part of all training plans. The recreational runner usually does not run every day, so concern about injury prevention is centered more on footwear, gait problems, chronic injury, and sudden changes in distance or terrain. For the competitive runner, these are considerations, but attention must be given to the type of workouts incorporated into the training schedule as well.
FOOTWEAR
Selecting Proper Footwear
The runner should know some general principles for the selection of appropriate footwear. This can only come from the practitioner educating the athlete on the foot type he or she possesses. The three categories of shoe type discussed are shoes for the low arch foot (pes planus), high arch foot (pes cavus), and neutral foot.
Motion control. Motion control shoes provide medial support and stability, with the purpose of decreasing excessive pronation. Strong heel counters in the shoes help to control calcaneal valgus positioning. This is important to stabilize and limit motion from heel strike to midstance, and finally to toe-off. Many motion control shoes have a straight last that gives maximum support to the foot. The sole is firm with a dual-density quality that has the most firm portion along the inner edge providing support that resists pronation (5). Motion control shoes are best for the low to flat arch (pes planus) foot.
Cushion. Cushion shoes are the opposite of motion control shoes. A shoe for the pes cavus foot needs to allow pronation, not restrict it, because at heel strike the higharched foot contacts the surface in a varus or inverted rearfoot position. Cushion shoes are designed to allow the foot to pronate, while discouraging supination. They have a medium-density outer sole, made of a soft material. This makes them less supportive allowing them to work with the foot throughout the gait cycle, not to control it (5).
Stability. These shoes are for the neutral to mild pronator. Stability shoes have a strong heel counter and a lightly curved shape (semicurved last) offering more support than cushion shoes. Stability shoes should be advised for the runner who needs the support of a motion control shoe and the shock absorbance of a cushion shoe.
Wearing the proper footwear as a runner is crucial to prevent overuse injuries. Motion control shoes are designed to support the foot and limit excessive pronation. Cushion shoes are designed to allow the shoe to work with the foot allowing more motion throughout heel strike, midstance and toe-off. A stability shoe, designed to support the neutral foot, is a balance between the cushion and motion control shoe.
Shoe Wear Patterns
Normal heel strike. The normal heel strike should be just slightly lateral of the center of the heel, 8 to 15 degrees (6). The axis considered normal for gait and wear is a line drawn lateral to the center of the heel, bisecting the sole, and slightly medial of center at the toe box. Any deviation of wear is determined to be abnormal.
Supination. This wear pattern appears on the lateral side of the heel and sole. Visual inspection of feet will determine a high-arch varus or a tibial varum heel strike.
Pronation. The wear pattern is on the medial side of the heel and sole of the shoe. Visual inspection of the shoes may demonstrate that the heel counter has shifted medially, while the front quarter has shifted laterally.
RUNNING WORKOUTS AND INJURY
A schedule for the competitive runner should be designed focusing on the specific events the runner will participate in. It is common for an elite athlete to design a cyclical schedule that incorporates not only rest days but also increases and decreases in intensity of training. This is as beneficial psychologically as much as it is physiologically. Getting into this habit is just as important for the competitive runner as it is for the elite-level runner. A healthy competitive drive exists at all levels, not just at the elite level. Because training error is the leading contributor to running injury, runners must have a healthy and safe running program that is tailored to their needs but controls and monitors total mileage (2).
The practitioner treating running injuries should be familiar with some of the standard running workouts. Additionally, a good history often provides the information necessary to determine the cause of most running injuries. Along with a complete history, a thorough examination of the entire spine and lower quarter is essential if the practitioner is to accurately determine the ultimate cause of the injury. The foot, leg, thigh, pelvis, and lumbar spine respond to isolated deviant motions often leading to a change in gait. Just as overtraining can result in tissue and joint damage, faulty mechanics can also lead to debilitating injuries.
Recreational runners are only one type of runner to consider. Competitive runners sustain injuries at a level higher than recreational runners, with total mileage being the primary factor. With regard to running injury management, the same general principles apply to both the recreational and the competitive (elite) runner.
MANUAL MEDICINE
The kinetic chain theory of running refers to how the body must absorb tremendous
ground-reactive forces throughout the musculoskeletal system. The foot and ankle mechanism is the first link in the kinetic chain. Twenty-six bones articulating at 30 synovial joints, and supported by over 100 ligaments and 30 muscles, help to dissipate these ground-reactive forces (8). If the musculoskeletal system has a structural problem, it can alter a runner’s function and can overload certain anatomic areas. A runner returning from an injury may have lingering changes in the range of motion of the previously injured site. Theoretically, this may change the biomechanics of the runner. In addition, weakness of a muscle that had prior inflammation may change its energy absorption potential and the protection that it could provide the area.
ground-reactive forces throughout the musculoskeletal system. The foot and ankle mechanism is the first link in the kinetic chain. Twenty-six bones articulating at 30 synovial joints, and supported by over 100 ligaments and 30 muscles, help to dissipate these ground-reactive forces (8). If the musculoskeletal system has a structural problem, it can alter a runner’s function and can overload certain anatomic areas. A runner returning from an injury may have lingering changes in the range of motion of the previously injured site. Theoretically, this may change the biomechanics of the runner. In addition, weakness of a muscle that had prior inflammation may change its energy absorption potential and the protection that it could provide the area.
A blocked or dysfunctional joint complex creates a need for nearby or adjacent structures to compensate for the structural problem. This altered function may be a contributing factor for a tendinitis, bursitis, or stress fracture. Most injuries are related to training errors, structural defects, or intrinsic running errors (leg-length discrepancies, excessive pronation or supination). Foot and ankle dysfunctions can lead to dysfunctions at the knee, which can alter pelvic mechanics, which in turn can affect the back and neck region. This type of musculoskeletal chain reaction is referred to as the kinetic chain theory of running.
Foot and Ankle Mechanics
Assessing and treating somatic dysfunction of the feet is an integral part of the osteopathic evaluation. These dysfunctions may occur within the forefoot, midfoot, or rearfoot, but are most common in the midfoot. In middle and long distance runners, the midtarsal bones may even sublux. Somatic dysfunction of the cuboid involves the medial edge of the bone. The cuboid moves in a plantar direction and rotates medially around its anteroposterior axis (2). Cuneiform somatic dysfunction often involves the intermediate (second) cuneiform gliding directly in a plantar direction. Navicular somatic dysfunction also involves the medial edge of the bone gliding toward the plantar surface and rotating medially around its AP axis.
The principal movements of the feet are coupled motions, which allow the feet to absorb and disperse ground-reactive forces. Ground strike occurs 750 to 2,000 times per mile for the average runner (14). Ground-reactive forces are 1.5 to 5 times body weight (7). The shear forces through the joint complexes are 50 times that of walking (7). A runner’s foot strike at a slower pace (long distance running) occurs with the calcaneus, but at higher speeds (sprinting) foot strike occurs with the forefoot.
Understanding the coupled motions of pronation and supination is important when evaluating runners. Pronation includes dorsiflexion of the subtalar and midtarsal joints, abduction of the forefoot, and calcaneal eversion of the foot. Supination includes plantarflexion at the subtalar and midtarsal joints, adduction of the forefoot, and calcaneal inversion. When these movements become excessive, they can create stress upon adjacent anatomic areas. Because structure and function are intimately related, these changes in foot structure produce effects within the musculoskeletal system at distant sites.
Initially, at rearfoot contact, the foot is in a supinated position. This is a rigid, close-packed position, which loads the tarsal bones. The foot then pronates during midstance with the tarsal joints opening up and becoming less rigid. This transition allows for better shock absorption of ground-reactive forces. Internal rotation of the tibia on the talus also occurs with pronation. The runner then progresses to toe-off, as the subtalar joint supinates and the tibia externally rotates (2).
MUSCLE IMBALANCES
Muscles absorb approximately 80% of the impact of running, with the rest of impact forces going to bone and adjacent tissues (4). One rehabilitative principle that has widespread applicability to runners is the concept of muscle imbalances. The goal of treating muscle
imbalances is the protection of the osteoarticular system. The repetitive and often excessive nature of running creates a host of musculoskeletal injuries and dysfunctions. Janda determined that muscle dysfunction is not a random occurrence but that muscles respond in characteristic patterns (9). These patterns manifest themselves in different ways, even in sports. The concept focuses on the aspect of dynamic and postural muscles (Table 37.1). Runners characteristically spend the majority of their time in hip flexion (iliopsoas) and little of the running stride in hip extension (gluteus maximus).
imbalances is the protection of the osteoarticular system. The repetitive and often excessive nature of running creates a host of musculoskeletal injuries and dysfunctions. Janda determined that muscle dysfunction is not a random occurrence but that muscles respond in characteristic patterns (9). These patterns manifest themselves in different ways, even in sports. The concept focuses on the aspect of dynamic and postural muscles (Table 37.1). Runners characteristically spend the majority of their time in hip flexion (iliopsoas) and little of the running stride in hip extension (gluteus maximus).
TABLE 37.1. APPLICATION OF JANDA’S PRINCIPLES IN THE EVALUATION AND TREATMENT OF THE LOWER QUARTER | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
As a result, a pattern of dysfunction can occur within the iliopsoas mechanism, such that the muscle becomes facilitated, hypertonic, and shortened. This physiologic change, in turn, affects its antagonist muscle group, the gluteus maximus. Therefore, the hip extensors respond by inhibition, hypotonicity, and weakness. Janda describes the weakness as a pseudoparesis, due to inhibition rather than being intrinsically weak. Once this pattern develops, it can alter the arthrokinetics of the lumbopelvic region and lower quarter. This reciprocal inhibition of the tight and dysfunctional iliopsoas affects the antagonist gluteal mechanism (9).
A runner who exhibits such imbalance will also reveal signs of a tight anterior hip capsule. The conventional modified Thomas test reveals muscle tightness of the iliopsoas, rectus femoris, and tensor fasciae latae. Hip tightness may also be detected by assessing symmetry using the pelvic rock test (see Chapter 22.2), Hip and Pelvis: Physical Examination (Fig. 22.2.9). The side of restriction can be further evaluated by placing the athlete in a prone position and observing the motion of the hip and thigh with extension. A restricted anterior hip capsule resists extension of the hip (9).
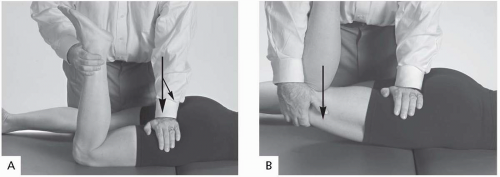
A tight anterior hip capsule can be treated with a joint play technique for anterior hip mobilization (Fig. 37.1A) or muscle energy into the hip extension barrier. In both techniques, the athlete is positioned in the same prone position, and a sequential 1/8-in. impulse is directed in a posterior to anterior glide. To do muscle energy, bring the femur into extension while the athlete gently flexes the hip against the clinician’s resistance (Fig. 37.1B).
The goal of treatment, as noted previously, is to restore reciprocal interplay between the agonist and antagonist muscles for improved shock absorption to prevent impact loading on the joint surfaces. Correcting these muscle imbalances can restore normal lines of stress across the articular surfaces. Clinical evaluations have indicated that disturbances of function within the locomotor system appear earlier than do degenerative morphologic changes. Correcting muscle imbalances reduces strain on joint capsules and ligaments.
COMMON INJURIES
Achilles Tendinitis
Achilles tendon injuries are the most common contributors to overuse injuries of the lower extremity in runners (10). These tendon injuries account for up to 5% to 18% of the total number of running injuries (10). Athletes may present with many different forms of Achilles tendon injuries, including paratenonitis, tendinosis, paratenonitis with Achilles tendinitis (tendinosis), insertional tendinitis, retrocalcaneal bursitis, Haglund’s deformity, partial ruptures, and complete ruptures (11), but in this section the focus is on Achilles tendinitis (tendinosis).
Achilles tendinitis is usually a degenerative process (tendinosis) occurring within the tendon. This common misnomer is a separate entity from the actual inflammatory process that occurs with insertional tendinitis.
Biomechanics
As with any physical activity, running greatly amplifies any and all of the demands and stresses that are placed on the body. Many studies have been devised to evaluate and quantify these forces. One such study found that the force on the Achilles tendon during running approaches that of six to eight times body weight, which approximates the maximal strength of the Achilles tendon itself. Another interesting point regarding excessive forces being applied to the Achilles tendon deals with an individual’s foot type and gait pattern. Because the tendon inserts onto the calcaneus, the tendon is exposed to stresses that occur secondary to subtalar motion (11).
Three popular hypotheses explain the occurrence of Achilles tendinitis in runners:
Hyperpronation, or pes cavus feet subjects the tendon to excessive stress that is amplified during the running motion. The normal individual makes initial foot contact or heel strike in a supinated position, followed by pronation during the midstance phase, then supination again as toe-off approaches (10). This repeated supination-pronation cycle becomes more rapid and frequent during running and produces a whipping or bowing action within the Achilles tendon (10), stressing the tendon and contributing to tendinitis.
Contradictory rotational or wringing forces applied to the Achilles tendon. During midstance, the foot normally pronates, which subsequently causes the tibia to internally rotate (11). With extension of the knee, an opposite external rotation force is applied to the tibia. Many experts now believe that this occurrence during midstance generates excessive force through the tendon (10).
Eccentric loading of the calf muscles during the normal gait cycle from impact to
propulsion. At impact, the gastrocnemius-soleus complex shortens rapidly (10) then lengthens as the tibia rotates anteriorly over the foot. The complex suddenly reshortens at the forward propulsion phase (29), and these quick muscle action alterations may cause microtears within the Achilles tendon.
Etiology
Multiple intrinsic factors are related to Achilles tendinitis, including age, sex, previous injury, aerobic fitness, body size, limb dominance, flexibility, muscle strength or imbalance, anatomic alignment, and the aforementioned foot morphology. The most common intrinsic factors are excessive rearfoot motion and gastrocnemius-soleus insufficiency. Another cause that is frequently missed is functional hallux limitus, in which the first metatarsophalangeal joint has restricted dorsiflexion. This causes a functional blockade of the gait cycle, and instead of the joint dorsiflexing fully to disperse force and motion, the next level up has to disperse more than its usual share. When the ankle makes up the difference, the Achilles tendon receives more tension and eccentric load, which can eventually lead to overload.
Prevention
As a common runner’s injury, treating Achilles tendinitis should begin with a proper training program. Prevention starts with educating the athlete about principles such as adequate stretching and warm-up, running shoe selection, custom-made orthotics to correct any malalignment in the foot, and proper training techniques. Athletes must be cautious of the too much, too soon error when beginning their training. Because the Achilles tendon has a particularly poor blood supply, especially the more distal aspects toward its insertion into the calcaneus, injuries to this segment tend to heal relatively slowly. By preventing overtraining, the chance of getting Achilles tendinitis decreases.
An important step in preventing Achilles tendinitis is correcting common training errors before an injury is sustained. Some of these errors include increasing mileage too quickly; interval training; running on sloping, hard, or slippery roads; indoor track running; and inadequate warm-up and stretching (11,12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree