Revision Requiring Osseous Augmentation
Bernard F. Morrey
Mark Morrey
Joaquin Sanchez-Sotelo
INTRODUCTION
There are three categories of the procedures that the authors consider to be bone augmentation in nature: cortical strut graft, cancellous impaction grafting, and allograft prosthetic composite. As might be expected, there is some overlap in the use of these options such as electing to perform impaction grafting versus type I allograft prosthetic composite for extensive expansion of the cortex. The important point is that there are several, reliable options and selection is based on surgeon experience and specific pathologic features. Hence, the authors employ all three options.
Revision for marked osseous deficiency is always a challenge and often requires a complex solution. It therefore goes without saying that preoperative assessment is critical and, of course, individualized. Details regarding presentation and assessment expectation are discussed in detail elsewhere (1). In keeping with the theme of Master Technique series, we detail the surgical technique.
SURGICAL OPTIONS
There are three bone augmentation procedures:
Strut Graft
Cancellous Impaction Grafting
Allograft Prosthetic Composite
A. STRUT GRAFT AUGMENTATION
Allograft cortical struts are used extensively, occasionally for primary conditions, but most often as a reoperation. The most common indication is for periprosthetic fracture.
INDICATIONS/CONTRAINDICATIONS
Indications
In general,
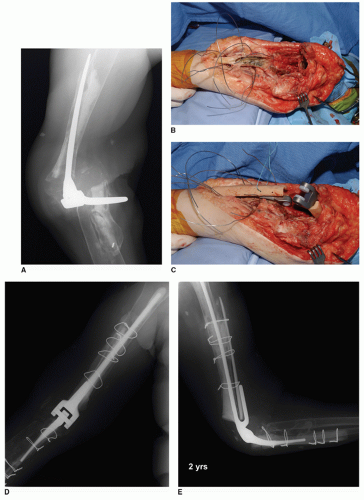
To augment and reinforce the strength of the host bone (Fig. 39A-1)
To address osseous length deficiency (Fig. 39A-2)
To avoid a stress riser or area of weakness (Fig. 39A-3)
To treat periprosthetic fracture (Fig. 39A-4)
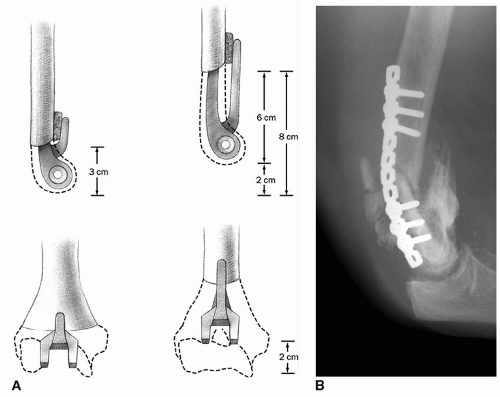
 FIGURE 39A-1 Two conceptual indications for strut graft (A) to supplement for length deficiency; (B) to reinforce areas of potential stress riser or weakness. |
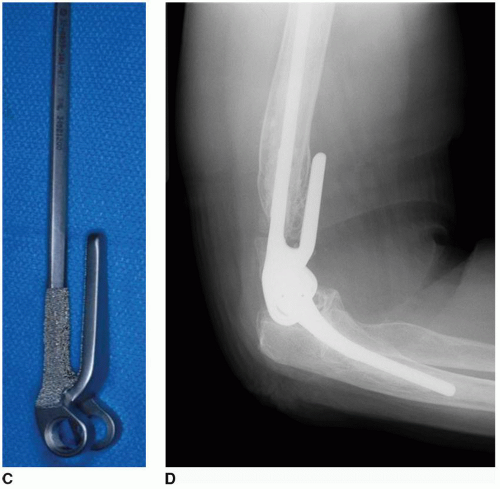 FIGURE 39A-2 (Continued) C: A long flanged Coonrad-Morrey implant was employed. D: At 3 years, the graft has incorporated and the bone-cement interface is stable. MEPS score was 92. |
Contraindications
Application to nonviable host bone
Excessive and unsupported length of the cortical strut graft
Relative Contraindication
Presence of active or low-grade sepsis
Note: The strut has been observed to heal in the presence of sepsis; however, if there is a known infection, the procedure should be staged. Resolve the infection first, and then deal with the underlying problem requiring revision with the strut.
SURGICAL TECHNIQUE: STRUT GRAFT
Position
The patient is supine on the table with the arm brought across the chest. For periprosthetic fracture in the proximal half of the humerus, an anterolateral exposure may be required. In this instance, the patient is prepped and draped as if a shoulder procedure is to be performed so as to allow the anterolateral adjunctive exposure (Fig. 39A-5). An Esmarch tourniquet is employed in such instances.
Surgical Incision and the Ulnar Nerve
This is dictated by the specific pathology and goals of treatment. In general, the previous surgical incision is reentered and the ulnar nerve is identified. If asymptomatic, it is simply identified and avoided. If the ulnar nerve is symptomatic, it is decompressed. For periprosthetic fracture, the articulation need not be exposed or addressed. However, if the implant has been in use for more than 5 years, it is wise to replace the bushings if this does not add significant time or risk to the procedure.
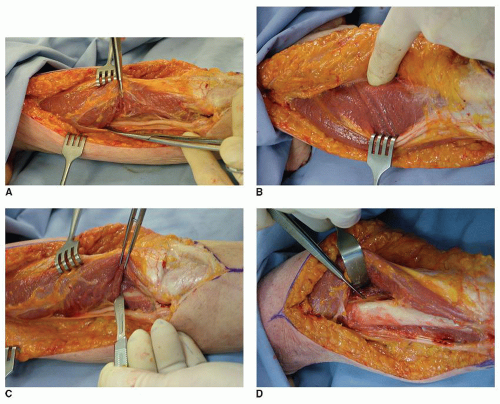
Exposure
The key is to adequately expose the field of graft application. This is not an issue for the ulna but is a major challenge for humeral strut application. In all instances, one must identify the radial nerve. The nerve is palpated and is isolated and protected. In some instances, it may be most convenient to elevate the triceps from the posterior medial humerus to the lateral intermuscular septum. The lateral intramuscular septum is released from the humerus, and the radial nerve is mobilized anteriorly with the muscular sleeve (Fig. 39A-6).
Periprosthetic Fracture
If the implant is loose, the component is removed and the fragments are prepared, usually with serial reamers through the fracture site.
Note: Special care is taken through all these steps to prevent injury to the radial nerve.
The goal is to bypass the fracture with a longer stem. The longer stem trial facilitates reduction.
If the bone is very osteoporotic, the authors prefer two struts placed approximately 180 degrees opposite each other.
Note: Care is taken not to allow the two struts to be applied to the same anatomic level. This avoids a potential stress riser that can occur from such a circumstance.
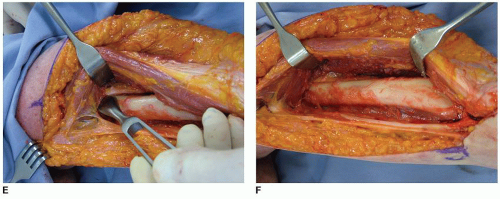
Strut Selection and Preparation
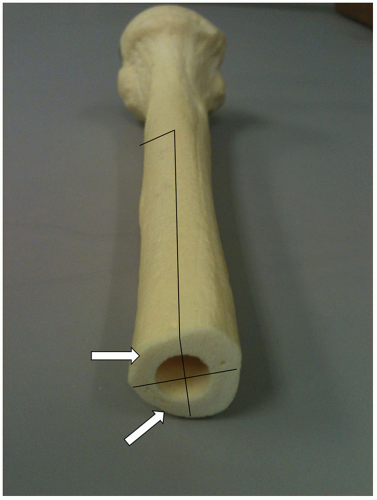
Ideally, struts are harvested from an allograft of the bone being treated. For maximum contact and structural stability, for the humerus, the struts should be slightly curved so as to follow the curvature of the host bone. The ideal strut constitutes about 90% of the bone circumference (Fig. 39A-7).
This provides markedly improved surface contact area and offers improved resistance to bending and torsion forces. Such a strut also allows plenty of exposed surface for soft tissue attachment to the host bone. The struts are NOT applied with cables but with monofilament wires. We prefer the Luque wires for their strength and the effective technique by which they can be applied.
This provides markedly improved surface contact area and offers improved resistance to bending and torsion forces. Such a strut also allows plenty of exposed surface for soft tissue attachment to the host bone. The struts are NOT applied with cables but with monofilament wires. We prefer the Luque wires for their strength and the effective technique by which they can be applied.
Note: It is important to perform a trial reduction prior to securing the struts. Struts are applied, and they are loosely tightened so that the proper orientation of the fracture has been defined.
Implant Reinsertion
The medullary canal is cleaned and dried, and polymethylmethacrylate (PMMA) is injected down the canal.
Efforts are made to plug the canal if possible to improve the bone-cement interface.
Note: The cement should be pressurized distal to the fracture line, but not across the length of the facture. Extruded cement will prevent osseous union.
Once the cement has been inserted and the proper anatomic orientation of the implant has been defined, the excess cement is removed from the fracture line as much as possible.
The struts are then firmly secured, while the cement is polymerizing.
A summary of the principles of strut grafting is shown in Table 39A-1 and illustrated in Figure 39A-8.
TABLE 39A-1 Principles of Strut Grafting | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
RESULTS
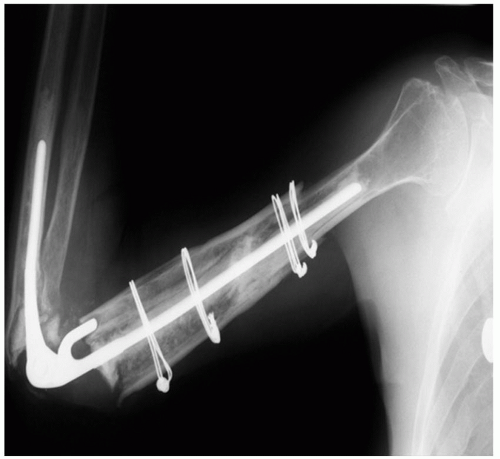
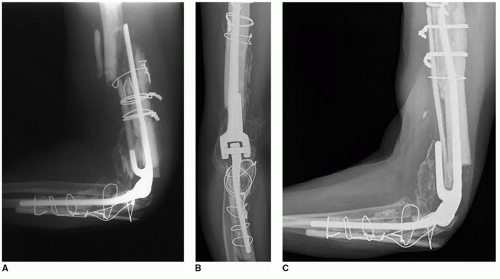
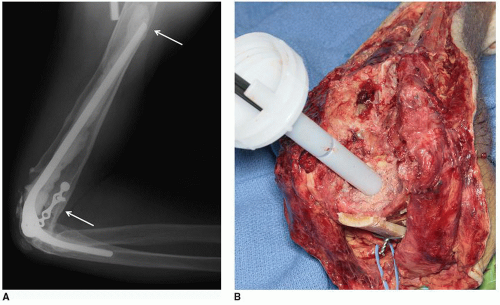
Strut graft incorporation is reliable and occurs in about 90% at the femur (2). We have documented an incorporation in 10 of 11 instances of treatment for periprosthetic fracture of the humerus (3) (Fig. 39A-9). An identical incorporation rate was reported after 22 instances of use at the ulna, for various indications (4) (Fig. 39A-10). Hence, this is a reliable and very useful technique when applied to the elbow.
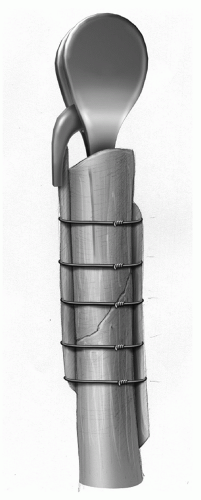
B. IMPACTION GRAFTING
Rationale: The effectiveness of cancellous impaction grafting is well documented in the orthopedic literature (5). The key concept is to create a very firmly applied cancellous bone substrate to mechanically substitute and support instances in which the osseous envelope has been expanded and compromised. Originally developed for the acetabulum by Slooff (6), the senior author has employed this technique for revision at the acetabulum, femur, ulna, and humerus.
INDICATIONS/CONTRAINDICATIONS
Indications
Expanded cortical envelope with loss of structural integrity is inadequate to accept cement or a prosthetic component (Fig. 39B-1).
Contraindications
Active infection
The inability to bypass the defect with the stem of the implant
Loss of structural integrity, making firm impaction impossible
PREOPERATIVE PLANNING
Assessment
The key is to assess the bone to be treated to assure it is suitable for this type of treatment based on the above characteristics.
SURGICAL TECHNIQUE
Preparation
Once the pathology has been exposed, several assessments are essential. The first step is to assure adequate circumferential integrity of the recipient bone. If adequate, the membrane from the prior implant is completely removed.
The host medullary canal is identified, and a trial implant is placed through the expanded bone into the more normal host bone. It is critical to determine the depth of insertion. The trial is articulated with the ulna, the elbow is flexed 90 degrees, and the position of the trial implant is determined (Fig. 39B-2). This approximates the proper depth of insertion of the humeral component.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree