Iatrogenic
Untreated combined instabilities
Missed posterolateral corner injury
Nonanatomic tunnel placement
Incorrect graft tensioning/inadequate fixation
Untreated or unrecognized meniscal or articular pathology
Biologic
Failure of graft incorporation (especially with allograft)
Soft tissue graft elongation
Traumatic
“Aggressive” early rehab before adequate biological healing
Major trauma/reinjury
Combined etiologies
Determining the timing of the failure as acute or chronic is important not only for understanding the etiology of failure but also for determining the viability of primary repair of structures versus reconstruction [19–24]. Chronicity of the treatment failure hints to the possibility of further internal derangement to the meniscus and articular surfaces. In the case of the posterolateral structures, chronicity may make revision repair impossible due to healing and excess scar formation [16–18].
Further classification of knee ligamentous injury includes precise diagnosis of which ligaments are insufficient and what associated injuries are present. This requires assessment of the cruciate ligaments, collateral ligaments, posterolateral structures, the meniscus, and articular cartilage. The two most common combined injury patterns after knee dislocations include the anterior cruciate ligament (ACL), PCL , and medial collateral ligament (MCL), and the ACL, PCL, lateral collateral ligament (LCL) , and PLC [8, 16–18, 25].
Associated injuries include damage to the patellar tendon, the iliotibial (IT) band, popliteal vascular structures and the common peroneal nerve, as well as bony avulsion fractures [26, 27]. As with all knee injuries, appropriate diagnosis and classification is based on an accurate history, thorough physical examination, and appropriate timely imaging studies [28–32].
Preoperative Evaluation
Patient History and Review of Previous Records
The preoperative evaluation for failed PCL and multiple ligament surgery begins with a thorough history. Though the history is obtained from the patient and family members, a review of the patient’s old records is essential for determining what original procedure was performed. Often patients are unreliable sources of objective information and, therefore, operative reports, clinic notes, arthroscopic photographs, and physical therapy reports all provide the revision surgeon with vital information for preoperative planning. Key information to glean from old records includes the timing of surgery, results of the examination under anesthesia, what structures were repaired or reconstructed, grafts used, the status of intraarticular structures, and the type of fixation used [16–18].
Information to be obtained directly from the patient pertains more to current symptoms, the mechanism of injury or reinjury, and the circumstances of the surgical failure [16–18, 33].The surgeon must be able to discern from the patient whether the chief complaint is knee pain or recurrent instability. This distinction alone often determines the course of treatment, with instability more often requiring surgical treatment and pain alone indicating conservative management. Finally, smoking history and the level of patient compliance should be addressed in order to understand the factors related to treatment failure. While the patient is often the best source for describing the circumstances of injury, postoperative level of compliance may be best sought from clinic notes and physical therapy reports.
Physical Examination
Once the patient’s chief complaint and the circumstances of treatment failure have been established from history and review of records, a thorough physical examination of both lower extremities in their entirety should be performed [16–18]. Examination findings are often time dependent. Key physical examination findings to evaluate are listed in Table 20.2. In the initial portion of the evaluation, the examiner should pay close attention to gait pattern, varus thrust, the soft tissue envelope, atrophy of the quadriceps musculature, the presence or absence of an effusion, ability to perform an active straight leg raise, neurovascular status, and active and passive range of motion [16–18, 27, 34–38]. More focused evaluation of the knee joint should include a detailed assessment of the patellofemoral joint for crepitation, tenderness to palpation, and the integrity of the medial patellofemoral ligament . Not uncommonly an associated patellofemoral subluxation or dislocation may occur with a tibiofemoral dislocation. Medial and lateral patellar glide as well of patellar tilt and lateral apprehension testing helps to determine the status of the medial checkrein structures [16–18].
Table 20.2
Key physical examination tests for the failed PCL and multiple ligament reconstructed knee
Global |
Gait pattern |
Varus thrust |
Quadriceps atrophy |
Soft tissue injury |
Previous incisions |
Neurovascular status |
Active straight leg raise |
Active and passive range of motion |
Patellofemoral joint |
Medial and lateral patellar glide |
Passive patellar tilt |
Crepitation with range of motion |
Medial and lateral facet tenderness |
Lateral patellar apprehension |
Meniscus |
Joint line tenderness |
McMurray’s test |
Ligamentous laxity examination |
Lachman |
Anterior drawer (internal, neutral, and external rotation) |
Posterior drawer (internal, neutral, and external rotation) |
Pivot shift (reverse and internal) |
Posterolateral rotatory instability (30° and 90° of flexion) |
Varus and valgus stress (0° and 30° of flexion) |
Joint line tenderness as well as the flexion McMurray’s test is utilized to assess the status of the meniscus medially and laterally. Ligamentous laxity patterns are then evaluated using the Lachman, anterior and posterior drawer, pivot shift, quadriceps active, varus and valgus stress, and posterolateral rotator instability tests [16–18, 39, 40]. Anterior and posterior drawer tests should be performed in internal rotation, neutral, and external rotation. Varus and valgus stress tests should be performed in 0° and 30° of flexion, and posterolateral rotatory instability (PLRI) tests in 30° and 90° of flexion. Keep in mind that there are two laxity patterns involved with a PLC injury: varus (LCL ) and rotation (PLC). They may occur separately or in combination [41]. These tests should be meticulously performed and graded, then compared to the uninjured limb to determine asymmetry.
Preoperative Imaging: Radiographs, MRI , and Vascular Studies
Complete and appropriate imaging studies serve as a road map for revision PCL and multiple ligament knee surgery. In addition to the bones and soft tissue structures, imaging should also be used to evaluate arterial and venous structures prior to revision surgery [16–18].
Radiographs
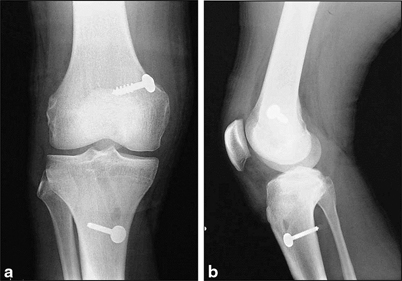
For all failed knee ligament reconstruction patients, standard knee series X-rays should be obtained and ideally compared with the patient’s original preoperative X-rays. In the senior author’s practice, all patients receive a standing bilateral 45° posterior-anterior (PA) flexion X-ray, a bilateral 30° merchant view X-ray, bilateral lateral views, and a standing bilateral long cassette image. Important information to be ascertained from this imaging series includes: (1) patella height, (2) tunnel position and size, (3) degree of tibiofemoral subluxation, (4) mechanical and anatomic axes, (5) position of retained hardware, and (6) associated fractures and osteopenia. Stress radiograph s may also be helpful to determine the presence of fixed subluxation. Figure 20.1 shows the preoperative bilateral AP radiographs after a failed PCL reconstruction .
MRI
A recent magnetic resonance imaging (MRI) should be obtained to evaluate the soft tissue structures prior to revision surgery. It should be born in mind, however, that postsurgical changes may confuse the injury pattern picture. All imaging series should be scrutinized by the surgeon and an experienced musculoskeletal radiologist to determine new injury from postsurgical changes. Care should be taken to evaluate all ligamentous structures, the patellar tendon, medial and lateral menisci, the articular cartilage, and posterolateral structures [16, 18, 19, 42, 43].
MRI can also be used to evaluate the arterial anatomy at the posterior knee. Revision surgery is significantly more risky with proximity of the popliteal artery due to scarring or variant anatomy of the vasculature. An aberrant anterior tibial artery which runs anterior to the popliteus muscle and adjacent to the posterior capsule and tibial cortex occurs in 2.1 % of extremities [44]. Recognition of the presence of this anatomical variant is important to decrease the risk of injury during tibial tunnel drilling and proximal tibial osteotomy when necessary.
Arteriogram/CT Angiogram
Though often more pertinent in the acute setting after knee dislocation and prior to primary reconstruction, an arteriogram or a computed tomography (CT) angiogram of the lower extremity should be obtained in any patient with suspected vascular injury [16–18, 27, 45]. Spasm, intimal injury, or complete tear may all alter vascular status to the injured limb and must be thoroughly evaluated prior to revision surgery [46–50]. It is strongly recommended that when there is any doubt regarding the vascular status of the extremity, a preoperative arteriogram should be obtained [16–18, 50–52]. Figure 20.2 demonstrates a preoperative arteriogram in a patient with popliteal artery occlusion after a knee dislocation.


Fig. 20.2
Preoperative arteriogram demonstrating a popliteal arterial injury. (With permission from Ref. [62], Fig 21.2)
Venous Duplex Doppler Ultrasound
All patients with combined ligamentous injuries and failed reconstructions should undergo a venous duplex Doppler ultrasound to rule out deep vein thrombosis (DVT). Given the decreased ambulatory status and limited range of motion of the traumatized knee, patients with MLI are predisposed to clot formation [16–18]. It is recommended that bilateral Doppler ultrasounds be obtained after the initial office visit and 1 day prior to revision surgery.
Patient Counseling
Discussions with patients prior to revision posterior cruciate and multiple ligament reconstructions should stress the importance of realistic expectations. Functional needs for activities of daily living and occupational requirements should take precedence over return to sporting activities. The lengthy recovery time, rehab commitment, and increased risk of complications after revision knee ligament surgery should be thoroughly understood by the patient and family members before proceeding to surgery. Degenerative changes to the joint are likely no matter how great the technical ability of the surgeon. It should be further stressed that the use of tobacco products may further delay or inhibit the patient’s healing ability postoperatively, and efforts should be made to discontinue tobacco use.
Revision PCL and Multiple Knee Ligament Surgery
Indications and Contraindications
Indications for revision PCL or multiple ligament reconstructions include a patient with a previous failed PCL or MLI reconstruction and continued symptoms of instability with or without pain. As previously noted, a thorough preoperative assessment of combined instabilities and associated injuries should be performed. Concomitant injuries should be addressed along with the revision reconstruction [53]. Contraindications to revision reconstruction include severe loss of range of motion, fixed posterior subluxation, advanced osteoarthritis, and active infection.
Preoperative Planning
Timing of Surgery
The appropriate timing of revision PCL and multiple knee ligament surgery is dependent on multiple factors. Key elements in determining ideal timing of surgery include patient-related factors, equipment availability, and qualified personnel. Patient-related factors affecting surgical timing pertain to the general health of the patient, availability of patient assistance after hospital discharge, and the presence of active infection. Available equipment must include desired allografts, necessary fixation devices, and intraoperative fluoroscopy [16–18, 26, 40]. Qualified personnel necessary for successful revision reconstruction includes an experienced knee surgeon, familiar operating room staff, and occasionally a vascular surgeon on standby. The procedure should be performed as the first and/or only case of the day when the reconstructive surgeon is well rested. Plans should be in place for the patient to be admitted to an inpatient orthopedic ward or ICU for the first 24 h postoperatively.
Graft Selection
Graft selection is dependent on autograft or allograft availability, previously used graft type, surgeon experience, and surgeon preference. In the revision situation, it is prudent to consider allograft reconstruction particularly for MLI cases. This is done in order to limit the amount of soft tissue disruption inflicted on an already traumatized soft tissue envelope. If autograft reconstruction is chosen, it is crucial to be aware of the type of any previously used autograft to assure intraoperative availability of the graft. Review of previous operative notes is essential for assuring graft availability and operative efficiency.
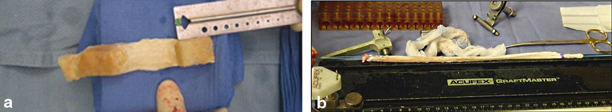
Autograft tissue may be harvested from the ipsilateral or contralateral extremity and has the advantage of better graft incorporation and remodeling [16–18]. At our institution, Achilles tendon and Tibialias Anterior allografts have been traditionally favored for revision reconstructions [1]. In recent years, quadriceps tendon autograft with a patellar bone plug has gained favor for younger patients. The advantages of using allograft tissue include: decreased operative time and no donor site morbidity [16–18, 54, 55]. Risks of allograft usage include an increase in cost, delay in incorporation, elongation of the soft tissue portion, and potential disease transmission [55]. Figure 20.3 illustrates commonly used allograft options.
Previous Skin Incisions
Prior to undertaking revision knee ligament surgery, all previously used skin incisions should be known and marked with an indelible marker. When practical, previous incisions should be utilized to avoid further disruption to the soft tissue envelope. Patients should be aware, however, that previous incision may need to be extended for adequate visualization and separate incisions may be necessary. Ideally, a discussion of incisions should be carried out with the patient in the clinic and expected incisions should be drawn and demonstrated to the patient.
Diagnostic Arthroscopy and Staged Procedures
In the case of malpositioned or overly dilated bone tunnels, bone grafting and staging of revision reconstruction may be necessary [16–18]. Most modern digital imaging programs include a ruler tool allowing for more accurate measurement of tunnel width. Preoperative radiographs should be scrutinized and tunnel widths noted. These results should then be compared with operative notes from the primary surgery to determine the presence of tunnel dilation. Preparations should be made for harvesting bone graft or inserting prepackaged allograft bone dowels if poor bone stock or malpositioned tunnels are present. Regardless of the results of preoperative X-rays, a diagnostic arthroscopy should be performed to determine the need for staged revision prior to proceeding with graft harvest. If excessive tunnel widening or reabsorption is encountered, previous fixation hardware should be removed, the tunnels grafted, and adequate time allowed for healing and incorporation (usually 6 months) [16–18].
Intraoperative Fluoroscopy
Intraoperative fluoroscopy has become an invaluable tool in primary as well as revision knee ligament reconstruction. The utility of readily available fluoroscopy lies in the ability to place precise anatomic tunnels in the femur and tibia and prevent the potential complication of tunnel convergence. Not only is fluoroscopy useful for guide pin and tunnel placement but also it helps the surgeon to perform a more accurate preoperative examination under anesthesia [16–18]. With fluoroscopic examination under anesthesia, real-time evaluation can be made of ligamentous laxity. This is especially useful in evaluating fixed posterior tibial translation with PCL injuries [16–18]. Figure 20.4 shows an intraoperative lateral fluoroscopic knee X-ray with a PCL tibial tunnel guide positioned for guide pin placement.
Surgical Technique (Section Adapted and Modified from Ref. [63], Chaps. 47 and 49)
Anesthesia
The choice of anesthesia is made in conjunction with the surgeon, the anesthesiologist, and the patient. The anesthesia team typically chooses between a general anesthesia or an epidural anesthetic with intravenous sedation. If the anesthesiologist is at all concerned regarding airway management, general anesthesia is performed. At our institution, preoperative femoral and sciatic nerve blocks are routinely used. The nerve blocks not only provide anesthesia for the surgical procedure but also provide up to 12 h of postoperative pain relief. A Foley catheter is placed for monitoring fluid status, and a vascular surgeon is on call in case a vascular injury occurs during the procedure.
Patient Positioning
The patient is placed in the supine position on a flat top table with the patient’s heels at the end of the operative table. No well-leg holder, or tourniquet, is used for the procedure. A foot post is secured to the operative table to maintain the knee in a 90° flexed position. A side post is secured to the table at the level of the lesser trochanter, and a soft bump is placed under the hip of the injured limb. Alternatively, a well-padded arthroscopic leg holder can be used to hold the leg. Figure 20.5 demonstrates the senior author’s operative setup for limb positioning and available fluoroscopic imaging. All limbs are well padded for the procedure, particularly the uninjured lower extremity.


Fig. 20.5
Operating room limb positioning with arthroscopic leg holder and available fluoroscopy seen in the background
Examination under Anesthesia
After successful induction of anesthesia in the operating room, a thorough examination under anesthesia is performed and correlated with clinical assessment and imaging findings. It is of utmost importance to examine the uninjured extremity and use it as a reference. Passive range of motion is first tested noting any deficits or asymmetry to the uninjured limb. The anterior drawer, Lachman, and pivot shift tests are then performed to evaluate the ACL.
Posterior tibial sag and translation with posterior drawer testing are then used to evaluate the PCL . The knee is then placed into the figure-four position, and the LCL is palpated with a bowstring test. Varus and valgus stress is then applied to the knee in 0° and 30° of flexion to evaluate the LCL and MCL, respectively. PLC structures are then evaluated by applying an external rotation force to the proximal tibia and fibula at 30° and 90° of flexion with the proximal tibia held in a reduced position. Degree of external rotation is then referenced with the uninjured limb. Greater than a 15° increase in external rotation is an indication of PLC injury.
Surface Landmarks and Skin Incisions
An indelible marker is used to identify the surface anatomy and the incisions that will be utilized during the procedure. The osseous landmarks including the inferior pole of the patella, the tibial tubercle, Gerdy’s tubercle, and the fibular head are identified and marked. The peroneal nerve is then palpated and marked superficial to the fibular neck. The medial and lateral joint lines are then identified. All previous and potential skin incisions are then marked. The anterolateral arthroscopy portal is placed adjacent to the lateral border of the patella above the joint line. The anteromedial arthroscopy portal is placed approximately 1 cm medial to the patellar tendon at the same level. A superolateral outflow portal is placed 1 cm proximal to the superior pole of the patella and posterior to the quadriceps tendon.
A longitudinal 3-cm incision originating 2 cm distal to the joint line and 2 cm medial to the tibial tubercle is drawn on the anteromedial proximal tibia for the ACL and PCL tibial tunnels. A 2-cm incision is placed just medial to the medial trochlea articular surface and along the subvastus interval for the PCL femoral tunnel. The incision for the lateral and posterolateral structures is a curvilinear 12-cm incision that is drawn midway between Gerdy’s tubercle and the fibular head. It is traced proximal to the lateral femoral epicondyle while the knee is in 90° of flexion [16–18]. If a medial injury is present, the distal incision for the tibial tunnels is traced proximally to the medial epicondyle in a curvilinear fashion.
Diagnostic Arthroscopy /Intra-Articular Evaluation
An arthroscopic approach is advocated to assist in the planning of potential skin incisions needed for the procedure based on the pattern of injury. Gravity inflow or dry arthroscopy is recommended for the prevention of iatrogenic compartment syndrome. If inflow is used, the posterior leg musculature should be palpated intermittently to assess for developing compartment syndrome. If excess fluid extravasation is noted, then the arthroscopic technique should be abandoned in favor of an open approach.
All compartments within the knee are assessed. The MCL and the meniscal attachment to the deep MCL are assessed to determine if tibial-sided injury is present. In the lateral compartment, the popliteus tendon is visualized and probed to discern if its function has been compromised. Both cruciate ligaments should be evaluated at their femoral and tibial insertion sites along with both menisci and the articular cartilage. If intra-articular pathology is present, any concomitant articular cartilage or meniscal injury must be addressed. Every effort should be made to preserve as much meniscus tissue as possible. Peripheral meniscus tears are repaired with an inside-out technique while irreparable tears may be debrided. If inside-out repair is performed, the sutures should be tied directly onto the joint capsule at 30° of flexion.
The necessary debridement of the joint is performed with a 4.5-mm arthroscopic shaver and basket forceps. This includes debridement of the notch while preserving any remaining intact PCL tissue. The tibial insertion site of the PCL is removed by inserting a shaver or a curette through a posteromedial portal and developing a plane between the PCL and the posterior capsule. Every attempt is made to debride the tibial insertion of the PCL to help with eventual placement of the guide wire for the tibial tunnel. In the senior author’s practice, a limited notchplasty is performed. The fat pad should be preserved if at all possible to prevent patellar fat pad entrapment syndrome.
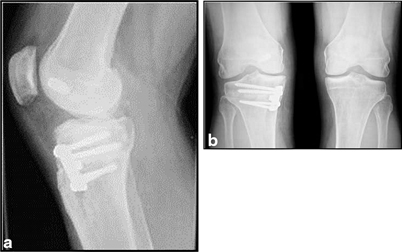
Biplanar Opening Wedge High Tibial Osteotomy
When performing a high tibial osteotomy, preoperative templating using standing long cassette radiographs is essential. The planned osteotomy should be drawn, and an estimate of the proximal tibial width and necessary plate size should be made. The width of the opening wedge osteotomy on the tibia is determined by the degree of desired correction.
The patient is placed in the supine position as described above. An incision is made midway between the tibial tubercle and the posterior border of the tibia. This incision begins 1 cm inferior to the joint line and extends approximately 5 cm distally. Exposure is made down to the superficial fibers of the MCL. Subcutaneous flaps are created to allow exposure of the patellar tendon and the tibial tubercle. The patellar tendon is retracted laterally. An incision is then made in the sartorius fascia just superior to the gracilis tendon, and a subperiosteal dissection is carried out superiorly to release the superficial fibers of the MCL off of bone. Care must be taken to prevent violating the fibers of the MCL.
A tibial guide wire is placed from an anteromedial to a posterolateral direction angled 15° cephalad along the proposed osteotomy, and its position is confirmed with fluoroscopy. The line of osteotomy should be just superior to the tibial tubercle. The width of the proximal tibia should then be confirmed using a free Kirschner (K)-wire to confirm that the actual tibial width at the osteotomy site matches the template tibial width on preoperative radiographs. This allows confirmation of an adequate tibial osteotomy correction. A 1-in. osteotome is used to begin the osteotomy, using the K-wire as the directional guide. Once the osteotomy plane is established, the K-wire may be removed and the osteotomy completed with an oscillating saw or osteotome. Care must be taken to protect the lateral hinge of cortical bone. To safely complete the osteotomy across the posterior tibial cortex and protect the neurovascular structures, the osteotome must be angled to avoid excess perforation of the posterior cortex.
An opening wedge osteotomy system with a wedge device is then inserted into the osteotomy site to create the desired angle of correction. The appropriate plate is then selected and placed in the anteromedial aspect to the osteotomy for a biplanar effect. The alignment of the leg is again checked using the Bovie cord and fluoroscopy with the cord recreating the mechanical axis of the knee joint. The axis should cross lateral to the tibial spine. The plate is then secured in place with two cancellous screws proximally that are directed parallel to the joint line. The plate is fixed distally with 4.5 mm screws with purchase into the lateral tibial cortex. Wedge cuts of bone graft are then inserted into the osteotomy site. The superficial MCL is then repaired to the medial proximal tibial metaphysis with suture anchors. Figure 20.6 shows the AP and lateral X-rays after a biplanar osteotomy and plate fixation with PCL reconstruction.